Figure 10.1
(a, b) The most common type of resection involves the carina and right lung; the reconstruction is perfomed by end-to-end anastomoses between the distal trachea and left main bronchus. Following right lateral thoracotomy in the fourth intercostal space with optional posterolateral extension and opening of the mediastinal pleura, the dissection of mediastinal structures allows assessment of the local tumor extension. This requires division of the azygos vein, with tape passed around the trachea, always keeping in mind the proximity of the left laryngeal recurrent nerve. Upon ventral luxation of the right lung, the posterior aspect of the bifurcation and the main bronchus are exposed. Blunt dissection mobilizes the trachea and left main bronchus. Close attention must be paid to the nutritive vessels reaching the trachea laterally. Ipsilateral mediastinal lymph node resection has to be performed with great care, avoiding devascularization of the trachea and esophagus. After transection and closure of the pulmonary artery and veins—often intrapericardially— the level of resection has to be defined. The safety margin should not be less than 0.5–1 cm; if needed, intraoperative video-endoscopic guidance may be installed. Before opening the tracheobronchial system, the anesthesiologist must retract the endotracheal tube, leaving its tip 2–3 cm cranial to the tracheal incision. At this time, ventilation must be applied using the jet catheter. After transection of the trachea and left main bronchus, the specimen is removed and sent for frozen section. With a special pair of forceps, the jet catheter is then guided into the left main bronchus, which is grasped with traction sutures or a Babcock clamp. The assistant must be constantly alert to aspirate clots and debris from the left bronchial system. (c, d) Control of bleeding of the transection plane should be aimed only at pulsating bronchial arteries, thus preserving the capillaries. A difference in lumen diameter almost always is observed, thus resulting in partially telescoping end-to-end anastomoses. Telescoping should not exceed the breadth of one cartilage ring, and traumatizing the mucosa must be avoided. Several techniques exist for managing the anastomosis; the author prefers the following method: Reconstruction starts along the posterior wall (paries membranaceus). A running suture with absorbable monofilament (4.0 polydioxanone [PDS; Ethicon, Somerville, NJ]) is inserted, avoiding immediate adaption. Single sutures are placed at each end of the running suture surrounding the cartilage of the left main stem as well as of the trachea. Carefully pulling simultaneously at the two single sutures and the running suture results in the final adaption of the posterior wall. Single and running sutures are tied, the knots lying outside the airway. Persistent tension may be neutralized using additional traction sutures placed two to three cartilage rings above and below the anastomoses. Interrupted sutures (4.0 or 3.0 PDS) complete the anastomosis of the anterior portion (paries cartilagineus). Once the anastomosis is completed, ventilation via the jet catheter must be withheld and switched to the tracheal tube. The anastomosis is then exposed to the ventilation pressure, and air leaks can be excluded by underwater testing. Additional coverage of the suture is advised to support the healing process. Intercostal muscle, diaphragm, mediastinal fat including thymic tissue, anterior serrate muscle, pericardium, or pleura may be used. Any leakage