Pattern
Incidence
Causal agent
Diffuse
Common
Pneumocystis
Cytomegalovirus
Mycobacterium
Rare
Cryptococcus
Aspergillus
Candida
Nodular or cavitary
Common
Cryptococcus
Bacteria
Nocardia
Aspergillus
Mycobacterium
Rare
Legionella
Septic embolism
Focal
Common
Bacteria
Cryptococcus
Aspergillus
Mucor
Rare
Tuberculosis
Viruses
Legionella
Local infiltrates
Bronchiolitis obliterans with organizing pneumonia
Diffuse alveolar bleeding
Metastasis
Pharmacological toxicity
Graft-versus-host disease
Post-transplantation lymphoproliferative disease
Radiotherapy toxicity
Pulmonary alveolar proteinosis
Diffuse infiltrates
Metastasis
Pharmacological toxicity engraftment syndrome
Early infiltrates
Pulmonary edema
Pulmonary embolism
Atelectasis
Bleeding
Aspiration, acute respiratory distress syndrome
Chemotherapy
Late infiltrates
Radiation
Tumors
Chemotherapy
Etiology
- 1.
The type of immunosuppression that the patient has.
- 2.
The medical history, physical examination, epidemic status, clinical presentation, and speed at which the respiratory disorder has developed: acute, subacute, or chronic.
- 3.
The timing of the appearance of the respiratory disorder relative to that of the base illness, transplantation, or immunosuppressive drug administration.
- 4.
The preliminary results of general and specific examinations to establish the etiology.
- 5.
The type of radiological infiltrate (diffuse, focal, nodular, cavitated) and the images obtained from computerized tomography (CT scanning), ultrasound scanning, or nuclear magnetic resonance imaging.
- 6.
The drugs and treatments the patient has received, considering that some of them might favor immunosuppression and/or lung damage. The use of immunosuppressive treatments needs to be noted in patients with transplants, such as cyclosporin, steroids, mycophenolate, monoclonal antibodies, or antithymocyte globulins.
- 7.
Chemotherapy drugs such as bleomycin, cyclophosphamide, and methotrexate can cause lung damage, while radiotherapy can cause myelosuppression and lung fibrosis.
