Richard A. Lange, L. David Hillis
Chemical Cardiomyopathies
Many toxins, some used by a substantial fraction of the population, may affect the heart adversely, so it is important to understand the myriad ways in which these substances may influence the cardiovascular system. This chapter focuses on environmental exposures and commonly prescribed pharmacologic agents, as well as frequently used illicit drugs, including cocaine and amphetamines. Chapter 69 discusses the toxicities of various chemotherapeutic agents in greater detail.
Ethanol
An estimated two thirds of Americans occasionally consume ethanol, and approximately 10% are considered heavy consumers. Although ingestion of a moderate amount of ethanol (usually defined as three to nine drinks per week) is associated with a reduced risk for cardiovascular disease, binge drinking and the consumption of excessive amounts have the opposite effect. When ingested in substantial amounts, ethanol may cause ventricular systolic and/or diastolic dysfunction, systemic arterial hypertension, angina pectoris, arrhythmias, and even sudden cardiac death.
Effects of Ethanol on Cardiac Myocyte Structure and Function
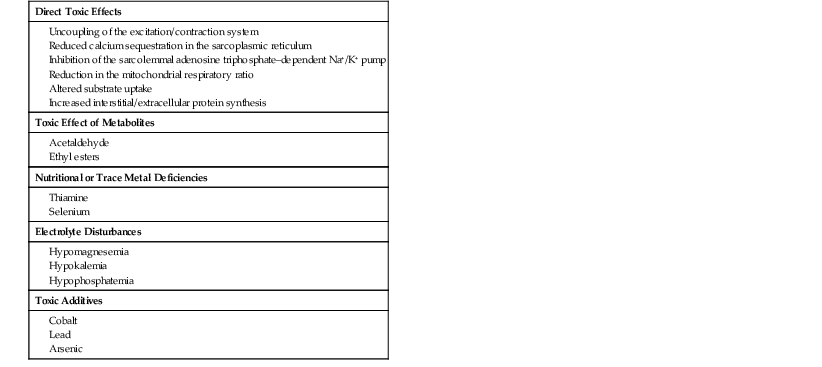
Ethanol may cause myocardial damage via several mechanisms (Table 68-1).1 First, ethanol and its metabolites acetaldehyde and acetate may exert a direct toxic effect on the myocardium. Second, deficiencies of certain vitamins (e.g., thiamine), minerals (e.g., selenium), or electrolytes (e.g., magnesium, phosphorus, or potassium), which sometimes occur in heavy ethanol consumers, may adversely affect myocardial function. Third, certain substances that sometimes contaminate alcoholic beverages, such as lead (often found in “moonshine” alcohol) or cobalt, may damage the myocardium.
TABLE 68-1
Mechanisms of Ethanol-Induced Myocardial Injury
| Direct Toxic Effects |
| Toxic Effect of Metabolites |
| Nutritional or Trace Metal Deficiencies |
| Electrolyte Disturbances |
| Toxic Additives |
Ethanol impairs excitation-contraction coupling, mitochondrial oxidative phosphorylation, and cardiac contractility by adversely affecting the function of the sarcolemmal membrane, the sarcoplasmic reticulum, mitochondria, and contractile proteins. Electron microscopic studies of the hearts of experimental animals in close temporal proximity to heavy ethanol ingestion demonstrate dilated sarcoplasmic reticula and swollen mitochondria, along with fragmented cristae and glycogen-filled vacuoles. With sustained exposure to ethanol, myofibrillar degeneration and replacement fibrosis appear. In addition to the effects of ethanol on the myocardial contractile apparatus, acute or chronic consumption may adversely influence myofibrillar protein synthesis. Microscopically, the hearts of chronic heavy consumers of ethanol manifest an increased accumulation of collagen in the extracellular matrix, as well as increased intermolecular cross-links.
