Fig. 8.1
The major vessels of the head and neck. The arch of the aorta gives rise to the innominate, left common carotid, and left subclavian arteries. The innominate bifurcates to form the right common carotid and right subclavian arteries. The common carotid artery bifurcates to form the left internal carotid and left external carotid
The external carotid artery is located medial and anterior to the internal carotid artery and terminates as the maxillary artery and superficial temporary artery. Additional branches include the superior thyroid artery, facial artery, occipital artery, and posterior auricular artery. Located posterior to the external carotid artery is the glossopharyngeal nerve [1]. The external carotid artery is the primary blood supply to the face, but due to the presence of extensive collaterals from the contralateral side, ligation of the external carotid artery can often be completed with impunity.
The internal carotid artery can be divided into seven distinct segments according to the Bouthillier classification: the cervical, petrous, lacerum, cavernous, clinoid, supraclinoid, and terminal segments [2]. At the bifurcation of the common carotid artery is the carotid bulb, which contains the carotid sinus and carotid body. The carotid sinus contains chemoreceptors that detect carbon dioxide and acidosis. The carotid body contains mechanoreceptors and baroreceptors that lead to bradycardia and vasodilation when stimulated. The internal carotid artery is the primary blood supply to the brain; ligation of the internal carotid artery can lead to stroke in up to 40 % of patients due to an incomplete circle of Willis [1].
The vertebral artery is the first branch of the subclavian artery and provides circulation to the posterior brain and collateral flow via the circle of Willis. The vertebral artery initially travels anterior to the transverse process of C7 (segment V1) and then within the transverse foramina until it reaches C1 (segment V2). It then travels posterior to the arch of the atlas (segment V3), enters the vertebral canal (segment V4) then passes through the foramen magnum where the vertebral arteries combine to form the basilar artery. In rare circumstances, the vertebral artery may terminate directly into the posterior inferior cerebellar artery, a condition known as PICA syndrome. Ligation of the vertebral artery in this case may lead to infarction of the posterior inferior cerebellum [1].
8.3 Penetrating Injuries to the Vascular Structures of the Neck
It is impossible to talk about penetrating vascular trauma of the neck region without discussing also the evaluation and management of aerodigestive injuries. Therefore, these injuries will also be mentioned in this focus on penetrating vascular trauma.
8.3.1 Evaluation
All patients with penetrating trauma to the neck must be treated initially according to the principles of Advanced Trauma Life Support (ATLS):
Airway: The airway must be patent and the patient must be able to control it. If not, the patient will require oral endotracheal intubation; depending on the injury, cricothyroidotomy may be necessary, or if the trachea has been severed, a tube can be inserted into it. The threshold for airway control must be lower in the setting of neck trauma, as progressive soft tissue swelling or expanding hematoma may compromise the patency of the airway.
Breathing: Injuries to the neck can also cause injury to the pleura; therefore, pneumothorax must be ruled out by physical exam and chest x-ray if needed.
Circulation: Take note of pulses, but especially with penetrating neck injuries, stop the bleeding by applying direct pressure to the area.
Disability: Assess the ability to move all four extremities and Glasgow Coma Score (GCS). It is crucial to know if a patient already demonstrates signs or symptoms of ischemic neurologic deficit.
After this primary survey is completed, the secondary survey is performed, noting which zone of the neck the injury is located. A laceration must traverse the platysma muscle to be classified as a true penetrating injury. If the injury does not traverse the platysma, it is considered a superficial injury and no further evaluation needs to be done. Penetrating injuries to the anterior neck between the sternocleidomastoid muscles are more likely to cause significant vascular or aerodigestive injury as compared to the side and posterior portions of the neck. The anterior neck between the sternocleidomastoid muscles is divided into three zones. Beginning caudad, zone 1 is from the sternal notch and clavicles to the cricoid cartilage (Fig. 8.2). Zone 2 is from the cricoid cartilage to the angle of the mandible. Important structures at risk in both zones 1 and 2 are the trachea, esophagus, and carotid and vertebral arteries. Zone 3 is from the angle of the mandible to the base of the skull. Important structures at risk in zone 3 are the carotid and vertebral arteries.