may be explained by telescoping exceeding more than one cartilage. In this case, the suture material must be removed and the anastomoses completely reconstructed. If incomplete adaptation due to inadequate traction is causing leakage, a blunt mobilization of the trachea must be extended cranially; simultaneous flexion of the head is helpful. Pledgets may be used as a reinforcement to prevent sutures from cutting through the tracheal wall. If the middle and lower lobes can be preserved, an end-to-side anastomosis of the bronchus intermedius into the left mainstem bronchus or into the trachea is an easy and safe alternative to a side-to-side anastomosis of the bronchus intermedius and left mainstem bronchus and consecutive end-to-end anastomosis with the trachea. The implantation must be performed in the cartilagenous part of the circumference because of the posterior portion’s lack of stability. This anastomosis should be at least 1 cm from the end-to-end anastomosis to avoid interference
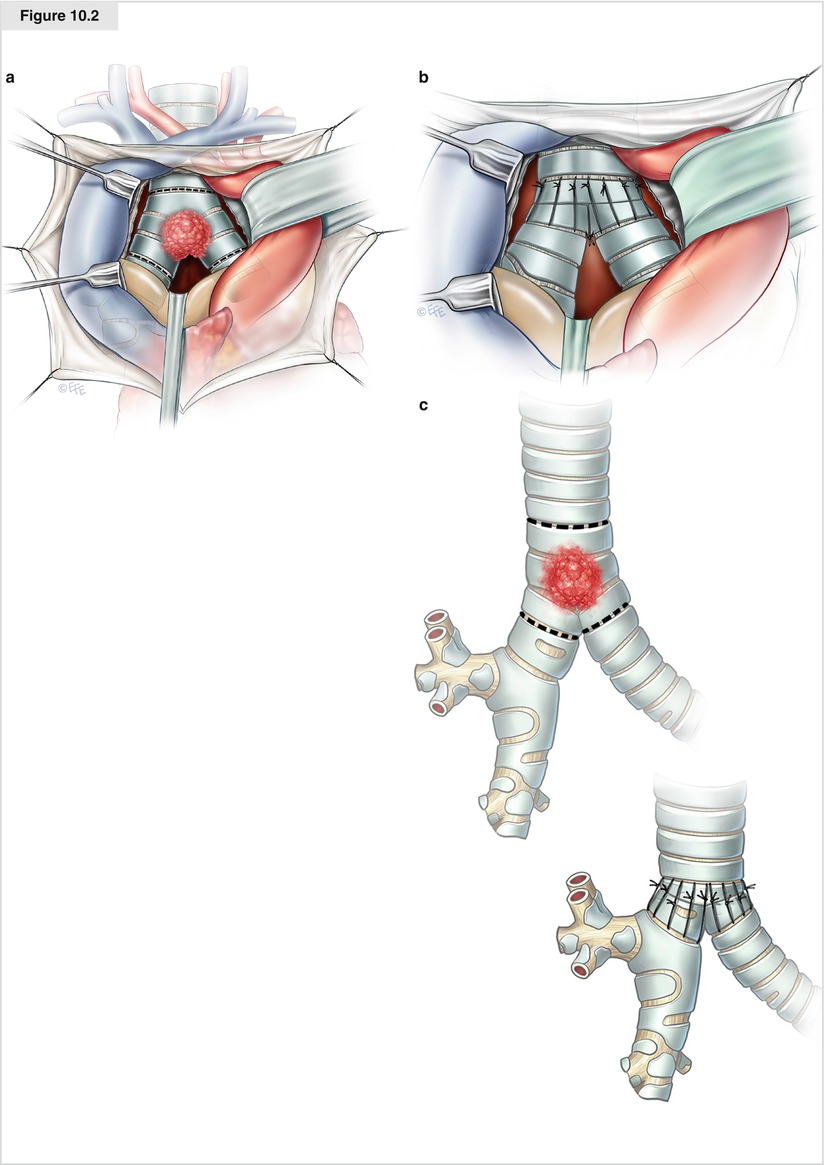
Figure 10.2




(a) In case of limited involvement of the carina, the lung parenchyma may be completely preserved. The best overview of the tracheal bifurcation is obtained through the transsternal, transmediastinal approach. Following approximation of the mainstem bronchi, end-to-end anastomosis with the trachea is performed. Without opening the pleural cavities, only very limited mobilization of the mainstem bronchi can be achieved. Therefore, this approach should be preserved for bifurcational lesions with limited extent. If the tumor extends more distally than expected and resection of the lung parenchyma seems inevitable, the incision has to be enlarged to a hemi-clamshell to the respective side. After complete median sternotomy, the pericardium must be opened between the SVC and ascending aorta. The SVC is surrounded by a loop and pulled to the left. The retropericardial portion of the right pulmonary artery is freed from the pericardium ventrally and pulled caudally. By pulling the ascending aorta to the right, the tracheal bifurcation can be seen. After transection of the pretracheal fascia, the infracarinal lymph nodes are visible. After dissection of this compartment, avoiding radical devascularization, the trachea and mainstem bronchi are exposed and the level of transection defined. The proximity of the laryngeal recurrent nerve must be kept in mind. The ventilation tube has to be placed far above the bifurcational area with its distal tip. After starting the jet ventilation, the bifurcation can be resected. The main bronchi are grasped with forceps or traction sutures to prevent retraction. (b, c) Reconstruction starts with a side-to-side suture of the main bronchi, with ties placed on the outside. The end-to-end anastomosis with a running suture begins at the posterior wall; however, the adaption is withheld until traction sutures are in place and under tension. The adaption may be supported by additional traction sutures placed more proximally and more distally to the anastomotic level. Flexion of the head can further support adaptation. Once the single sutures of the anterior wall are tied, ventilation is switched over to the tracheal tube. Leakage should be excluded by applying ventilation pressure of up to 35 cm H2O. Pericardial fat flaps are suitable for coverage, as an alternative omentum majus may be used, which is more versatile and can be retrieved using a short extension of the skin incision
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