Because of their base condition and chemotherapy/radiotherapy, oncological patients have periods of neutropenia and secondary cell immunodeficiency, with a higher risk of developing viral pneumonia due to respiratory syncytial virus (RSV), adenovirus, enterovirus, or varicella zoster; or mycotic pneumonia due to Aspergillus, P. jirovecii, Mucor, Rhizopus, or occasionally Candida. The possibility of pneumonia associated with M. tuberculosis—or, less often, Toxoplasma or Cryptococcus neoformans—must also be taken into account.
In patients who have undergone bone marrow or solid organ transplantation, lung complications will depend on the period of immunosuppression associated with the transplantation.
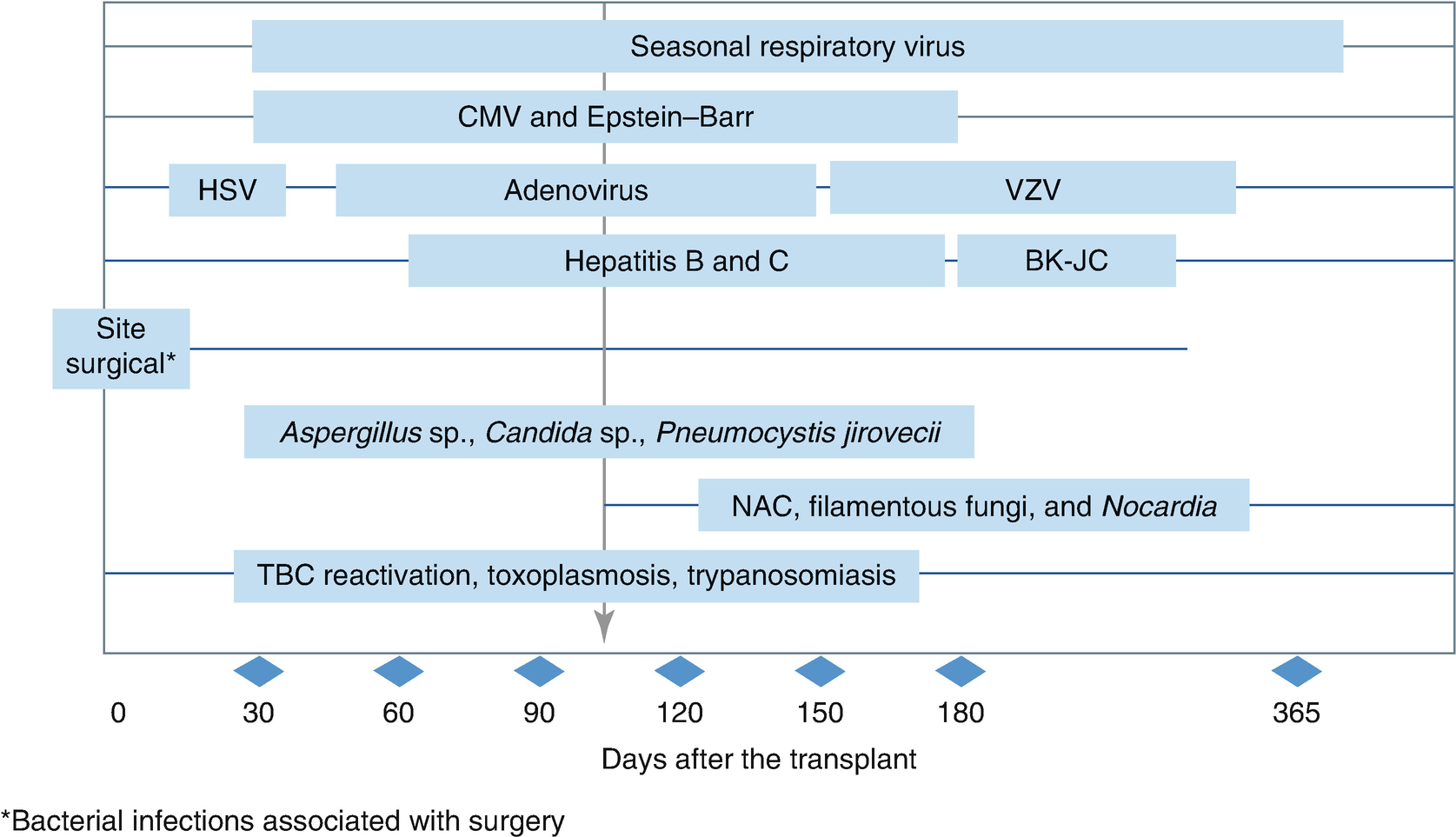
Timing of infections in solid organ transplant recipients
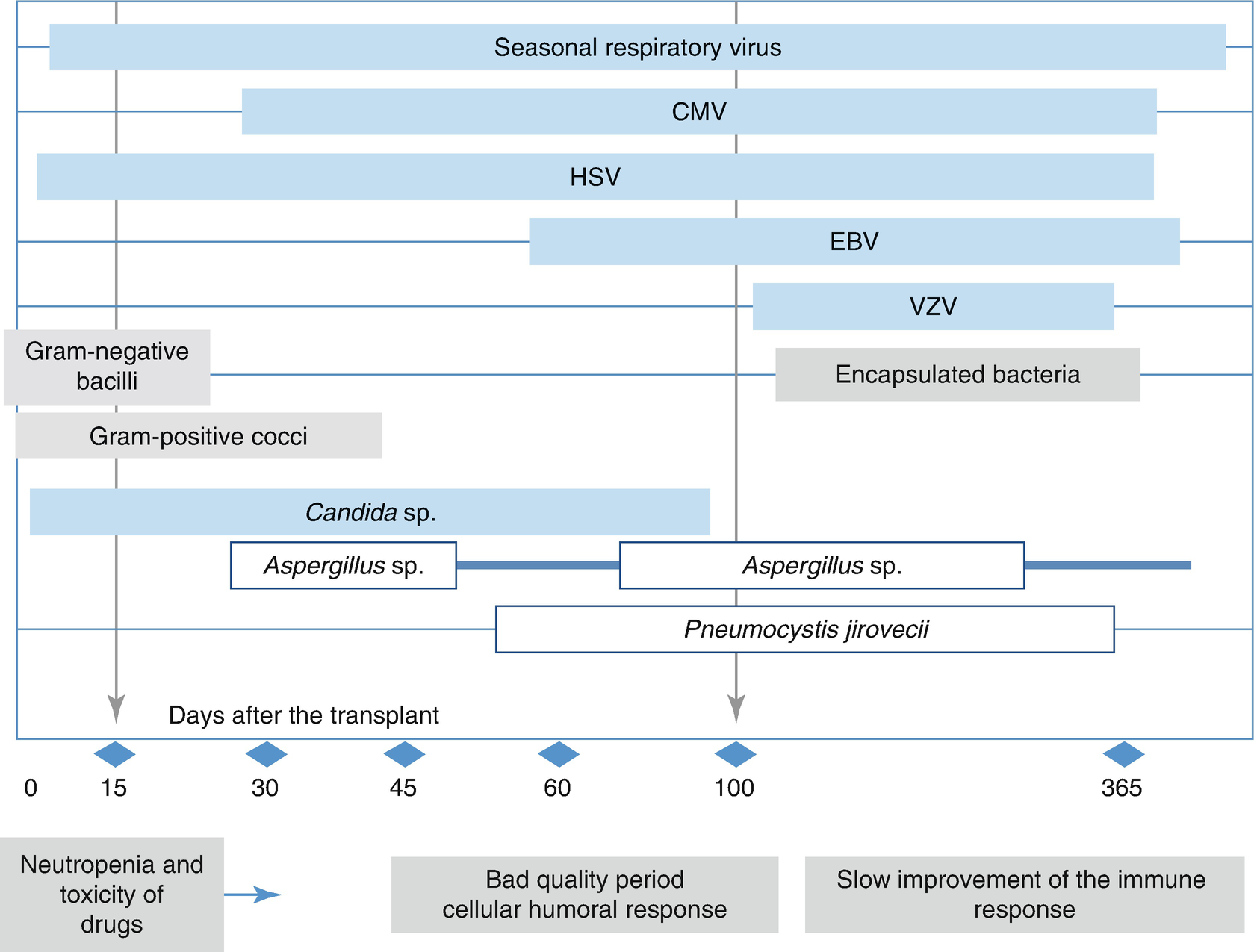
Timing of infections in hematopoietic precursor transplant recipients
Patients with common variable immune deficiency and agammaglobulinemia present recurrent bacterial pneumonia, normally produced by encapsulated germs; they are rarely present in pneumonia caused by P. jirovecii. Children with T cell immunodeficiency, serious combined immunodeficiencies, etc., have a higher risk of contracting the same type of opportunistic diseases as patients with acquired immunodeficiency syndrome (AIDS), as well as recurrent and persistent infections caused by Candida albicans in the mucosa or the skin. Patients with chronic granulomatous disease suffer lung infections caused by Aspergillus or Staphylococcus aureus—agents that require effective phagocytosis for their destruction. Children with primary immunodeficiency always present severe lung complications: bronchiectasis, empyema, lung abscesses, etc.
In patients with AIDS, there is a long list of associated lung infections, including those caused by P. jirovecii, CMV, Epstein–Barr virus, and mycobacteria, both typical and atypical. These are detailed in the corresponding chapter.
Immunosuppression and infectious etiology