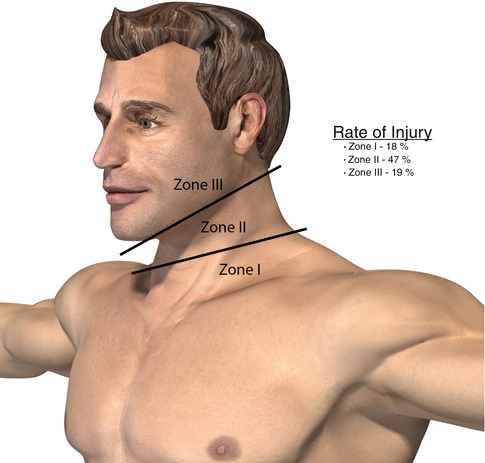
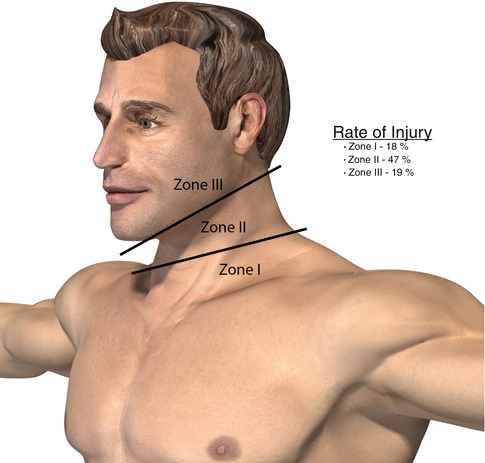
Fig. 8.2
The three zones of the neck. Zone I is located below the cricoid cartilage. Zone II is located between the cricoid cartilage and the angle of the mandible. Zone III is located above the angle of the mandible. Injury to zone I occurs in about 18 % of patients with neck trauma, zone II injuries occur in 47 %, and zone III injuries occur in 19 %
8.3.2 History and Exam
Important subjective findings of penetrating neck trauma are pain, dysphagia, and change in voice. Objective findings specific for vascular injury are active hemorrhage, hematoma, and presence of a bruit. Objective findings specific for a trachea or esophagus injury are crepitus, air coming from the wound, and subcutaneous emphysema. These findings are traditionally characterized as “soft” or “hard” signs of injury. Hard signs include active bleeding or shock from blood loss, expanding or pulsatile hematoma, air bubbling through the injury site, hemoptysis, and/or extensive subcutaneous emphysema. Hard signs indicate a surgical emergency and thus mandate immediate operation. Soft signs include dysphagia, voice change, venous oozing, and nonexpanding or nonpulsatile hematoma. Soft signs may be safely observed, at least for a short time to allow for further evaluation with imaging and procedures.
8.3.3 Initial Imaging
Initial imaging may or may not be indicated. A chest x-ray may be performed to look for a pneumothorax or other injury. Plain films of the neck are rarely done and will only be useful if a fracture of the cervical spine is suspected. Patients with “hard” signs for neck injury will require an immediate chest x-ray to evaluate for thoracic trauma and assist with operative planning and treatment. Plain films of the neck are rarely performed but are useful to rule out a fracture of the cervical spine and assist with cervical collar removal to facilitate positioning and neck exploration. Penetrating injury with “soft” signs for cervical injury will best be evaluated by computed tomography angiography (CTA) of the neck.
8.3.4 Management
Any patient with penetrating neck trauma to any zone with hard signs of vascular injury should go immediately to the operating room for neck exploration. Hard signs by definition indicate an injury that requires surgical repair. However, there is a possible exception to this. If a patient has a penetrating injury to zones 1 and 3 and if the patient is not in shock, a CTA of the neck and upper chest may show a “road map” of injury to better plan the operative approach.
Patients with soft signs or no signs at all can be managed in a few different ways. A traditional algorithm called for all zone 2 injuries to be explored in the operating room. This approach is based partially on the fact that injuries in zone 2 are amenable to straightforward, though not mandatory exploration, unlike zones 1 and 3 which are not as easily explored. In this algorithm, zone 1 injuries are evaluated by CTA to evaluate for a great vessel injury in the chest or in the carotid arteries in the neck, followed by whatever combination of esophagoscopy, bronchoscopy, and esophagram is necessary to evaluate for an aerodigestive injury. Finally, zone 3 injuries are worked up by CTA to evaluate the vasculature; there is no need to evaluate the aerodigestive structures here because it is only the oropharynx there and it is not under any pressure because it is superior to the cricopharyngeus.
