INDICATIONS
Resection and reconstruction of the carina remains challenging and one of the least common procedures performed in tracheobronchial surgery. In this chapter, we address the single entity: Resection and reconstruction for bronchial stump recurrence following pneumonectomy (Fig. 47.1). The principal indications for carinal resection in such an instance (1): Unanticipated tumor recurrence involving the bronchial stump, occurring months, years, or even decades from the time of pneumonectomy, and (2) a known positive margin resulting from an operation in which a more complete oncologic resection was not done due to unfamiliarity with the procedure of carinal resection, and (2) planned staged procedure with left pneumonectomy and known positive margins. It is helpful to place a pedicled intercostal muscle over the end of the stump to separate from the nearby pulmonary artery stump when approaching from the right chest (3). Carinal resection after pneumonectomy has also been reported for persistent bronchopleural fistula.
Mitchell et al. (2) reported 134 primary carinal resections from 1962 through 1996 and Porhanov et al. (3) reported 231 carinal resections from 1979 to mid-2001, with only 14 patients, or 4%, were noted to have undergone carinal resection for tumor recurrence following pneumonectomy. Despite the uncommon nature of this problem, an excellent outcome can be achieved in the carefully selected patient managed in accordance with the principles outlined below. Indeed, Grillo reported the case of a young woman, who had undergone carinal resection and reconstruction for recurrent carcinoid 14 years following left pneumonectomy and remained disease-free three decades later (4).
 CONTRAINDICATIONS
CONTRAINDICATIONS
This operation should only be undertaken by an experienced team of surgeons, anesthesiologist and intensivists. Especially close cooperation is required between surgeon and anesthesiologist. Operating on the side of the only remaining lung and performing carinal resection may require a variety of techniques to manage the airway and maintain oxygenation. This could include intermittent cross-field ventilation, a high frequency ventilation, cardiopulmonary bypass or ECMO. A careful plan must be established with back-up available.
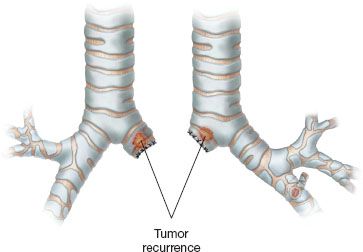
Figure 47.1 Tumor recurrence is depicted in the stump of the bronchus following pneumonectomy.
Careful evaluation of medical comorbidities, metastatic disease, and lung function must be done. Prior mediastinal radiation, high-dose steroids, or previous mediastinoscopy limiting mobility may be relative contraindications. Extensive involvement of the trachea or mainstem bronchi may preclude safe resection and reconstruction. Extensive extraluminal disease and esophageal or left recurrent nerve involvement are likely contraindications to resection.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Careful preoperative planning is essential. Contrast computerized axial tomography with three-dimensional reconstruction has become the preferred radiologic test to evaluate the extent of disease. Barium swallow, PET scans, brain imaging, and magnetic resonance imaging will add to the evaluation in certain instances. Careful endoscopic evaluation by the operating surgeon is essential. Rigid bronchoscopy provides superior optics and precise measurements of the involved airway. The amount of airway that can be resected varies by body habitus, prior operations, radiation, and the side of pneumonectomy. A prior left pneumonectomy allows for greater mobility of the trachea and right mainstem bronchus. A prior right pneumonectomy will have less airway mobility because of scarring and therefore less than can be resected and reconstructed. There is no real rule of thumb but if the distance of trachea and mainstem involvement exceeds 3 to 4 cm, resection is not advisable. Any concern about esophageal involvement should prompt esophagoscopy and endoscopic ultrasound to evaluate involvement.
 SURGERY
SURGERY
Anesthesia
The precise anesthetic technique should be left to the discretion of surgeon and anesthesiologist, working in concert, but the general principles are: Epidural analgesia, invasive blood pressure monitoring, mainstem bronchial intubation (initial endobronchial intubation with an extra long metal reinforced endotracheal tube, augmented by cross-field intubation, if necessary, once the airway is entered), and early extubation in the operating room both to assess the quality of the reconstruction and to avoid the complications attributable to prolonged mechanical ventilation. We do not advocate for the routine use of cardiopulmonary bypass or ECMO in carinal resection and reconstruction, though carinal resection following pneumonectomy is one scenario in which it is potentially of value (5,6). The literature contains at least two case reports, one from Moreno et al. (7) and the other from Lei et al., (8) describing carinal resection for bronchial stump recurrence performed with the assistance of venoarterial ECMO. In each case, the outcome was reported as excellent.
Approach
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