Effects of Ethanol on Organ Function
Chronic heavy ethanol ingestion may induce left ventricular diastolic and/or systolic dysfunction. Diastolic dysfunction, which is caused, at least in part, by interstitial fibrosis of the myocardium, is often demonstrable in heavy consumers of ethanol even in the absence of symptoms or obvious signs. About half of asymptomatic chronic alcoholics have echocardiographic evidence of left ventricular hypertrophy with preserved systolic performance. By Doppler echocardiography (see also Chapter 14), left ventricular relaxation time is often prolonged, peak early diastolic velocity is reduced, and the acceleration of early diastolic flow is slowed—all manifestations of left ventricular diastolic dysfunction. Even small amounts of alcohol are associated with an acute worsening of diastolic function, as assessed by early diastolic velocity (E′), its ratio to late diastolic velocity (E′/A′), and the ratio of mitral to myocardial early diastolic velocity (E/E′).2 Abnormal increases in left ventricular filling pressure during volume or pressure loading may be observed.
Ethanol may induce asymptomatic left ventricular systolic dysfunction even when it is ingested by healthy individuals in relatively small quantities, as occurs in subjects who are considered “social” drinkers. As many as 30% of asymptomatic chronic alcoholics have echocardiographic evidence of left ventricular systolic dysfunction. With continued heavy ethanol ingestion, symptoms and signs of heart failure often develop (see also Chapters 23 and 25) as a result of dilated cardiomyopathy. In fact, ethanol abuse is the leading cause of nonischemic dilated cardiomyopathy in industrialized countries; it accounts for approximately half of those with this diagnosis. The likelihood of ethanol-induced dilated cardiomyopathy developing correlates with the amount of ethanol that is consumed in a lifetime: most men in whom it develops have consumed more than 80 g of ethanol (i.e., 1 liter of wine, eight standard-sized beers, or one-half pint of hard liquor) per day for at least 5 years. Women appear to be even more susceptible than their male counterparts to ethanol’s cardiotoxic effects in that dilated cardiomyopathy may develop in women following the consumption of a smaller amount of ethanol per day and per lifetime.
Although heavy intake of ethanol is associated with nonischemic dilated cardiomyopathy, individuals with light to moderate ethanol consumption (5 to 25 g/day) actually have a lower incidence of congestive heart failure than do those who do not drink at all.1 In patients with left ventricular dysfunction, light to moderate ethanol ingestion does not exacerbate heart failure. In subjects with ischemic cardiomyopathy, light to moderate ethanol consumption may reduce mortality.1,3,4
Subjects with markedly symptomatic ethanol-induced dilated cardiomyopathy may manifest a substantial improvement in left ventricular systolic function and symptoms of heart failure with complete abstinence or a dramatic reduction in ethanol consumption (i.e., to less than 60 g of ethanol per day or the equivalent of four standard drinks). Although most of this improvement occurs in the first 6 months of abstinence, it often continues for as long as 2 years of observation.
Ethanol and Systemic Arterial Hypertension
Experts estimate that ethanol has causal importance in up to 11% of men with hypertension (see Chapter 43). Individuals who consume more than two drinks daily are 1.5 to 2 times more likely to have hypertension than are age- and sex-matched nondrinkers. This effect is dose related and most prominent when daily ethanol intake exceeds five drinks (i.e., 30 g of ethanol).5 “Social” ethanol consumption is associated with a modest rise in systolic arterial pressure, whereas heavy consumption and binge drinking may lead to a substantial increase. Although the mechanism by which ethanol induces a rise in systemic arterial pressure is poorly understood, studies have demonstrated that ethanol consumption increases plasma levels of catecholamines, renin, cortisol, and aldosterone, each of which may cause systemic arterial vasoconstriction. In individuals with ethanol-induced hypertension, abstinence often normalizes systemic arterial pressure.
Ethanol and Lipid Metabolism
Ethanol consumption inhibits the oxidation of free fatty acids by the liver, which stimulates hepatic triglyceride synthesis and the secretion of very low-density lipoprotein cholesterol. Most commonly, therefore, ethanol consumption causes hypertriglyceridemia. In addition, heavy ingestion may cause an increase in the serum concentrations of total cholesterol and low-density lipoprotein (LDL) cholesterol. Regular ethanol consumption increases the serum concentration of high-density lipoprotein (HDL) cholesterol.6 Subjects with hyperlipidemia should be encouraged to limit their ethanol intake.