Type of immunosuppression | Mechanisms compromised | Favored organisms | Common causes |
|---|---|---|---|
Phagocytosis | Engulfment of bacteria and fungi by mononuclear cells (monocytes and macrophages) and polymorphonuclear cells (neutrophils) Antigen presentation | Staphylococcus aureus, bacilli, Gram-negative aerobes (Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli), Candida spp., Aspergillus spp. | Neutropenia (leukemia, bone marrow suppression due to chemotherapy) Chronic granulomatous diseases Corticotherapy Hyper-IgE (Job syndrome) |
Humoral immunity | B lymphocytes Neutralization Opsonization Complement activation | Extracellular encapsulated bacteria: Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus | Primary: agammaglobulinemia, IgA deficiency, IgM deficiency Secondary: myeloma, Waldenström macroglobulinemia, lymphocyte leukemia |
Complement | Mediation of opsonization Attraction of inflammatory cells Elimination of microorganisms through damage to their membranes | C3-C5: encapsulated bacteria C5–C9: Neisseria gonorrhoeae, Neisseria meningitidis | C3–C5: encapsulated bacteria C5–C9: Neisseria gonorrhoeae, Neisseria meningitidis |
Cellular immunity | T lymphocytes Killing of pathogen-infected cells by cytotoxic T (CD8) cells Macrophage activation by Th1 (CD4) cells B lymphocytes activation by Th2 (CD4) cells to produce antibodies | Mycobacterium tuberculosis, Mycobacterium avium-c, Nocardia asteroides, Legionella spp., Cryptococcus neoformans, Histoplasma capsulatum, Coccidioides immitis, varicella zoster, herpes simplex, Cytomegalovirus, Epstein–Barr virus, Pneumocystis jirovecii, Toxoplasma gondii | Primary Secondary: malnutrition, lymphoma, leukemia, old age, drugs, AIDS Corticosteroids |
Hyposplenia/asplenia | Blood filtration Production of bacteria-specific antibodies Removal of bacteria covered in antibodies | Encapsulated bacteria | Thrombotic thrombocytopenic purpura, Hodgkin lymphoma |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


