Chest Pain
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Acute Myocardial Infarction
Pulmonary Embolism
Pneumothorax
Rib Fracture
Pneumonia
Bronchitis
Less Common
Acute Aortic Syndrome
Pleural Effusion
Diffuse Esophageal Spasm
Gastrointestinal Abnormalities
Aortic Stenosis
Pericardial Disease
Metastatic Disease
Sickle Cell Anemia
Sarcoidosis
Rare but Important
Esophageal Tear
Mediastinitis
Chest Wall Mass
Chest Wall Infection
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Chest pain presenting to primary care physician is usually benign
Usually no radiographic abnormalities
Chest radiograph is initial radiographic examination in emergency department
Helps to exclude conditions that may mimic acute coronary syndrome
Helpful Clues for Common Diagnoses
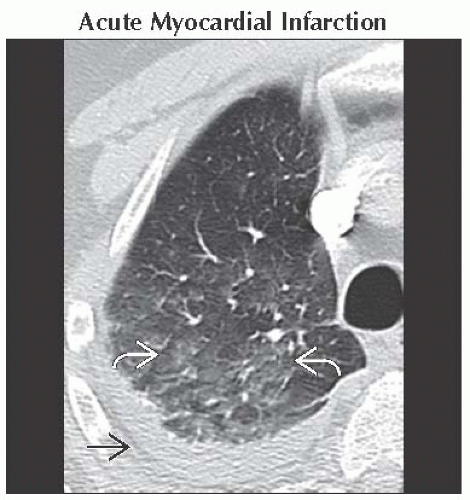
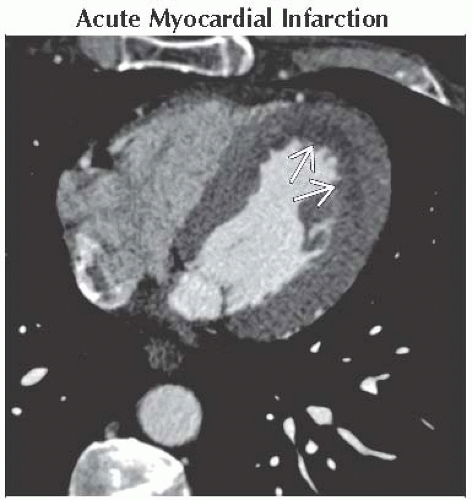
Acute Myocardial Infarction
Chest radiograph normal in 50%
Pulmonary edema without cardiomegaly in 50%
Pulmonary Embolism
Chest radiograph abnormal in most patients
Cardiomegaly is most common finding
Hampton hump and Westermark sign infrequently seen
CTA: Intraluminal filling defect surrounded by contrast is diagnostic
“Doughnut” or “railroad track” sign
Signs of right heart strain
RV/LV chamber size ≥1, leftward bowing of interventricular septum, and reflux into inferior vena cava
Pneumothorax
Spontaneous
Rupture of apical bleb or bulla
Young, tall, and thin male smokers
Association with emphysema, cystic lung disease, asthma, infection, or lung fibrosis
Recurrence is common
Traumatic pneumothorax due to
Chest trauma or mechanical ventilation
Rib Fracture
ACR states rib radiography not recommended for diagnosis
Pneumonia
Symptoms of infection
Lobar or segmental lung consolidation
Bronchitis
Radiograph usually normal
± bronchial wall thickening and mucus plugging
Helpful Clues for Less Common Diagnoses
Acute Aortic Syndrome
Sudden onset of severe chest/back pain
Predisposing factors
Hypertension, bicuspid aortic valve, and connective tissue disorders
All 3 conditions have similar classification
Stanford type A involves ascending aorta and is treated surgically
Stanford type B occurs distal to left subclavian artery and is treated medically
Life-threatening complications of type A aortic dissection
Pericardial tamponade, myocardial infarction, acute aortic insufficiency, and stroke
Intramural hematoma
Diagnose with noncontrast CT
Crescent-shaped, high-density thickening of aortic wall
Penetrating aortic ulcer
Atherosclerotic plaque rupture with focal contrast collection within media
Common in descending thoracic aorta
May propagate and lead to dissection
Pleural Effusion
Pain usually indicates pleuritis
Diffuse Esophageal Spasm
Reproduction of pain with tertiary contractions on esophagram
Gastrointestinal Abnormalities
Occasionally present with chest pain
Normal chest radiograph or basal atelectasis
Chest CT may detect unsuspected intraabdominal abnormality
Aortic Stenosis
Radiograph shows
± aortic valvular calcifications
Enlarged ascending aorta with normal heart size
Pericardial Disease
Pain with pericarditis, pericardial effusion, or metastatic disease
Pericarditis
Thickening and enhancement of pericardium
Pericardial fluid
Metastatic Disease
Bone or lung metastases can cause pain
Multiple well-circumscribed lung nodules in random distribution
Lytic or blastic bony lesions
Sickle Cell Anemia
Acute chest syndrome
Vasoocclusive crisis with new lung opacity, ± fever, chest pain, and respiratory symptoms
Secondary to infection, infarction, pain episode, or fat embolism
Predisposes to pulmonary arterial hypertension through lung fibrosis
H-shaped vertebral bodies, avascular necrosis of humeral heads, and expanded ribs
± posterior mediastinal extramedullary hematopoiesis
Sarcoidosis
Bilateral hilar and right paratracheal lymphadenopathy
Perilymphatic distribution of lung nodules (nodules along fissures, subpleural lung, and bronchovascular bundles)
Helpful Clues for Rare Diagnoses
Esophageal Tear
Occurs with trauma, retching, or iatrogenic injury
Pneumomediastinum, extravasated oral contrast, and periesophageal fluid collections
Mediastinitis
Associated with sternotomy, esophageal perforation, or spread of adjacent infection
Postoperative fluid collections normally resolve in 2-3 weeks
CT findings
Diffuse mediastinal fat stranding and fluid collections
Pneumomediastinum
Chest Wall Mass
Pain occurs with Pancoast tumor and numerous sarcomas
Chest Wall Infection
Rib sclerosis or periosteal reaction indicates osteomyelitis
Image Gallery
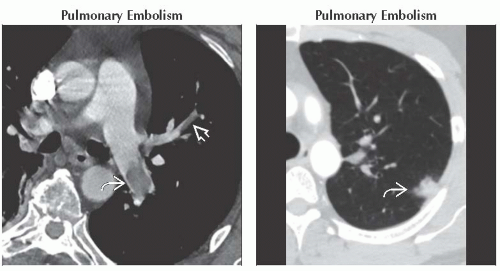 (Left) Axial CECT shows large pulmonary embolism in the left pulmonary artery
 with typical “railroad track” sign. Smaller embolism is noted in a segmental left upper lobe pulmonary artery with typical “railroad track” sign. Smaller embolism is noted in a segmental left upper lobe pulmonary artery  . It is important to report signs of right heart strain in the setting of pulmonary embolism as it has prognostic implications. (Right) Axial CECT shows a peripheral infarct in the same patient . It is important to report signs of right heart strain in the setting of pulmonary embolism as it has prognostic implications. (Right) Axial CECT shows a peripheral infarct in the same patient  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|