Self-care theory
Nursing Care Management
Management of care involves clinical processes linked to people’s healthcare. Management of clinical processes can be seen as the most appropriate for adjusting the criterion of the health team according to the most dominant sanitary criterion in management teams, having links between clinical logic, which has the individual patient as its thrust, and sanitary logic, which considers collective users/patients.
In order to generate an effective management of care, we have to consider available evidence through different updated publications, patient’s preferences in relation to what are his/her educational needs, and the environment and available resources.
The new model of global hospital management is based on the integral model of health attention, which is defined as the group of actions that enforce and facilitate efficient, effective, and opportune attention directed not to specific incidents but toward persons considered in their physical and mental completeness, and as social beings belonging to different types of families and communities that are in a permanent process of integration and adaptation to their physical, social, and cultural environment.
Characteristics of a Correct Educational Instance for Self-Care
In the outpatient field, and particularly in a pulmonary function laboratory, the diversity of patients gives a rich educational instance for delivering tools for health self-care. “The self-care agency is the group of powers and abilities within the patient which allows him/her to commit to self-care”. This complex ability maintains or enforces the integrity of human structure, its functioning, and promotion of well-being, and it is acquired to satisfy continuous care requirements which regulate different processes.
For all diseases, adherence to treatment is the most important factor, but as it is susceptible of being modified, it compromises the results of treatments.
- 1.
Needs derived from diagnosis and treatment of the disease: adherence to treatments and control of the disease, family, and school environment.
- 2.
Needs derived from emotional and social disorders, for the adapting of parents and children: psychological support to the child and family.
- 3.
Needs related to school curriculum and early attention for favoring an appropriate cognitive, motor, affective, and social development of the child: early attention services, school units of support in hospital institutions, educational domiciliary attention, and school centers of reference.
- (a)
Adaptation of hospital, family, and school environment to the needs derived from the disease, for eliminating associated risk factors.
- (b)
Education of parents about how to control the disease and obtaining adherence to treatments. It represents a priority objective in this stage of the development of the child.
- (c)
Child’s control of the disease: management of devices, preparation for diagnostic tests and treatments. This objective is accomplished by incorporating the child to the educational instances.
Since 2009, there has been a program in our institution named “Education for health self-care”, where according to the patient’s pathology, certain topics are addressed for improving his/her health and to clarify question of his/her parents about basic care or general measures for maintaining good control of the disease.
Objectives of Educational Programs
Emphasizing the concept of disease;
Encouraging prevention according to the disease;
Directing the educational program to target group (depends on age group).
Educational programs have shown that they modify life quality and adherence to treatment.
Characteristics of an Efficient Education
Education must be understood as a continuous and dynamic process, adapted to the patient’s needs, for obtaining changes in attitudes and lifestyles of the patient and the family, which will surely produce an improvement in their life quality, allowing self-control and autonomous decision making.
Education is very important for the child that has a chronic disease.
Education must involve the patient, his/her family, and school environment.
Education must start when the diagnosis is made.
Education is continuous, and it is complemented until accomplishing self-management.
The main objective of education for self-care is to increase quality of life with no limitations.
For establishing a good, effective educational plan it is required to previously identify the real educational needs and the core of the disease presented in the child and his/her family.
Learning Areas
Affective: The main caregiver will recognize the importance of his/her participation in caring activities.
Cognitive: The caregiver can describe the signs of the chronic disease that affects the patient.
Psychomotor: The caregiver is capable of showing through supervised repetition each technique taught in the educational instance.
Evaluation of Educational Instances
They consider learning outcomes, whether the evolution of the disease is beneficial or not, and the way in which the patient, family, tutor, or main caregiver manages his/her everyday life. It is required to determine to what degree each agreed objective has been accomplished, the quality and effectiveness of applied techniques, and the quality of teachers in charge of transmitting the educational plan, and that is why the continuous training of the whole health team is so important. In order to clearly satisfy defined objectives, readjustments in the educational sequence have to be made, considering the learning capacity of the patient, family, or tutor, and their personal peculiarities.
