Outcomes in patients with out-of-hospital cardiac arrest (CA) who undergo percutaneous coronary intervention (PCI) have been limited to small, mostly single-center studies. We compared patients who underwent PCI after CA included in the CathPCI Registry with those without CA. Patients with ST elevation were classified as ST-elevation myocardial infarction (STEMI); all other patients having PCI were classified as without STEMI. Patients with CA in each group were compared with the corresponding non-CA groups for baseline characteristics, angiographic findings, and outcomes. A total of 594,734 patients underwent PCI, of whom 114,768 had STEMI, including 9,375 (8.2%) had CA, and 479,966 had without STEMI, including 2,775 (0.6%) had CA. Patients with CA were similar in age to patients with non-CA, with a lower frequency of coronary disease risk factors and known coronary disease. On angiography, patients with CA were significantly more likely to have more complex lesions with worse baseline thrombolysis in myocardial infarction flow. Patients with CA were significantly more likely to have cardiogenic shock, both for patients with STEMI (51% vs 7.2%, respectively) and for patients without STEMI (38% vs 0.8%, respectively, both p <0.001). In-hospital mortality was substantially worse in patients with CA, for both patients with STEMI (24.9% vs 3.1%, respectively) and patients without STEMI (18.7% vs 0.4%, respectively). In conclusion, patients who underwent PCI after CA had more complex anatomy, more shock, and higher mortality. The substantially increased mortality in patients with CA has important implications for the development and regionalization of centers for CA.
Cardiac arrest (CA) affects approximately 235,000 to 325,000 patients in the United States a year. Many patients with CA present with ST elevation on the initial electrocardiogram. Emergent percutaneous coronary intervention (PCI) in these patients appears beneficial and is recommended in current guideline. In patients without ST elevation, the majority have underlying coronary disease, indicating that ischemia is a likely precursor for many of the events. However, the role of PCI in patients with CA without ST elevation who have return of circulation is less clear. Coronary angiography in these patients has demonstrated a high prevalence of underlying coronary artery disease and findings consistent with acute coronary syndrome. Current data are limited to relatively small populations often from single centers. Because CA is frequently an exclusion from randomized clinical trials, and most myocardial infarction registries have not collected information on patients with CA, outcomes from large studies are lacking. Therefore, we analyzed data from the National Cardiovascular Data Registry (NCDR) CathPCI Registry and report (1) the clinical features, (2) angiographic findings, and (3) outcomes in patients with and without ST-elevation myocardial infarction (STEMI) who underwent PCI after CA.
Methods
The CathPCI Registry is a large, ongoing registry of clinical data and procedural outcomes associated with diagnostic cardiac catheterization and PCI including >1,300 participating sites sponsored by the American College of Cardiology and the Society for Cardiovascular Angiography and Interventions. Data are captured at participating hospitals and include patient and hospital characteristics, procedural findings, interventions, and outcomes. The NCDR also has a comprehensive data quality program, including data abstraction training, data quality thresholds for inclusion, site data quality feedback reports, independent auditing, and data validation. Data auditing has demonstrated accurate representation with agreement with chart review >93%. Data elements and definitions are available at https://www.ncdr.com/WebNCDR/docs/public-data-collection-documents/cathpci_v4_codersdictionary_4-4.pdf?sfvrsn=2 . All data were collected using version 3 of the data collection form. This research was supported by the American College of Cardiology Foundation’s NCDR.
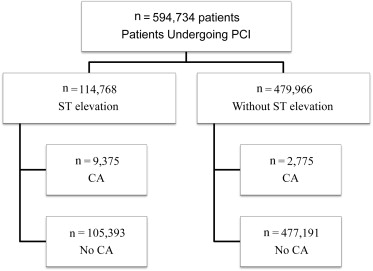
Patients who underwent PCI from August 2009 through July 2010 were included. Patients were classified into 4 groups based on whether they had CA before PCI and whether they met criteria for STEMI ( Figure 1 ). Patients who underwent coronary angiography without PCI (n = 4,244) or those without information on CA (n = 352) were excluded. Patients not classified as having STEMI were classified as without STEMI (non-STEMI, 1,624 [59%]; unstable angina, 598 [22%]; stable angina, 161 [5.8%]; atypical chest pain, 58 [2.1%]; and asymptomatic, 334 [12%]). CA was defined as a pulseless clinical scenario that could be bradycardic or tachycardic, requiring cardiopulmonary resuscitation (requiring 2 or more chest compressions or open chest massage) and/or requiring emergency defibrillation within 24 hours before PCI.
