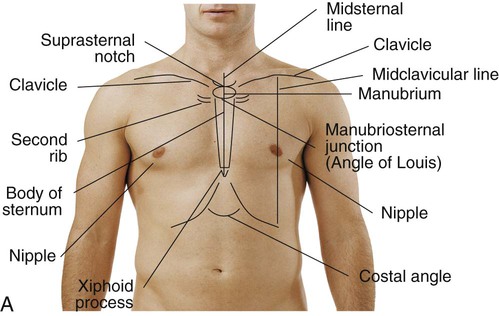
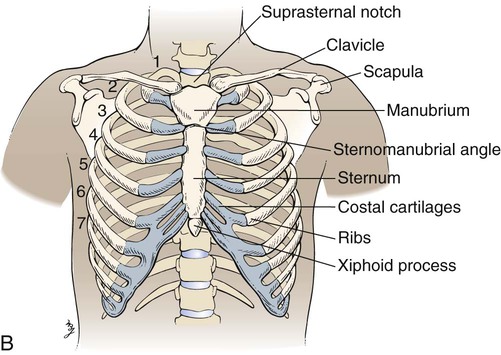
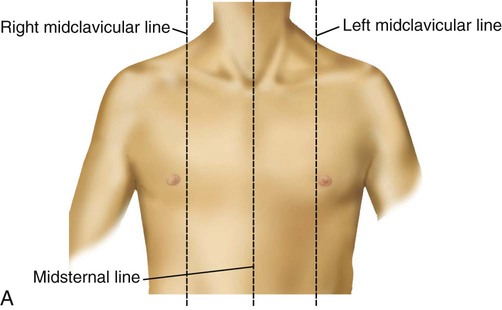
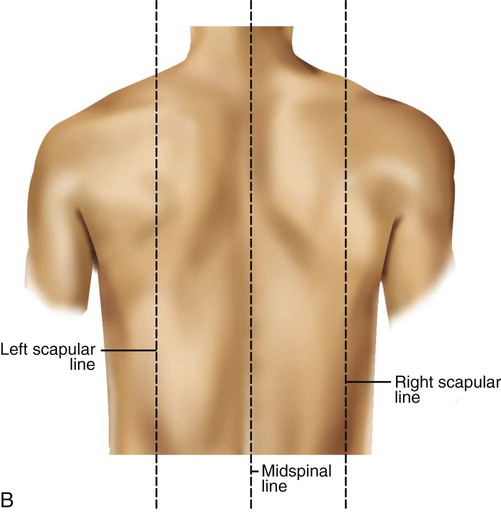
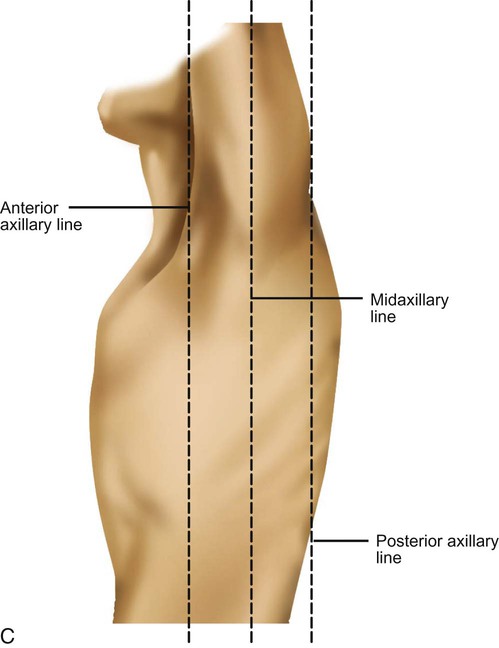
The Guide to Physical Therapist Practice provides a thorough patient management model.1 It identifies the key components necessary for a thorough examination and evaluation of the patient, tests and measures, identification of impairments, and interventions and outcomes that help the therapist in providing a multisystem examination and evaluation that will lead to appropriate treatment and achievement of optimal function and goals (see Figure 17-2). 1. Read the history and the physical and admission medical notes (i.e., the preadmission symptoms, past medical history)—this includes the physician’s notes and the nurse’s notes. 2. Read the most recent medical notes. 3. Scan the remainder of the chart. 4. Read any reports from medical specialists and consultants, such as pulmonologists, neurologists, or oncologists. 5. Review any pertinent lab tests, such as chest radiograph, arterial blood gases (ABGs), complete blood count (CBC), cardiac tests, CAT scans, and MRIs. 6. Review medications—in particular, pulmonary and cardiac drugs. 7. Review any procedures performed (e.g., surgery, intubation, chest tubes, NG tubes). 8. Review the psychosocial information (e.g., family, support systems, education, financial concerns, psychological issues, architectural barriers). Details regarding the patient interview have been covered in Chapter 7. However, there are questions that should be posed to any patient, even if his or her primary condition is not cardiovascular and/or pulmonary. The patient whose primary referring impairment is musculoskeletal or neurological needs to have a screening of the cardiovascular and pulmonary system. The therapist should consider the following questions: What is the patient’s smoking history? Does the patient have a family history of premature coronary artery disease (i.e., a parent or sibling who had a myocardial infarction)? Can the symptoms presented also be signs of a cardiovascular or pulmonary illness? Does the patient have an active or a sedentary lifestyle? What activities precipitate the patient’s symptoms? Do these symptoms include breathlessness? Are there problems with airway clearance, congestion, etc.? Key anatomic structures include the following: See Box 15-1 and Figure 15-1 for specific definitions and anterior and lateral views of the thorax. Imaginary