Catheter-associated Upper-extremity Deep Venous Thrombosis
JimBob Faulk
Marc A. Passman
While lower-extremity venous thrombosis is well described, upper-extremity venous thrombosis has traditionally been viewed as rare and of uncertain clinical significance. Although there are several potential causes of upper-extremity venous thrombosis, catheter-associated venous thrombosis is the most common etiology that parallels increased medical care requiring central venous access. Upper-extremity venous access using catheters directed into the central venous circulation is a mainstay of both inpatient and outpatient care, and it provides access for laboratory blood draws, delivery of medications, central venous monitoring, parenteral nutrition, and hemodialysis. However, central venous catheters are not without problems. While most attention is directed at reduction of catheter-related infection, upper-extremity catheter-associated venous thrombosis is becoming a significant clinical problem. Catheter-associated upper-extremity venous thrombosis has been reported to range from 3% to 72% of catheter placements, although most of these never reach clinical attention. While most hospitals adhere to strict guidelines to reduce the risk of catheter-related infections, protocols are beginning to develop aimed at decreasing potential catheter-induced venous thrombosis. In addition, more aggressive treatment strategies are being employed than in the past to maintain central venous access when upper-extremity venous thrombosis does occur.
Pathogenesis
Upper-extremity venous thrombosis has been traditionally divided into two broad categories. Primary upper-extremity venous thrombosis typically refers to the “effortrelated” thrombosis or the Paget-von Schrötter syndrome. Secondary upper-extremity venous thrombosis refers to the vast majority of cases where a causative agent is identified. Patients with no identifiable cause are termed idiopathic, and in the past have been generally included in the primary group. However, it is now commonly accepted that nearly all instances of upper-extremity venous thrombosis are secondary to some underlying cause, whether it be catheter-related, hypercoagulable condition(s), underlying malignancy, infection, or an anatomic abnormality, as in the case of Paget-von Shrötter syndrome. Central venous catheters are by far the most common cause of secondary upper-extremity venous thrombosis.
As noted by Virchow, thrombosis occurs in the setting of vessel injury, alterations in flow (stasis), and perturbations in the coagulation state. Central venous catheters as a foreign body positioned in the central venous circulation contribute to all of these factors. The characteristics of the infusate (pH, osmolarity, and amino acids) also contribute to inducing venous thrombosis. Silicone and polyurethane catheters appear to be less thrombogenic than polyvinyl chloridecoated catheters. This is secondary to the stiff properties of polyvinyl chloride, which are thought to induce a larger degree of vessel injury when compared to the more pliable compounds found in silicone and polyurethane catheters. Larger catheters that are in place for extended periods of time are associated with higher rates of venous thrombosis.
The location of the thrombus depends somewhat on the patient’s anatomy and catheter-related history. Thrombus is more likely to progress from the site of vessel injury than from a site removed from injury. With multilumen “over-the-wire” central venous catheters and long peripherally inserted central catheters (PICCs), the site of maximal vessel injury or denuded endothelium is not always close to the site of percutaneous entry. For PICCs, upper-extremity venous thrombosis may not become evident until thrombus propagates into the axillary or subclavian veins. In the absence of propagation or septic thrombophlebitic complications, thrombus within the superficial vein at the site of insertion is rarely of clinical significance. The presence of a large number of venous collaterals in the upper extremities and chest contributes to the relatively quick resolution of symptoms when compared to the lower extremities (Fig. 71-1).
While the rate of post-thrombotic symptoms with upper-extremity venous thrombosis is widely debated, symptoms are less prevalent than they are with lower-extremity venous thrombosis. The lower extremities are subjected to the effects of gravity, venous pooling, and immobility to a larger degree than the upper extremities are. Because of the extensive collateral network, even in the presence of post-thrombotic valvular incompetence, the upper extremities are less likely to be symptomatic.
Clinical Presentation
Most patients with upper-extremity venous thrombosis are asymptomatic. Often the first suggestion of a catheter-associated UEDVT is a catheter malfunction. Most symptomatic presentations are a result of thrombosis within the axillary or subclavian veins
ipsilateral to the site of catheter insertion. Generalized extremity pain and edema are the most common complaints. Other symptoms include extremity numbness, heaviness, and coolness. Physical findings include limb edema, cyanotic discoloration, prominent venous collaterals, tenderness, and warmth. The clinical exam is highly unreliable, with only 50% of symptomatic patients actually having venous thrombosis. Because of this lack of reliability, objective testing is needed for confirmation.
ipsilateral to the site of catheter insertion. Generalized extremity pain and edema are the most common complaints. Other symptoms include extremity numbness, heaviness, and coolness. Physical findings include limb edema, cyanotic discoloration, prominent venous collaterals, tenderness, and warmth. The clinical exam is highly unreliable, with only 50% of symptomatic patients actually having venous thrombosis. Because of this lack of reliability, objective testing is needed for confirmation.