We also analyzed the subgroup of patients who had cardiogenic shock at presentation or after PCI. Cardiogenic shock was defined as sustained (>30 minutes) systolic blood pressure <90 mm Hg and/or cardiac index <2.2 L/min/m 2 secondary to cardiac dysfunction and/or the requirement for inotropic or vasopressor agents or mechanical support.
Categorical variables are summarized using percentages and compared using Pearson chi-square tests, whereas continuous variables are presented using median and compared using Wilcoxon rank-sum test. All p values were calculated using only nonmissing row values. p Value <0.05 was considered significant. All statistical analysis was performed using SAS software (version 9.2; SAS Institute, Cary, North Carolina).
Results
A total of 594,734 patients underwent PCI during the period of this analysis, of whom 114,768 had STEMI, including 9,375 (8.2%) had CA, and 479,966 patients had without STEMI, including 2,775 (0.6%) had CA ( Figure 1 ). Patients with CA were less likely to have coronary disease risk factors, known coronary artery disease, and previous revascularization, although they were more likely to be men ( Table 1 ). In addition, patients with CA were significantly more likely to have cardiogenic shock within 24 hours of PCI.
| Variables | STEMI | Without STEMI | ||||
|---|---|---|---|---|---|---|
| CA (n = 9,375) | No CA (n = 105,393) | p Value | CA (n = 2,775) | No CA (n = 477,191) | p Value | |
| Age, median (yrs) | 60 (52–69) | 60 (52–70) | 0.013 | 64 (56–74) | 65 (57–73) | 0.14 |
| Women | 26.8 | 28.4 | 0.0006 | 27.8 | 32.1 | <0.0001 |
| White | 89 | 88.5 | 0.10 | 88.8 | 89.7 | 0.12 |
| Diabetes mellitus | 20.7 | 24.1 | <0.0001 | 34.6 | 35.9 | 0.15 |
| Hypertension | 62.6 | 66.0 | <0.0001 | 77.5 | 83.8 | <0.0001 |
| Dyslipidemia | 56.5 | 63.2 | <0.0001 | 70.7 | 84.0 | <0.0001 |
| Previous myocardial infarction | 18.6 | 19.5 | 0.0391 | 30.6 | 30.3 | 0.74 |
| Previous heart failure | 6.5 | 4.5 | <0.0001 | 15.5 | 10.1 | <0.0001 |
| Previous percutaneous coronary intervention | 19.3 | 21.1 | <0.0001 | 30.8 | 44.5 | <0.0001 |
| Previous coronary bypass | 5.5 | 6.1 | 0.032 | 18.5 | 20.1 | 0.04 |
| Cerebrovascular disease | 7.8 | 6.9 | 0.0007 | 12.1 | 11.7 | 0.46 |
| Current/recent smoker (with 1 yr) | 45.2 | 42.7 | <0.0001 | 30.4 | 24.5 | <0.0001 |
| Chronic lung disease | 11.4 | 10.1 | 0.0002 | 16.6 | 14.1 | 0.0002 |
| Preprocedure glomerular filtration rate (ml/min/m 2 ) | 64.8 (50.8–80.5) | 74.4 (59.7–90.8) | <0.0001 | 64.6 (48.3–81.9) | 75.3 (59.8–90.6) | <0.0001 |
| Currently on dialysis | 1.4 | 1.0 | <0.0001 | 4.4 | 1.8 | <0.0001 |
| Canadian Cardiovascular Society Anginal Class within 2 weeks | ||||||
| 1 | 7.0 | 13.6 | <0.0001 | 6.9 | 14.4 | <0.0001 |
| 2 | 10.2 | 22.7 | 17.4 | 36.8 | ||
| 3 | 18.4 | 26.7 | 25.9 | 33.6 | ||
| 4 | 64.1 | 36.4 | 48.6 | 14.7 | ||
| Cardiogenic shock within 24 h | 50.9 | 7.2 | <0.0001 | 38.0 | 0.8 | <0.0001 |
Both groups of patients with CA were more likely to have multivessel disease and have an ejection fraction <40% than their corresponding groups without CA ( Table 2 ). Consistent with the increased incidence of cardiogenic shock, intra-aortic balloon pump use was more frequent in patients with CA. Patients with CA were more likely to have 100% occlusive lesion with preprocedural thrombolysis in myocardial infarction 0 flow; after PCI, patients with CA were more likely to have no, slow, or partial flow. Patients with CA in the without STEMI group were more likely to have an acute lesion or thrombus on coronary angiography as classified by the site.
