Physical examination, electrocardiograms, and an echo-Doppler study document multiple consequences of a right coronary arterial occlusion.
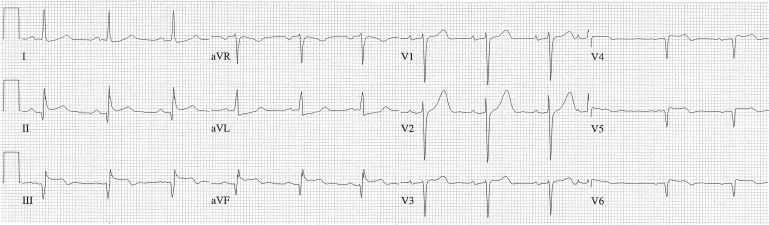
A 45-year-old man came to the emergency department because of the acute onset of chest pain, and a holosystolic murmur was heard at the cardiac apex. He had a history of systemic arterial hypertension and Hodgkin’s lymphoma but not a heart murmur. Electrocardiograms (ECGs) 1 and 2 years earlier had been normal. On this admission, 2 ECGs were recorded 3 minutes apart in the emergency department, and a third was recorded 5 days later ( Figures 1 to 3 ).
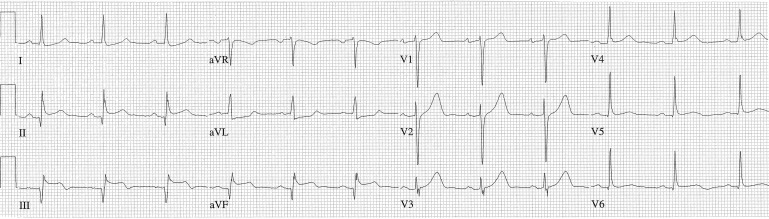
Initial ECG in the emergency department showed normal sinus rhythm and an AIMI.
ECG 3 minutes later showed sinus rhythm, a premature atrial complex, AIMI, and an acute right ventricular MI. See text for further explication.

ECG 5 days later showed sinus rhythm, type I second degree AVB, and left atrial enlargement.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