Coronary Artery Disease
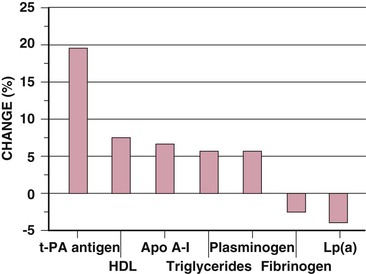
Heavy ethanol use is associated with an increased incidence of atherosclerotic coronary artery disease and resultant cardiovascular morbidity and mortality (see also Chapter 54). This rise may result, at least in part, from the increased likelihood that heavy ethanol consumers (versus nondrinkers) have systemic arterial hypertension, increased left ventricular muscle mass (with concomitant diastolic and/or systolic dysfunction), and hypertriglyceridemia (Table 68-2). Conversely, light to moderate ethanol intake (two to seven drinks per week) is associated with a decreased risk for cardiovascular morbidity and mortality in both men and women.7–12 Even in men already at low risk for cardiovascular disease on the basis of body mass index, physical activity, smoking, and diet, moderate alcohol intake is associated with a reduced risk for myocardial infarction (MI) (Fig. 68-1).13 This lower risk for cardiovascular morbidity and mortality in consumers of moderate amounts of ethanol than in nondrinkers or heavy consumers is supported by numerous retrospectively and prospectively conducted studies. The French were noted to have a reduced incidence of coronary artery disease when compared with inhabitants of other countries despite high smoking rates and a diet high in fat (the so-called French paradox). Although this diminished incidence was initially attributed to the antioxidant and hemostatic properties of red wine, similar findings were subsequently reported in mild to moderate consumers of other alcoholic beverages and in other study populations.7–12 Several prospectively performed cohort studies have demonstrated that drinkers of moderate amounts of ethanol are 30% to 70% less likely than nondrinkers or heavy consumers to manifest coronary artery disease or ischemic stroke.14 Some studies have suggested that the consumption of all alcoholic beverages exerts such an effect, whereas others have reported that this so-called cardioprotection is strongest with the consumption of wine.15 The mechanism or mechanisms by which the consumption of moderate amounts of ethanol reduces cardiovascular risk appear to be multifactorial in that moderate consumption exerts several beneficial effects, including (1) an increase in the serum concentrations of HDL cholesterol, apolipoprotein A-I, and adiponectin; (2) inhibition of platelet aggregation; (3) decreased serum fibrinogen concentration; (4) increased antioxidant activity (from the phenolic compounds and flavonoids contained in red wine); (5) anti-inflammatory effects (with lower concentrations of white blood cells and C-reactive protein); (6) improved fibrinolysis (resulting from increased concentrations of endogenous tissue plasminogen activator and a concomitant decrease in endogenous plasminogen activator inhibitor activity); and (7) improved insulin sensitivity (Fig. 68-2).6,12,16
TABLE 68-2
Qualitative Effects of Light to Moderate and Heavier Alcohol Intake on Cardiovascular Risk Factors and Outcomes
| CARDIOVASCULAR RISK FACTORS AND OUTCOMES | LIGHT TO MODERATE ALCOHOL INTAKE (<2 DRINKS PER DAY) | HEAVIER ALCOHOL INTAKE (>2 DRINKS PER DAY) |
| Blood pressure | ↔ | ↑↑ |
| HDL cholesterol | ↑↑ | ↑↑↑ |
| Triglycerides | ↑ | ↑↑ |
| LDL cholesterol | ↔ or ↓ | ↑ |