Tracheal injury can be evaluated by physical exam or bronchoscopy. Esophageal injury can be evaluated by barium esophagram and/or esophagoscopy. Recent literature highlights the accuracy of either study alone—i.e., endoscopy for intubated patients and esophagography for awake patients [3]. Arterial vascular injury is best evaluated by CTA, preferably a minimum of 64 slices. CTA has also been used to evaluate for aerodigestive injuries. One prospective study found that CTA was 100 % sensitive and 97.5 % specific for detecting clinically significant aerodigestive or vascular injuries [4].
8.3.5 Management of Specific Penetrating Vascular Injuries
8.3.5.1 Venous
At neck exploration, bleeding from the external or internal jugular veins is common and these vessels may be ligated with impunity. If the internal jugular vein has a minor injury, then consider repair via lateral venorrhaphy with 5-0 or 6-0 Prolene. If both jugular veins are injured, consider repairing one of the injured vessels not associated with a carotid artery repair suture line.
8.3.5.2 Carotid Artery Injuries
Injuries to the carotid artery are subdivided into the common carotid, external carotid, and internal carotid artery. In general, injuries to the carotid artery can be dealt with using ligation, primary repair, patch, or interposition grafting. Surgical exposure of the common carotid, external carotid, and internal carotid arteries can be accomplished via a longitudinal incision anterior to the medial border of the sternocleidomastoid muscle after positioning the patient supine with a roll under the shoulder to extend the neck and the head turned away from the site of injury (Fig. 8.3). The dissection continues through the platysma, then the SCM is retracted laterally. The carotid sheath is identified and incised, with the internal jugular vein retracted laterally. The site of injury of the carotid artery should be identified and proximal and distal control established. Clamping of the vessels should proceed first with the internal carotid artery, followed by the common carotid and external carotid arteries to avoid dislodging plaque into the brain. If the patient’s other injuries permit, therapeutic heparin should be administered prior to clamping these vessels.


Fig. 8.3
Incision for neck exploration. A longitudinal incision turned posterior under the ear is made medially along the anterior border of the sternocleidomastoid
Injuries involving the internal carotid artery may require extensive dissection into the superior portion of the neck. Better visualization can be achieved by dividing the posterior belly of the digastric and nasotracheal intubation to permit subluxation of the mandible. One of several cerebral protective adjuncts should be utilized whenever blood flow through the internal carotid artery is impeded to identify cerebral ischemia; otherwise, the mandatory use of shunting should be considered. Patients with a back pressure less than 40 mmHg, electroencephalogram changes, changes in neurologic status during awake surgery, or changes in cerebral oximetry are candidates for shunt placement. Extensive exposure of the external carotid artery is rarely necessary, as this vessel can simply be ligated at its takeoff from the common carotid artery in cases where extensive bleeding is present. In cases involving extensive bleeding from the carotid vessels, the use of a temporary occlusive balloon can achieve hemostasis while a more through exposure is completed. Endovascular stent placement across lesions of the common carotid and/or internal carotid arteries can also be completed in selected patients, although long-term results in trauma patients are not available. Exposure of the internal and external jugular veins can also be accomplished in a similar manner.
Trauma to the V1 segment of the vertebral artery may best be treated with ligation of the vertebral artery. A transverse supraclavicular incision at the base of the neck can be made to expose the subclavian artery. The dissection is carried to the subclavian artery by separating the two heads of the sternocleidomastoid muscle, dividing the omohyoid muscle, and identifying the scalenus anticus. The vertebral artery will travel in conjunction with its vertebral vein at this location, and the vessel may be ligated after confirming a satisfactory collateral supply from the contralateral vertebral artery and ruling out PICA syndrome via cerebral arteriography.
Trauma to the V2 segment of the vertebral artery is difficult to repair and often involves ligation of the vessel at the base of the neck. Trauma to the V3 segment can be investigated by completing an incision similar to that of a carotid exposure, with the superior extent being just inferior to the earlobe. The digastric muscle and the proximal portion of the levator scapulae are divided to expose the transverse process of C1, at which point the V3 portion of the vertebral artery can be identified. Trauma to the V4 portion of the vertebral artery is typically self-limiting due to its course within the bony portion of the skull.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