Minimum Contents of an Effective Educational Instance
In a center of reference of respiratory diseases, the health professional is in contact with several diseases, as well as the patients and their families. Asthma, cystic fibrosis, sleep disorders, and food allergies are reviewed in this chapter.
Self-Care in Asthma
It must be highlighted that education is not just informing. Information is necessary, but insufficient. The objective is that the child and his/her family acquire abilities for controlling asthma.
Education must be stepwise, from basic knowledge, to self-control, if possible. In addition, it must be continuous, progressive, and adapted.
Authors themselves say that the use of educational programs generates a decrease in unscheduled medical visits, emergency visits, and hospitalizations, as well as school absenteeism.
Basic Knowledge about Asthma
What is asthma?
What factors influence in the emergence of asthma?
Rules for avoiding triggering allergens
Treatment Description
Patients and their relatives must know what rescue medications are and how to use them, along with knowing about preventive control medications. Frequent questions presented by parents are about adverse effects of the treatment, tachycardia associated with bronchodilators, and low height gain associated with steroids.
Prescription and Sequence of Utilization
Asthma treatment pursues two objectives: to obtain and maintain control of clinical signs and symptoms, preventing exacerbations, chronic obstruction of air flow, and decreasing mortality.
Pharmacological treatment of asthma is based on controlling inflammation, which is treated by anti-inflammatory drugs (basically, steroids, and in some cases, chromones or leukotriene antagonists), whereas bronchodilator drugs are applied as symptomatic drugs, also named rescue medications.
- 1.
Choosing the most appropriate device before prescription, which can be detected by the nursing personnel in the first encounter with the patient for educational instance.
- 2.
As we have seen, verifying the technique in every instance and showing in a physical way the technique and asking to repeat, to know whether both patient and tutor understood the technique.
Techniques for Medication Use
This is put into practice during the time exams are being made, which is the best instance for educating, because the patient stays at least 15–60 minutes with the nurse or nurse technician. In the medical visit, some contents can be reinforced.
Patients must correctly use the inhalation technique, which will be different according to the inhalation system used. An incorrect inhalation technique is equal to not taking the medication. In addition, a high and increasing number of commercial products for inhalation therapy exist: metered dose inhalers (MDI), holding chambers, dry powder inhaler (DPI), unit doses, multi-doses, auto-trigger systems, among others.
In toddlers, medium doses of MDI and small volume chambers with a mask are favored, whereas in school children (because of capacity), DPI or medium dose of MDI and chambers with a mouth piece are favored. We discourage mouth direct administration of MDI. Assessment of the technique must be a part of every encounter in children with asthma. Families must know how to keep chambers clean, verify the device’s correct functioning, know when few doses of the drug are left if it does not have a dose counter, and buccal hygiene rules after its administration.
Educational Factors
Recognizing and avoiding triggering factors
Ability to monitor symptoms
Correctly mastering drug inhalation techniques.
Ability to recognize when asthma is worsening
Knowing how to act pre-emptively before any variation of the process is essential.
Self-care abilities will be applied by families in cases of breastfed babies and infants, and progressively, according to growth, the child will be involved in the control of his/her disease. There has to be room for the child to express feelings about his/her disease and his/her opinion about the treatment, letting him/her choose, as far as possible, his/her inhalation device, as long as the child has a good command of the technique. In many occasions, especially in adolescents, talking to the patient alone is useful, without the presence of the parents. Starting with the information and correct application of the abilities acquired, self-control will be the ability to understand clinical situations and make the right decisions for them.
In order to act in case of deterioration, there has to be a previously made self-treatment plan. On the basis of a control of symptoms or measurement of peak expiratory flow (PEF), there must be a written maintenance treatment: when to use rescue medication, when to increase the dose of anti-inflammatory inhalation medication, when to start a pattern of oral steroids, and when, how, and whom to ask for medical help.
