Combined Iliac Stent with Femoral Endarterectomy
Richard J. Powell
Endarterectomy with patch angioplasty is the standard for treatment of isolated common femoral artery (CFA) occlusive disease. The management of disease that extends proximally into the external iliac arteries is a more challenging problem. According to the modified guidelines from the Trans-Atlantic Society Consensus (TASC II) document, external iliac disease involving the CFA is classified as either TASC C or D depending on the extent of iliac involvement. For TASC D lesions, open surgical bypass remains the recommended treatment with consideration of endovascular options only for TASC C lesions in poor-risk patients. Standard open surgical therapies include iliofemoral endarterectomy or aortofemoral bypass. While durable, these options are associated with increased perioperative morbidity. Less invasive but also less durable open surgical options include axillobifemoral bypass or femoral–femoral bypass for unilateral disease. In the endovascular era, endoluminal treatment has been shown in certain situations to be a comparable option for iliac occlusive disease.
Indications for the combined femoral endarterectomy and iliac stent or stent graft placement include:
Disabling claudication
Critical limb ischemia
As an inflow adjunct to femoral–femoral or infrainguinal bypass grafting
There are several potential limitations with this technique which include:
The need to cover the internal iliac artey
We do not routinely cover the hypogastric artery in treating common or external iliac lesions. The fate of a crossed hypogastric artery for treatment of adjacent disease is unknown and may eventually exacerbate or contribute to pelvic ischemia. If the decision that covering the hypogastric artery is warranted we attempt to do with a bare metal self-expanding stent.
In addition, the inability to cross long total occlusions is a potential obstacle for successful utilization of this technique. This has largely been overcome by increased use of reentry devices.
The presence of concomitant severe aortic occlusive disease including the presence of shaggy thrombus within the infrarenal aorta.
Presence of common iliac or aortic aneurysm is a relative contraindication.
All patients undergo preoperative peripheral vascular evaluation with physical examination, ankle-brachial indices (ABI), and either duplex ultrasound, computed tomography angiography (CTA), or digital subtraction angiography (DSA) to assess iliac and CFA disease burden. Patients with significant CFA occlusive disease with proximal extension into the external iliac artery (EIA) are considered for the combined procedure.
The presence of significant CFA disease is defined by:
Greater than 2.5× step-up increase in peak systolic velocity (PSV) across the CFA with duplex ultrasound scan.
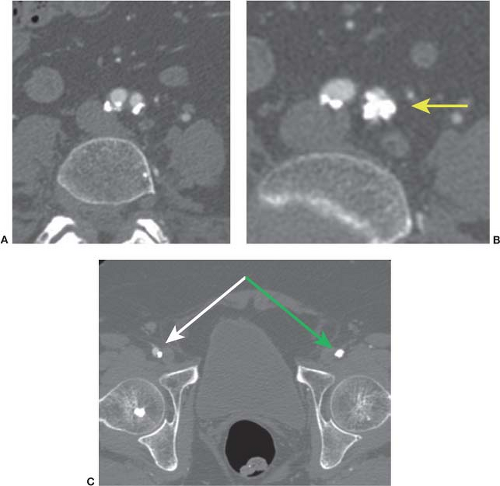
More than 50% diameter reduction on DSA or CTA (Fig. 3.1).
More than 10 mm Hg systolic pressure gradient at the time of angiography.
Selected patients with contralateral or infrainguinal disease requiring revascularization undergo various adjunctive procedures such as angioplasty/stenting, femoral-distal bypass, femoral–femoral crossover bypass as needed at the time of femoral endarterectomy.
Positioning
Patient is placed supine of in the operating on an x-ray compatible table. The procedure is preferably performed in a hybrid operating room with high-quality fluoroscopic imaging and the availability of intravascular ultrasound (IVUS).
Procedure
Standard CFA exposure is gained usually under general anesthesia though local anesthesia with conscious sedation is an option in selected patients.
The CFA is exposed usually through a longitudinal incision. The circumflex femoral arteries are looped with vessel loops as is the profunda femoris artery. The CFA above the circumflex femorals is also looped.
Needle-guided retrograde guidewire access through the CFA is then obtained under fluoroscopic guidance. This is performed prior to endarterectomy to avoid retrograde dissection which can easily occur following attempts at retrograde guide wire passage after endarterectomy. In patients with chronic total occlusion (CTO) of the EIA it is less important to obtain guidewire access prior to CFA endarterectomy. Typically the bulky component of the CFA plaque is located on the posterior aspect of the vessel and the flow lumen maybe located very anteriorly within the vessel.
Standard endarterectomy and patch angioplasty are then performed with the guidewire in place. Efforts are undertaken to ensure that adequate profunda femoris artery outflow is preserved or restored.
The wire is then back-fed through the center of the patch and a retrograde working sheath is placed once inflow has been restored. A second option is to incorporate the sheath into the anastomosis so that it exits the side of the patch (see Fig. 3.2).
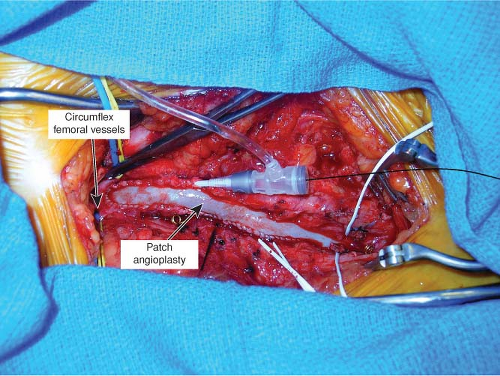
Figure 3.2 Intraoperative photograph. Note that sheath is usually placed through the center of the patch.
Standard interventional techniques are then used to treat the proximal arterial lesion. If guidewire access could not be obtained initially, it is then attempted after endarterectomy. With the development of reentry devices that are used for crossing CTOs of the iliac system (Pioneer Reentry Catheter, Medtronic, Santa Rosa, CA; Outback Reentry Catheter, Cordis, Miami Lakes, FL) it is rare, but occasionally, contralateral iliac artery or brachial artery access is required in order to cross the lesion antegrade. For EIA CTO we frequently use the Pioneer Reentry Catheter (Medtronic, Santa Rosa, CA) to cross the CTO and reenter just distal to the internal iliac artery. This allows for treatment of the EIA while maintaining patency of the internal iliac.
Arterial diameter and lesion measurements are made using preoperative CT scan measurements, IVUS or calibrated using a marker catheter and fluoroscopy imaging software.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree