Chronic Pulmonary Consolidation
Dharshan Vummidi, MD
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Endobronchial Tumor
Aspiration
Bronchioloalveolar Carcinoma
Less Common
Coccidioidomycosis
Blastomycosis
Cryptogenic Organizing Pneumonia
Lymphoma
Chronic Eosinophilic Pneumonia
Rare but Important
Sarcoidosis
Lipoid Pneumonia
Churg-Strauss Syndrome
Pulmonary Alveolar Proteinosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Acute vs. chronic
Helpful Clues for Common Diagnoses
Endobronchial Tumor
Endobronchial soft tissue mass or broncholith obstructing bronchus
Air bronchograms often absent within consolidation
CT may show fluid attenuation filling bronchi
Signs of volume loss, such as fissural or hilar displacement
Consider broncholith in presence of calcified lung nodules and calcified lymph nodes
Aspiration
Basal predominant consolidation, often bilateral
CT shows peribronchial consolidation with bronchial wall thickening and tree in bud opacities
Debris and fluid in central airways
Bronchiectasis suggests chronicity
Findings of esophageal dysmotility such as retained fluid and debris
Bronchioloalveolar Carcinoma
Slowly progressive lung consolidation
May increase in both size and density
CT often shows mixed consolidation and ground-glass opacity
Crazy-paving and septal thickening less common
Dilated airways within consolidation: “Pseudocavitation”
Helpful Clues for Less Common Diagnoses
Coccidioidomycosis
Endemic in desert regions of southwestern USA
Single or multiple foci of lung consolidation
Nodules less common, may cavitate
Lymphadenopathy in 20% of patients
Pleural effusion in 10-20% of patients
Blastomycosis
Endemic in central and eastern USA along major rivers and around the Great Lakes
Single or multiple foci of lung consolidation
Slow to resolve or respond to therapy
Nodules and masses; cavitate in 1/3 of patients
Lymphadenopathy uncommon
Pleural effusion in 20% of patients
Cryptogenic Organizing Pneumonia
Subpleural, peribronchial, or perilobular consolidation or ground-glass opacity
Often has basal predominance
May wax and wane without treatment
Atoll or reverse halo sign: Focus of ground-glass opacity surrounded by ring-like or crescentic consolidation (20% of patients)
May also occur with infection, hemorrhage, and vasculitis
Responds to steroids
Lymphoma
Multiple nodules or foci of consolidation with associated lymphadenopathy
Primary pulmonary lymphoma far less common than secondary involvement
May present as solitary lung nodule or mass
Chronic Eosinophilic Pneumonia
Mid and upper lung predominant peripheral consolidation
“Reverse bat-wing” or “photographic negative of pulmonary edema” pattern on radiography
Responsive to steroid therapy
Helpful Clues for Rare Diagnoses
Sarcoidosis
Chronic lung consolidation uncommon manifestation
Upper lung predominance with air bronchograms
HRCT may show cluster of tiny nodules “galaxy” sign
Other features of sarcoidosis often present (e.g., lymphadenopathy)
Lipoid Pneumonia
Chronic mass-like consolidation and ground-glass opacity
Basal predominance (similar distribution to other causes of aspiration)
Fat attenuation of consolidation on CT virtually diagnostic
Mineral oil aspiration most common cause (exogenous)
Endogenous lipoid pneumonia from impaired surfactant metabolism
Chronic amiodarone therapy
Churg-Strauss Syndrome
Transient pulmonary consolidation or ground-glass opacity in peripheral or random distribution
Associated with eosinophilic vasculitis and asthma
Pulmonary Alveolar Proteinosis
Accumulation of periodic-Schiff (PAS) positive material in alveolar spaces
Primary (idiopathic): Middle-aged men most commonly affected
Secondary: Related to blood stem cell transplant or hematologic malignancy
Imaging abnormalities out of proportion to clinical signs and symptoms
Chest radiograph: Diffuse or patchy consolidation and ground-glass opacity
CT: Crazy-paving in geographic distribution with interspersed areas of normal lung
Bronchoalveolar lavage is both diagnostic and therapeutic
Clinical improvement promptly after therapeutic lavage
Radiographic improvement may lag behind clinical improvement
Alternative Differential Approaches
Unilateral consolidation
Obstructive pneumonia
Bronchioloalveolar carcinoma
Bilateral
Aspiration, especially if basilar
Cryptogenic organizing pneumonia
Chronic eosinophilic pneumonia
Alveolar proteinosis
Multifocal peripheral consolidation
Lymphoma in setting of systemic lymphoma
Chronic eosinophilic pneumonia: Upper lung zone predominance and peripheral blood eosinophilia
Cryptogenic organizing pneumonia: Migratory opacities or basilar predominance
Sarcoidosis: Other findings of sarcoidosis (e.g., lymphadenopathy)
Image Gallery
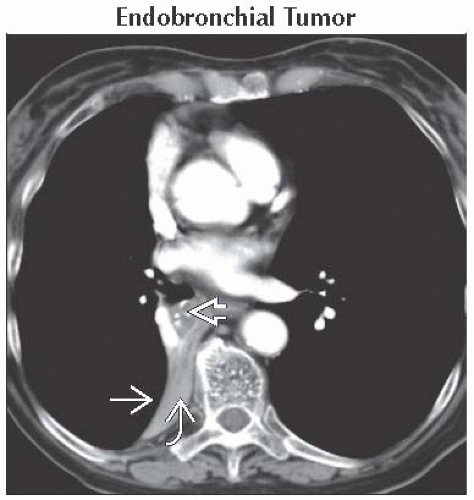 Axial CECT shows collapse of the right lower lobe
 with posteromedial displacement of the major fissure with posteromedial displacement of the major fissure  secondary to an obstructing lung carcinoma secondary to an obstructing lung carcinoma  in the right lower lobe bronchus. in the right lower lobe bronchus.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|