Carotid Body Tumors
THOMAS C. BOWER
Presentation
A 58-year-old man is referred to you by his primary care physician for evaluation of slowly enlarging bilateral neck masses. The patient has sporadic mild pain in the upper right neck. He has a 50-pack-year history of smoking and drinks occasional alcohol. He has developed moderate hypertension over the past year, controlled with two medications. He has not had palpitations or other cardiac problems. He has some occupational hearing loss, but no dysphagia, odynophagia, or visual changes. He has a morning cough but has not had fevers or a sore throat. He believes an aunt may have had some type of neck tumor. On physical examination, he has a regular heart rate of 95 beats per minute and a blood pressure of 140/86 mm Hg. The thyroid gland is mildly enlarged. There is a 3-cm immobile mass high in the right neck and a 2-cm mass in the mid left neck just below the angle of the jaw. The left neck mass can be moved laterally but not vertically. Carotid and upper extremity pulses are normal. No bruits or thrills are present in the neck. There is mild erythema in the posterior pharynx but no ulcerations or masses. There are no cardiac murmurs. There are a few coarse rhonchi on auscultation of the lungs. Neurologic examination is within normal limits, including cranial nerves.
Differential Diagnosis
The differential diagnosis for an anterior neck mass in an adult male includes benign and malignant thyroid tumors; adenopathy from metastatic head and neck cancer; tumors of the salivary gland, larynx, or parathyroid; lymphadenitis or lymphoma; and carotid body tumor or carotid aneurysm. The most likely diagnosis in this patient is carotid body tumors (CBTs). Most CBTs can be moved laterally but not in a cranial-caudal direction (Fontaine’s sign). They are not expansile like an aneurysm. While the tumors are hypervascular, only 40% of patients have a bruit over the mass. Chronic hypoxemia may play a role in their development.
Evaluation
A complete blood count with differential and thyroid-stimulating hormone level are normal. A color flow duplex ultrasound scan of the neck shows a normal thyroid gland, mildly enlarged cervical lymph nodes with fatty centers, and three masses in the neck, two on the right side and one on the left. The larger upper right neck mass cannot be fully imaged, measures about 3.5 cm but looks solid. The remaining masses splay each carotid artery bifurcation, are hypervascular, and measure between 2 and 2.5 cm in maximum diameter. The common, internal, and external carotid artery velocities are normal.
These findings are suspicious for bilateral carotid body tumors. The upper right neck mass is indeterminate but could represent a vagal tumor or a paraganglioma of the cervical sympathetic chain. While CBTs in most patients are sporadic (75%), the bilateral CBTs, and a relative with a neck tumor in this patient, suggest a familial syndrome.
Approximately 20% to 25% of patients have a family history of paragangliomas, and the tumors may be multicentric. CBT carries a low risk of malignancy. Even though patients rarely present with symptoms, such as headaches, flushing, or palpitations, the presence of bilateral tumors in this man, and a possible family history, warrant additional biochemical, genetic, and radiologic tests.
Biochemical testing is done with a 24-hour urine collection for metanephrines and catecholamines. Succinyl dehydrogenase subunit mutations are common in patients with bilateral tumors and/or a family history. A Mayo Clinic study found 94% of patients with a positive family history and 71% with bilateral tumors to have a genetic mutation. These include subunits SDHB on chromosome 1p35-36 and SDHD on chromosome 11q23. Importantly, metachronous paragangliomas occur in one third of patients with a genetic mutation, which emphasizes the importance of surveillance studies in this subset.
Radiologic imaging is done with 123I-metaiodobenzylguanidine scintigraphy, or CT or MRI studies of the chest and abdomen to exclude other paragangliomas. CT angiography of the head and neck provides better anatomic detail about tumor location, its superior and medial extent, size, volume, and characterization than ultrasonography. In this patient with multiple tumors, the ultrasound study did not fully image the tumors, so CTA would be very useful.
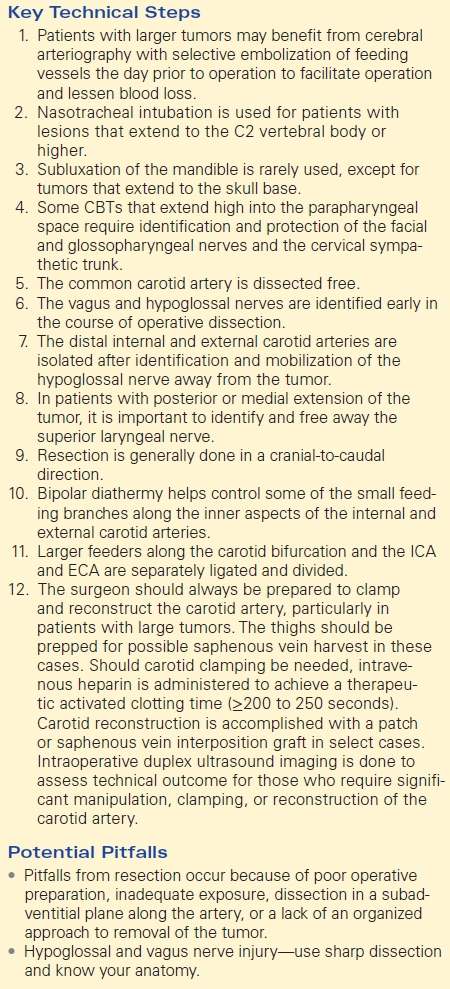
Size, volume, and anatomic location referable to the angle of the mandible and the upper cervical vertebrae on the CTA determine risk of operation, including injury to adjacent cranial nerves. Ease of resection can be predicted by the Shamblin classification of the tumor (Fig. 1). This classification is determined by the preoperative imaging studies, the operative findings, and pathologic analysis. Class I tumors are localized to the carotid bifurcation and easily resected. Class II tumors partially surround the external and internal carotid arteries but may be adherent to them. Class III tumors completely encase at least one of the arteries and are the most difficult to resect. In general, the larger the tumor size and the more encased the internal carotid artery is, the more difficult the operative resection, the higher the risk of cranial nerve injuries, and the greater the potential need to replace or patch the artery.
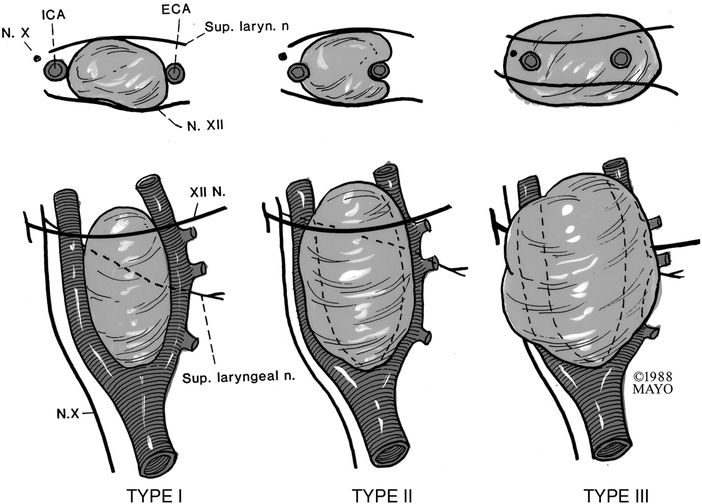
Figure 1 The Shamblin classification of carotid body tumors predicts the difficulty of surgical resection. Class I tumors are localized and easily resected. Class II tumors adhere to or partially surround the carotid arteries. Class III completely surround or encase at least one of the arteries. (ECA, external carotid artery, ICA, internal carotid artery.) (Reprinted with permission from the Mayo Clinic and Hallett JW Jr et al.)
Surgical Approach
This patient proved to have nonfunctioning tumors, all isolated to the neck. The SDH genetic analysis was positive, and additional family members were scheduled to be screened. CT imaging of the chest and abdomen showed no other paragangliomas. Select images of the CT of the head and neck are shown in Figure 2. The next steps are planning and executing the operation.
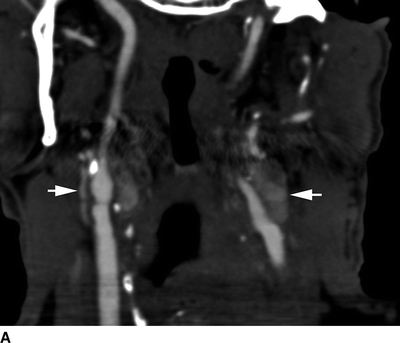
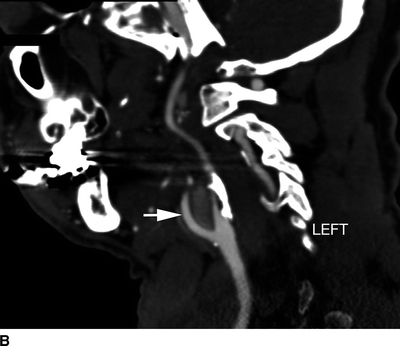
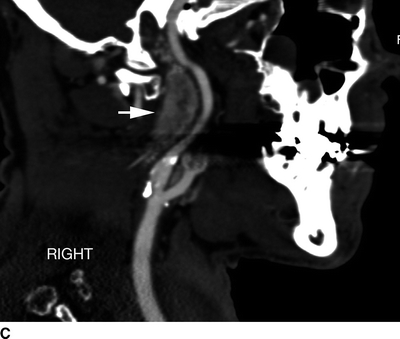

Figure 2 Select AP and sagittal CT angiographic images of the patient. A and B show the 2.5-cm carotid body tumors at each carotid bifurcation. Image C shows a sagittal image of the superior extent of the 5-cm vagal tumor high in the right neck. Image of the right carotid artery during cerebral arteriography at the time of embolization of the larger upper right neck tumor (D).