| Variables | STEMI | Without STEMI | ||||
|---|---|---|---|---|---|---|
| CA (n = 9,375) | No CA (n = 105,393) | p Value | CA (n = 2,775) | No CA (n = 477,191) | p Value | |
| Intra aortic balloon pump use | 32.2 | 8.2 | <0.0001 | 19.7 | 0.8 | <0.0001 |
| Other mechanical ventricular support | 6.2 | 0.7 | <0.0001 | 5 | 0.2 | <0.0001 |
| Number of diseased vessels | ||||||
| 0 | 0.3 | 0.3 | 0.0298 | 0.5 | 0.6 | <0.0001 |
| 1 | 45.3 | 46.4 | 39.1 | 48.1 | ||
| 2 | 32.1 | 32.2 | 31.2 | 30.7 | ||
| 3 | 22.2 | 21 | 28.9 | 20.2 | ||
| Ejection fraction <40% | 77.2 | 64.2 | <0.0001 | 59.1 | 33.5 | <0.0001 |
| Procedure medications | ||||||
| Aspirin | 77.6 | 90 | <0.0001 | 75.9 | 86.7 | <0.0001 |
| Clopidogrel | 56.9 | 76.5 | <0.0001 | 61.8 | 80.8 | <0.0001 |
| Percent preprocedure stenosis | ||||||
| <50 | 0.2 | 0.3 | <0.0001 | 0.2 | 0.3 | <0.0001 |
| ≥50 and <70 | 0.4 | 0.5 | 1.2 | 1.9 | ||
| ≥70 and <100 | 30 | 38.4 | 66.4 | 89.1 | ||
| 100 | 69.2 | 60.7 | 32.1 | 8.6 | ||
| Preprocedure TIMI flow | ||||||
| 0 | 68.5 | 59.2 | <0.0001 | 32.7 | 8.4 | <0.0001 |
| 1 | 10.7 | 11.2 | 11.6 | 8.5 | ||
| 2 | 10.9 | 14.6 | 19.2 | 20.1 | ||
| 3 | 9.7 | 14.8 | 36.3 | 62.8 | ||
| Coronary thrombus | 55.1 | 50.1 | <0.0001 | 23.2 | 6.5 | <0.0001 |
| Postprocedure TIMI flow | ||||||
| 0 | 2.3 | 1.4 | <0.0001 | 2.4 | 0.7 | <0.0001 |
| 1 | 1.5 | 0.6 | 1.3 | 0.2 | ||
| 2 | 4.6 | 2.7 | 2.9 | 0.9 | ||
| 3 | 89.4 | 93.9 | 88.9 | 96.4 | ||
Unadjusted mortality was significantly higher in patients with CA both in the STEMI and in the without STEMI groups ( Table 3 ). Complications including postprocedure renal failure, stroke, bleeding events, and need for blood transfusions were significantly more common in patients with CA.
| Variables | STEMI | Without STEMI | ||||
|---|---|---|---|---|---|---|
| CA (n = 9,375) | No CA (n = 105,393) | p Value | CA (n = 2,775) | No CA (n = 477,191) | p Value | |
| Death | 24.9 | 3.1 | <0.0001 | 18.7 | 0.4 | <0.0001 |
| Cerebrovascular accident/stroke | 1.2 | 0.5 | <0.0001 | 0.9 | 0.1 | <0.0001 |
| Renal failure | 1.6 | 0.4 | <0.0001 | 1.8 | 0.1 | <0.0001 |
| Bleeding event within 72 h | 7.8 | 3.8 | <0.0001 | 5.2 | 1.3 | <0.0001 |
| RBC/whole blood transfusion | 12.6 | 5 | <0.0001 | 10.6 | 1.4 | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