In pediatrics, the strategy for recognizing signs and symptoms of progressive obstruction of the airway and developing a plan depends on factors, such as age, sociocultural level of the family, and also involving the older child or adolescent in the process, the severity of the asthma or whether it is persistent or seasonal.
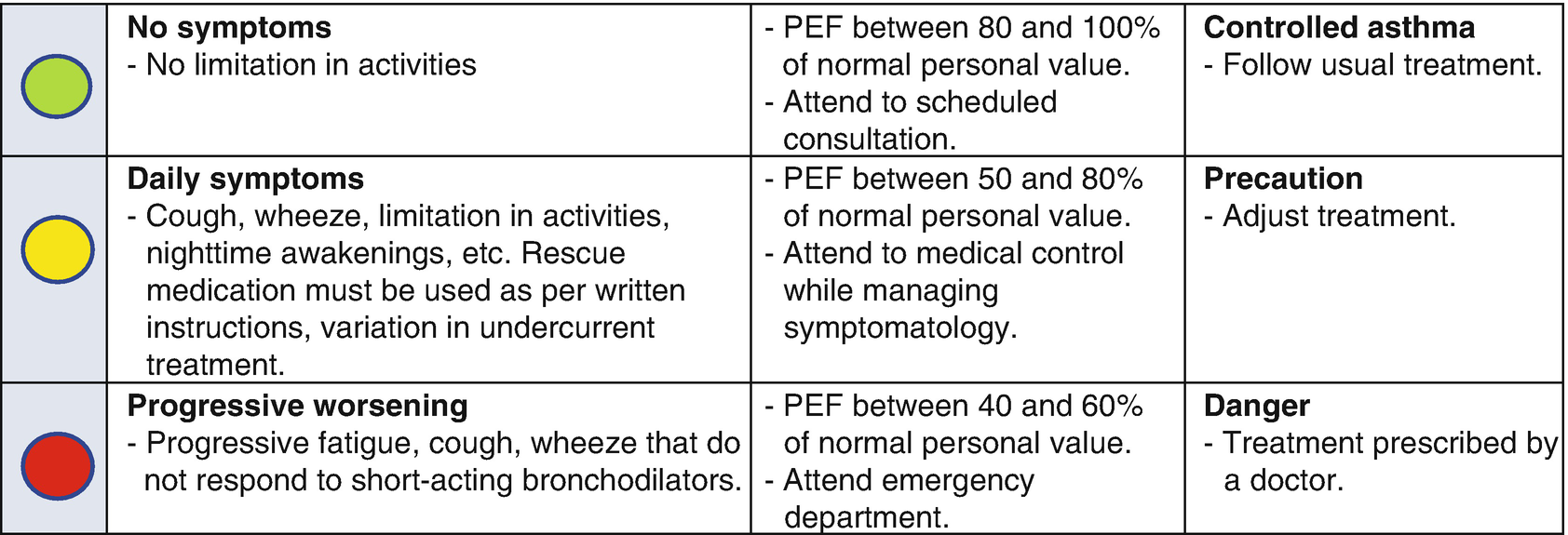
Self-control measures (warning system)
The importance of peak expiratory flow in self-control of asthma lies in the possibility of home use, because the PEF measuring device is small in size and easily transportable, its use is basic, and provides objective and quantifiable values.
Self-Care in Cystic Fibrosis
Cystic fibrosis (CF) is the most frequent autosomal recessive disease in the white race. Commonly, this results in development of chronic obstructive pulmonary disease and secondary malnutrition. Since pulmonary damage flourishes progressively, early diagnosis and focusing on respiratory and nutritional management are crucial for improving the prognosis of these patients.
Medical advances achieved during the last 30 years have increased survival rate, which is now up to 40 years of life. As it is a multisystem and progressive disease, whose treatment includes different daily measures affecting nutrition and the respiratory system, patients and caregivers have a great responsibility in controlling the disease and applying treatment measures, aiming for a better general health condition as well as slowing the progression of the disease. Educational intervention helps patients and families to solve problems, set goals, and plan some changes in their lifestyles in order to better manage the disease.