Surgical considerations and patient counseling include the need to embolize the tumor, the risk of cranial nerve injury, the side to treat, and operative preparations. Most tumors less than 3 to 4 cm in diameter or 20 cm3 can be resected without adjuncts, such as embolization. Patients with larger tumors may benefit from cerebral arteriography with selective embolization of feeding vessels the day prior to operation to facilitate operation and lessen blood loss. Most of the arterial feeders originate from the external carotid artery, particularly, the ascending pharyngeal branch (Fig. 2D). The goal of embolization is to decrease tumor vascularity as much as safely possible. While intuitively it might seem that the risk of cranial nerve injuries would be lower if the tumor shrinks and it is less vascular, that has not been a consistent correlation. In the Mayo Clinic report, tumor embolization was safe with no patient sustaining a transient ischemic attack, stroke, or access-site complication in 33 patients treated from a cohort of 131 who had CBT resection. Embolization allowed for a significantly higher number of simple excisions, less need for temporary carotid clamping, and lower blood loss than those not treated by preoperative embolization. However, cranial nerve injuries were no different between the two groups.
The risk of stroke during tumor excision is exceedingly low in experienced hands. Nonetheless, cranial nerve injuries remain problematic for patients with large tumors (Shamblin III). For this reason, most good-risk patients are considered for surgical resection, unless a tumor has been nonfunctional and stable in size for years and the patient is old (greater than 70 to 80 years), or rarely if the tumor is large and asymptomatic but when surgical resection risks significant disability from cranial nerve injuries. Although nerve injuries occur in one third of patients or more with large tumors, the permanent cranial nerve deficits that are clinically evident 1 year after resection was only 6% in the Mayo Clinic series. The most common temporary nerve injuries were the marginal mandibular branch of the facial nerve (13%) and the hypoglossal nerve (12%).
The primary cranial nerve injury in this patient may be to the vagus nerve, given that the upper right neck tumor could originate from that nerve.
There is some controversy regarding which tumor should be resected first. One approach is resection of the larger tumor first, as this may pose the greatest threat to the patient. Should the individual sustain a cranial nerve injury, the smaller contralateral tumor can be either observed or treated by alternative means, such as radiation therapy. Significant growth of the contralateral tumor occurs in less than 10% of patients with bilateral carotid body tumors who only have unilateral resection. Other surgeons suggest resection of the smaller tumor first, because of the lower risk of cranial nerve injuries. In this way, if a cranial nerve injury occurs after the second operation to remove the larger CBT, both sides will have been treated.
Nasotracheal intubation is used for patients with lesions that extend to the C2 vertebral body or higher. Subluxation of the mandible is rarely used, except for tumors that extend to the skull base. Tumor extension into the skull mandates input from neuro- or otorhinolaryngologic surgeons with expertise in dealing with such lesions. Surgical assistance from an experienced head and neck cancer surgeon is beneficial to free cranial nerves in patients with large tumors located high in the neck. Some CBTs that extend high into the parapharyngeal space require identification and protection of the facial and glossopharyngeal nerves and the cervical sympathetic trunk. Electroencephalography is often used. The key steps of the operation are as follows. The common carotid artery is dissected free. The vagus and hypoglossal nerves are identified early in the course of operative dissection. The distal internal and external carotid arteries are isolated after identification and mobilization of the hypoglossal nerve away from the tumor. In patients with posterior or medial extension of the tumor, it is important to identify and free away the superior laryngeal nerve. Resection is generally done in a cranial-to-caudal direction. Bipolar diathermy helps control some of the small feeding branches along the inner aspects of the internal and external carotid arteries. Larger feeders along the carotid bifurcation and the ICA and ECA are separately ligated and divided.
Temporary arterial clamping is needed in less than one fourth of patients, and only 10% will need some type of carotid artery reconstruction. However, the surgeon should always be prepared to clamp and reconstruct the carotid artery, particularly in patients with large tumors. The thighs should be prepped for possible saphenous vein harvest in these cases. Should carotid clamping be needed, intravenous heparin is administered to achieve a therapeutic activated clotting time (≥200 to 250 seconds). Carotid reconstruction is accomplished with a patch or saphenous vein interposition graft in select cases. Intraoperative duplex ultrasound imaging is done to assess technical outcome for those who require significant manipulation, clamping, or reconstruction of the carotid artery.
Pitfalls from resection occur because of poor operative preparation, inadequate exposure, dissection in a subadventitial plane along the artery, or a lack of an organized approach to removal of the tumor (Table 1).
TABLE 1. Carotid Body Tumor