topographic lines are used to more clearly describe any physical findings (e.g., location of surgical incisions, abnormal breath sounds, etc.; Figure 15-2). The anterior view of the thorax has three vertical lines: Laterally, there are also three vertical lines, originating in their respective axillary folds: The posterior chest has the following three lines: Does the patient appear comfortable? Is there any facial grimacing? Is the patient awake and alert or somnolent or disoriented? Is there any nasal flaring, wheezing, or pursed-lip breathing? (These are signs of respiratory distress. Nasal flaring can be defined as the outward movement of the nares with inspiration.2) Are the accessory muscles of respiration (i.e., sternocleidomastoid and trapezius) hypertrophied? How is the patient positioned? Is the patient resting comfortably or leaning forward over the bedside table and struggling for breath? What is the patient’s build—stocky, thin, or cachectic? Is the patient’s mobility limited? Can the patient sit unsupported? Should the assessment be performed in stages, allowing the patient to be supine and then to lie on each side? Is there any extra equipment in the patient’s surroundings? Is the patient using supplemental oxygen? Is the oxygen delivered through a nasal cannula or other device? What is the fraction of inspired oxygen (FiO2)? Are there any monitoring lines, and where are they located? For instance, if an arterial line is present, is it placed in the radial or the femoral artery? Are there electrocardiogram (ECG) leads? Is it a hard line (directly connected to a monitor) or a telemetry line (communicating through radio transmitter)? Are there intravenous (IV) sites? Are they peripheral (antecubital) or central (subclavian or jugular)? Is there a urinary catheter? Are there chest tubes?
Clinical Evaluation and Assessment of the Cardiovascular and Pulmonary System
History: Review and Interview
Medical Chart Review
Patient/Family Interview
Topographic Anatomic Landmarks
 Midsternal line (MSL)—a vertical line bisecting the sternum
Midsternal line (MSL)—a vertical line bisecting the sternum
 2 Midclavicular lines (MCLs)—parallel to the MSL, bisecting each clavicle; the borders of the lower lung cross the sixth ribs at the MCLs
2 Midclavicular lines (MCLs)—parallel to the MSL, bisecting each clavicle; the borders of the lower lung cross the sixth ribs at the MCLs
Visual Inspection
General Appearance
Clinical Evaluation and Assessment of the Cardiovascular and Pulmonary System