The role performed by the patient and family members in the active management of their attentions is now considered relevant for increasing the probability of positive health results. Educational programs in cystic fibrosis traditionally provided specific knowledge with the only purpose to fulfill the pharmacological treatment. Currently, educational programs are oriented toward placing patients and their relatives as experts that work collaboratively with sanitary professionals in the treatment of the disease.
Education of the patient and her/his relatives;
Aforementioned respiratory physiotherapy and muscular training;
Psychosocial and nutritional control;
Oxygen therapy teaching and control;
Non-invasive ventilation teaching and control, in required cases;
Home assistance.
Throughout the years, parents become specialists in the disease, and the level of response they expect requires a trained health team. Specialist nursing personnel is actively involved in the decision making related to the treatment and monitoring of medical attention in these patients that are with the health team for years.
Nursing personnel must coordinate the attention between patient and family, besides extra-hospital services, both at a practical level and through support and advice. This is accomplished through their function as a teacher, reliable caregiver, advisor, and confidant. Trusting this professional must have a benefit in the good management of acute and chronic symptoms.
Patients have the responsibility of taking the correct doses of the prescribed medications in a timely manner and in the right order. Normally, patients with cystic fibrosis have very complex pharmacological regimes. The clinical pharmaceutical professional can help in educating patients about correct drug reconstitution, inhalation, and the correct order of the drugs.
Education of the patient with cystic fibrosis is considered fundamental, since he/she has to be aware of the disease in all its aspects, because patients that know their problem (progression, treatment to follow, etc.) get much more involved in therapeutic guides, both of medicines and its rehabilitation, and they are more motivated to fight for its healing or relief.
Nurse Specialized in Cystic Fibrosis
He/she has responsibilities with patients, relatives, and personnel involved in medical attention of patients, so he/she has to commit to care for them.
Advocating for each patient and having updated information about current treatment practices.
Maintaining and teaching clinical experience and practice.
Support and advice.
Education and investigation.
Relationship with patients and relatives.
As a chronic disease, with differences in its development, educational stages overlap when working with the patient.
Decreasing respiratory symptoms and flare-ups;
Improving state of mind (increasing motivation);
Increasing tolerance to efforts (by improving muscular function);
Decreasing number of hospital admissions;
Reducing days of hospitalization;
Prolonging survival.
Hereunder, we deliver some topics as an example to educate family and patient:
Basic Knowledge About the Disease
Cystic fibrosis is an inherited and incurable disease, which mainly affects the digestive tube, lungs, and pancreas. It is one of the most common chronic pulmonary diseases in boys, girls, and young adults. Cystic fibrosis is caused by an abnormal gene that produces a thick and sticky liquid called mucus, which accumulates in airways and pancreas. This causes pulmonary infections that can be complex, as well as digestive problems, and may affect the male reproductive system.
Cystic Fibrosis Signs and Symptoms
Symptoms do not appear simultaneously, but many times they do it gradually. That is why it is important to mention them in each educational instance to make the patient, family, or main caregiver alert for symptoms that can appear in the course of this chronic disease.
Upper airway manifestations: Symptoms and signs of the upper airway according to age.
Lower airway manifestations: Symptoms and signs of lower airway according to age.
Respiratory exacerbations: Most patients have an insidious respiratory worsening, that is characterized by exacerbations of its chronic pulmonary infection. It is taught to parents or tutors to recognize these changes and to have a meticulous registration of pulmonary images, cultures, and lung function tests.
Microbiology: Patients are colonized according to the disease’s progression and the accompanying flora varies over the course of the disease, for this purpose, active vigilance during exacerbations is important. In this process, patients and relatives have a leading participation.
Pulmonary complications: They are taught to recognize the presence of atelectasis, bronchiectasis, hemoptysis, and pneumothorax according to the disease’s progression.
Pancreatic, hepatic, and urogenital complications: They are taught about signs and appearance of complications according to the disease’s advance, in order to detect them in a timely manner.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