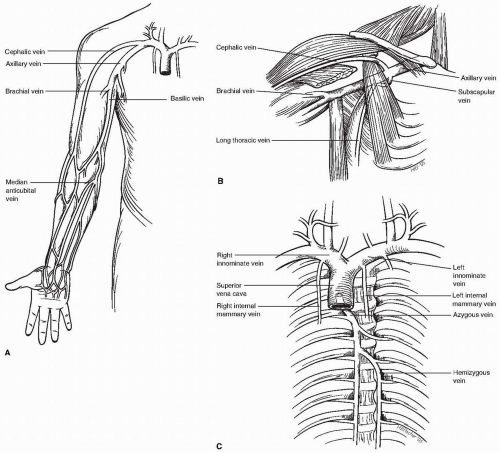 Figure 71-1. The vast array of venous collaterals in the upper extremities allows for easy venous access and adequate extremity venous compensation in the presence of venous thrombosis. |
Potentially life-threatening presentations rarely occur but deserve specific mention. Pulmonary embolism from thrombus requires prompt recognition. Dyspnea, pleuritic chest pain, hypoxia, hemodynamic instability, or other factors with a high clinical suspicion should be evaluated further. Catheter-associated thrombus that propagates to involve the superior vena cava can also cause superior vena cava syndrome. Bilateral upper-extremity swelling, plethora, upper-extremity cyanosis, or facial edema should raise suspicion for this condition. Venous gangrene is an exceedingly rare but life-threatening complication following massive extremity venous thrombosis and is most commonly seen in the context of malignancy. The extremity appears edematous, blanched, cyanotic, and mottled, and this can progress to critical limb ischemia and necrosis.
Diagnostic Considerations
Venous duplex ultrasound is the initial screening diagnostic test that should be obtained. Real-time B-mode ultrasonography
coupled with color or pulsed-wave Doppler allows for accurate interrogation of upper-extremity and central venous anatomy. Compressibility and augmentation maneuvers yield sensitivities and specificities in the 95th percentile. Normal upper-extremity veins should have phasic flow and be compressible when visualized. Abnormal findings are suggested by noncompressibility, absence of venous phasicity, and lack of augmentation of flow with distal compression maneuvers. When venous thrombus is present, differences in echogenicity can help distinguish acute from chronic thrombus, with chronic thrombus appearing more echogenic and heterogeneous compared to acute thrombus. Limitations of upper-extremity venous duplex ultrasonography include inability to visualize and compress around the clavicle and within the thoracic cavity. While venous duplex ultrasound is somewhat technician dependent, advances in the technology and standardized accreditation have made it more reliable and reproducible.
coupled with color or pulsed-wave Doppler allows for accurate interrogation of upper-extremity and central venous anatomy. Compressibility and augmentation maneuvers yield sensitivities and specificities in the 95th percentile. Normal upper-extremity veins should have phasic flow and be compressible when visualized. Abnormal findings are suggested by noncompressibility, absence of venous phasicity, and lack of augmentation of flow with distal compression maneuvers. When venous thrombus is present, differences in echogenicity can help distinguish acute from chronic thrombus, with chronic thrombus appearing more echogenic and heterogeneous compared to acute thrombus. Limitations of upper-extremity venous duplex ultrasonography include inability to visualize and compress around the clavicle and within the thoracic cavity. While venous duplex ultrasound is somewhat technician dependent, advances in the technology and standardized accreditation have made it more reliable and reproducible.
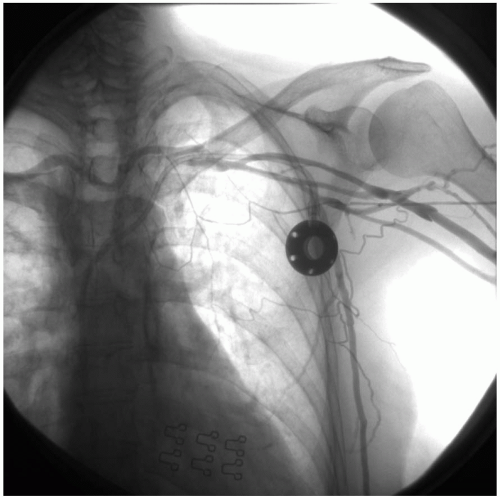 Figure 71-2. Contrast venogram via a left median antecubital injection demonstrating occlusion of the left subclavian vein at the site of a chronic indwelling central venous access port insertion. |
Contrast venography is still considered the “gold standard” for diagnosis, and unlike other modalities, it offers some therapeutic options. It is performed by injection of an iodinated contrast agent via a peripheral vein in the extremity of concern (Fig. 71-2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


