Carotid Artery Stent/Neck Approach/Difficult Arch
LINDA WANG and CHRISTOPHER J. KWOLEK
Presentation
A 74-year-old female is referred by another vascular surgeon for a second opinion concerning the management of a critical right internal carotid artery (ICA) stenosis. She denies any focal motor or sensory deficits, speech difficulties, or visual changes. The patient is 14 years status post resection of a right-sided tonsillar carcinoma with chemoradiation. Her past medical history is significant for diabetes, hypertension, and hyperlipidemia. She is a nonsmoker and currently taking aspirin 81 mg/d, simvastatin 20 mg/d, and metformin 500 mg twice a day. On physical examination, the patient is a well-appearing Caucasian female who looks her stated age. Vital signs are notable for a regular pulse of 70 beats per minute, blood pressure of 152/67 mm Hg in the left arm and 168/75 mm Hg in the right arm, and a respiratory rate of 16. Her physical examination is significant for a right carotid bruit, palpable carotid pulses bilaterally, and well-healed scar tissue from previous neck surgery and radiation. Her neurologic exam is intact.
Differential Diagnosis
Any patient with a history of neck radiation is at risk for developing ipsilateral carotid artery stenosis. This patient’s history of radiation 14 years prior puts her at high risk for developing radiation-induced vascular disease. She additionally has cardiovascular risk factors, such as hypertension and hyperlipidemia, which put her at increased risk for developing atherosclerotic disease.
Workup
It is important to know about cardiovascular risk factors in patients presenting with carotid artery stenosis. More specifically, a history of diabetes, hyperlipidemia, myocardial infarction, stroke, a positive family history of premature atherosclerosis, and smoking are particularly pertinent. A full neurologic and pulse examination should be performed in any patient presenting with carotid artery disease.
Carotid duplex examination should be used to evaluate for the presence of calcification and thrombus as well as for the degree of stenosis by measuring elevation in peak systolic velocity (PSV) and end diastolic velocity (EDV). In the present case, ultrasound demonstrates a severe right ICA stenosis with a PSV of 506 cm/s, EDV of 228 cm/s, and ICA to common carotid artery (CCA) ratio of 10.4 as shown in Figure 1. She had no significant left-sided stenosis.
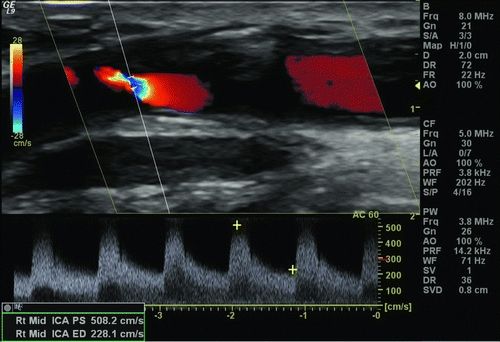
Figure 1 Preoperative carotid duplex ultrasound demonstrating severe right ICA stenosis.
Computed tomography angiography (CTA) can help define arch anatomy and disease, vessel tortuosity, calcification, and intracranial disease. CTA to evaluate these characteristics in patients being considered for carotid artery stenting (CAS) is routinely used. This patient’s CTA is shown in Figure 2. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) can also be used for evaluation of arch and cerebral vessels as well as to evaluate for acute and chronic stroke.
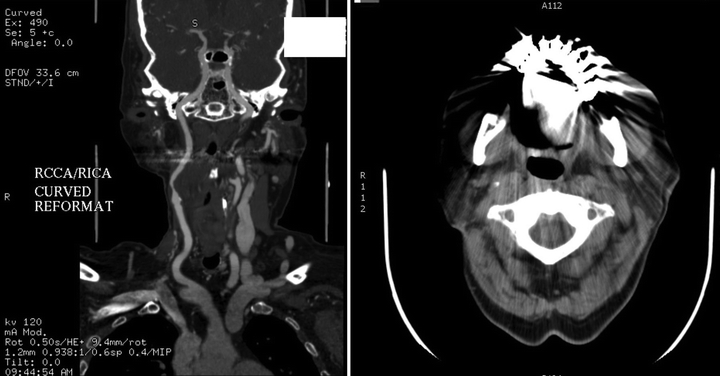
Figure 2 CTA demonstrating critical right ICA stenosis.
Diagnosis and Treatment
The patient has a critical right ICA stenosis. One option for treatment would involve open surgical exploration with a carotid artery endarterectomy (CEA) or a carotid artery interposition grafting. However, there are several things to consider in a patient who has undergone prior radiation and/or dissection. Radiation induces skin changes that can compromise nutrient delivery and therefore affect wound healing. Scar tissue from previous dissections can complicate subsequent open procedures and also increases the risk of nerve injury.
Carotid angioplasty and stenting is therefore a reasonable alternative. Minimizing the risk of stroke during this procedure is of the utmost importance. Transfemoral carotid stenting has been shown to have a higher incidence of new microembolic lesions on diffusion-weighted MRI when compared to proximal carotid artery occlusion with flow reversal. However, the current commercially available proximal balloon occlusion systems require placement through a 9-French femoral sheath and can significantly increase the risk of embolic events in patients with tortuous and diseased aortic arches. Direct CCA access via a supraclavicular incision with proximal occlusion and flow reversal was thus developed to overcome these limitations.
To minimize the risk of periprocedural stroke and embolization, the patient should be started on aspirin, clopidogrel, and a statin 3 to 5 days before the intervention if the patient is not already taking those medications.
Surgical Approach
Direct cervical carotid access with flow reversal was designed to combine the advantages of both CEA and CAS by pairing direct carotid access with proximal occlusion and flow reversal to provide embolic protection during stenting. In contrast to traditional CAS, the procedure starts at the neck instead of the groin. Direct carotid access is intended to minimize the risk of microemboli and stroke associated with arch navigation.
The procedure is done under local anesthesia and minimal sedation to be able to assess intraoperative neurologic status. The patient is pretreated with glycopyrrolate to prevent procedure-induced cardiac vagal reflexes. An ultrasound is performed to confirm the length from the clavicle to the carotid bifurcation (minimum of 5 cm), to identify the depth of the CCA, and to identify a potential puncture site free from calcification and thrombus. Control of the CCA is accomplished through a small transverse incision above the clavicle with placement of a Rummel tourniquet or vessel loop.
A 5-0 prolene suture is placed as a U-stitch in the anterior wall of the CCA. The patient is systemically heparinized to maintain an activated clotting time (ACT) greater than 250 seconds, and a micropuncture needle is introduced through the U-stitch into the CCA. Angiography is then performed to confirm a greater than or equal to 80% stenosis and locate the lesion (Fig. 3A). An Amplatz Super Stiff wire with a 1-cm floppy tip is introduced into the CCA while staying below the level of the lesion. The entry site is then dilated with an 8-French dilator. The flow reversal cannula is introduced 2.5 cm into the CCA (Fig. 4A), and cervical and intracranial angiograms are performed.


Figure 3 Intraoperative angiography demonstrating critical right ICA stenosis (A) and completion angiogram after CAS (B).