| Platelet aggregability/coagulability | ↓ | ↓↓ |
| Systemic inflammation | ↓ | ↑ |
| Congestive heart failure | ↓ | ↑↑ |
| Coronary artery disease (angina, nonfatal MI) | ↓↓ | ↓ |
| Atrial fibrillation | ↔ | ↑↑ |
| Stroke | ↓ | ↑↑ |
| Sudden cardiac death | ↓↓ | ↑ |
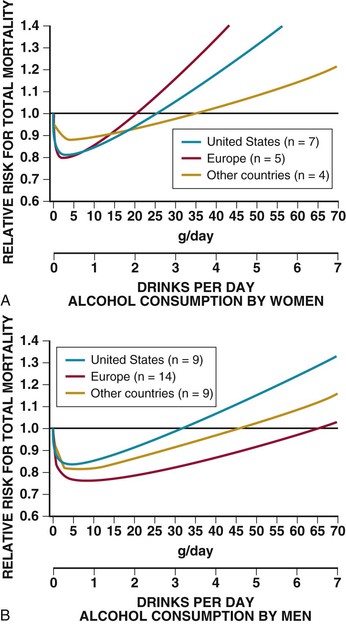
Men and women manifest a difference in the cardioprotective effect of alcohol (Fig. 68-3). The maximal beneficial effect of ethanol occurs at lower doses for women than for men, and the range of alcohol consumption at which it is protective is wider for men than for women. In addition, the relative cardioprotective effect of ethanol is greater for middle-aged and elderly individuals than for young adults.17 Light to moderate ethanol consumption is associated with similar reductions in risk for coronary artery disease in diabetic and nondiabetic men and women.18 In survivors of MI, moderate ethanol consumption appears to reduce subsequent mortality.3,4 In patients suffering an acute MI, those with light or moderate alcohol use have a better prognosis than do heavy drinkers or abstainers,3,19 even though recent ingestion of ethanol does not appear to reduce infarct size or the propensity for the subsequent appearance of arrhythmia or heart failure.
Arrhythmias
Ethanol consumption is associated with a variety of atrial and ventricular arrhythmias, most commonly (1) atrial or ventricular premature beats, (2) supraventricular tachycardia, (3) atrial flutter, (4) atrial fibrillation, (5) ventricular tachycardia, or (6) ventricular fibrillation (see also Chapters 34, 37, and 38). The most common ethanol-induced arrhythmia is atrial fibrillation. Ethanol is of causal importance in about a third of subjects with new-onset atrial fibrillation; in those younger than 65 years it may be responsible in as many as two thirds. Most episodes occur after binge drinking, usually on weekends or holidays—hence the term “holiday heart.” Electrophysiologic testing in humans without cardiac disease has shown that ethanol enhances vulnerability to the induction of atrial flutter and fibrillation. Treatment of these ethanol-induced arrhythmias is abstinence.
Ethanol may be arrhythmogenic via several mechanisms. In many ethanol consumers, concomitant factors may predispose to arrhythmias, including cigarette smoking, electrolyte disturbances, metabolic abnormalities, hypertension, and sleep apnea. Acute ethanol ingestion induces diuresis, which is accompanied by the concomitant urinary loss of sodium, potassium, and magnesium. The presence of myocardial interstitial fibrosis, ventricular hypertrophy, cardiomyopathy, or autonomic dysfunction may also enhance the likelihood of dysrhythmias. Prolongation of the QT interval, decreased heart rate variability, diminished vagal modulation, and reduced baroreflex sensitivity have also been noted in patients with alcohol use or withdrawal.20
Sudden Death
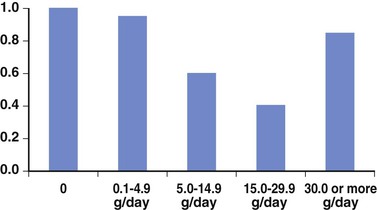
In subjects without known cardiac disease, the decrease in cardiovascular mortality that is associated with moderate ethanol intake results largely from a reduction in the incidence of sudden death (Fig. 68-4) (see also Chapter 39). Of the more than 21,000 men in the Physicians Health Study,21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree