Few reports have examined the utility of plasma B-type natriuretic peptide (BNP) testing for cardiovascular (CV) risk stratification in real-world hypertensive subjects. Subjects of the study were community-based hypertensive patients (n = 5,865). The CV event rate within each BNP quartile was estimated, and a Cox regression model was used to determine the relative hazard ratio (HR) among the quartiles. Furthermore, to determine the usefulness of BNP as a biomarker in combination with the Framingham risk score (FRS), the predictive abilities in terms of area under the curve of receiver operating characteristic analysis, net reclassification improvement, and integrated discrimination improvement indices were determined. The mean follow-up duration was 5.6 years. The highest quartile showed a significantly higher rate of CV events compared with the lower quartiles (p <0.001). After adjustment for established CV risk factors, the HR for CV events increased significantly according to the quartile (p value for trend <0.03), and the HR for the highest quartile was significantly elevated compared with the lowest quartile (HR 1.59, 95% confidence interval 1.16 to 2.19). The predictive abilities of BNP in terms of sensitivity and specificity for CV events were comparable with those of FRS. When BNP was added to an FRS-only model, the predictive abilities in terms of area under receiver operating characteristic curve, net reclassification improvement, and integrated discrimination improvement were significantly increased (all; p <0.001). Elevated BNP levels are thus a useful biomarker for CV risk stratification in unselected real-world hypertensive subjects. Adding BNP to an established CV risk score improves the predictive ability in this cohort.
B-type natriuretic peptide (BNP) is a hormone that is released from the heart along with its biologically inactive N-terminal peptide (N-terminal probrain natriuretic peptide [NT-proBNP]). It has been suggested that cardiac secretion of BNP is increased by elevated left ventricular end-diastolic pressure, decreased cardiac systolic and/or diastolic function, atrial fibrillation, myocardial ischemia, and hypertensive heart disease. Although circulating levels of BNP have been reported to be a predictive biomarker of cardiovascular (CV) events in several types of CV diseases in the general population, it remains unknown whether BNP is valid for prediction of CV events in subjects with hypertension, and whether its use in conjunction with an established clinical predictive score would improve its predictive abilities. The purpose of this study is to clarify whether plasma BNP testing is a valid means, both singly and in combination with an established CV risk score, for assessing the risk of CV events in subjects with hypertension within the general population.
Methods
The subjects of the present study were participants in the Iwate KENCO (KENpoku COhort) study cohort, which was designed to prospectively determine the risk of CV disease in the general Japanese adult population as described previously. The original cohort of the study was recruited during 2002 to 2004 from the community-based population in 3 districts (Ninohe, Kuji, and Miyako) of the northern Iwate prefecture, Japan. This region has a resident population of >144,000 adults aged >40 years. The cohort was recruited from subjects of a government-regulated multiphasic health checkup for the general population. The total number of subjects who agreed to participate within the study district was 26,469. Of this original cohort in the Ninohe and Kuji districts (n = 15,927), 97% of subjects agreed to undergo plasma BNP measurement (men 5,288; women 10,106).
The study design incorporated a baseline survey, which consisted of a self-administered lifestyle questionnaire, blood pressure (BP) measurement, electrocardiography, anthropometrical measurement, and blood collection. Systolic and diastolic BPs were determined with an automated sphygmomanometer (BP103i II; Nippon Colin, Komaki, Japan) placed on the right arm of seated subjects who had rested in a sitting position for at least 5 minutes before measurement. Measurement was performed twice, with the mean value used for statistical analysis. Hypertension was defined by ≥1 of the following factors: systolic BP ≥140 mm Hg, diastolic BP ≥90 mm Hg, and the use of antihypertensive agents. Left ventricular hypertrophy (LVH) was defined by electrocardiographic criteria (Sokolow-Lyon voltage criteria; SV 1 + RV 5 or RV 6 >35mV), and the number of subjects with hypertensive LVH was 1,771 (men 822, women 949; mean age 66 ± 9 years). Subjects with the following characteristics were excluded: history of CV events such as stroke, heart failure, or acute myocardial infarction and age <40 years. A final hypertensive cohort of 5,865 subjects was analyzed in this study (2,145 men and 3,720 women, mean age 66 ± 9 years). The study protocol was approved by the Iwate Medical University Institutional Ethical Committee (H13-33). All participants gave written informed consent.
The end point of the study was a composite outcome comprising stroke, heart failure, acute myocardial infarction, and sudden unexpected death. Information about emigration was obtained from local government records (October 2009). Stroke was identified from local stroke registry data. Stroke was defined on the basis of symptoms (sudden onset of a focal neurological deficit of ≥24-hour duration) confirmed by brain computed tomography or magnetic resonance imaging. Heart failure was defined according to the Framingham criteria that were confirmed by the researchers from medical records at all general hospitals located within the study area. Incidence of myocardial infarction was also based on hospital registration survey data. The diagnosis of acute myocardial infarction was based on the MONICA (MONItoring of trends and determinants in CArdiovascular Disease) criteria. Based on death certificates, sudden unexpected death within 24 hours after the onset of acute illness was determined by a committee consisting of cardiologists, neurologists, and epidemiologists.
Blood samples were drawn from the antecubital vein while participants were seated. A 2-ml sample of venous blood was collected into a test tube containing EDTA-2Na. The tubes were stored, immediately after sampling, in an icebox and transported to the Iwate Health Service Association laboratory. They were centrifuged at 1,500g for 10 minutes, and plasma samples were stored frozen at −20°C until transportation to the Shionogi central laboratory for assay. Plasma BNP levels were measured by direct radioimmunoassay using monoclonal antibodies specific for human BNP (Shionoria RIA BNP kit; Shionogi & Co. Ltd., Osaka, Japan). Cross reactivity of the antibody was 100% for human BNP and 0.001% for human atrial natriuretic peptide. Intra- and interassay coefficients of variation were 5% and 6%, respectively.
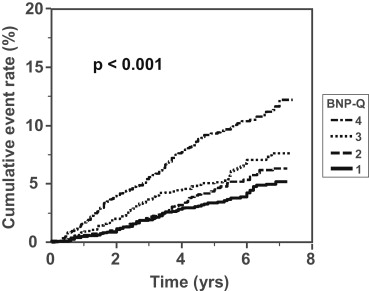
Participants were divided into quartiles according to baseline plasma BNP levels. Continuous variables are expressed as mean ± SD. Categorical parameters are expressed as proportions (percentage) and group comparisons were based on 1-way analysis of variance or chi-square test. The cumulative CV event rate within each BNP quartile was estimated using the Kaplan-Meier method. A multivariate Cox regression analysis was performed to examine the relative risk of onset of CV events among the BNP quartiles. For all models, the hazard ratios (HRs) were adjusted for age, sex, body mass index, systolic BP, estimated glomerular filtration rate, the use of antihypertensive drugs, diabetes, hyperlipidemia, current smoking, and atrial fibrillation (model 1), and further adjustments included electrocardiographically proven LVH (model 2). For the analyses of CV incidence, person-years were determined at the date of the CV events, date of emigration from the study area, date of death, or end of the follow-up period, whichever came first. The follow-up survey was carried out after the baseline study through to March 2009.
To compare BNP testing and Framingham risk score (FRS) in terms of their overall diagnostic accuracy for general CV events, receiver operating characteristic curves were constructed, and the area under the curve (AUC) and 95% confidence intervals (CIs) for each receiver operating characteristic curve were calculated. In addition, to determine the usefulness of plasma BNP as a predictor of CV events in addition to FRS, we calculated net reclassification improvement and integrated discrimination improvement indices. These statistical analyses were performed using SPSS software (version 11.0.1 J, Chicago, Illinois) or R software (CRAN project, version 3.0.1, http://cran.r-project.org/ ). A significant difference was defined as p <0.05.
Results
Table 1 presents a comparison of clinical variables according to quartile levels of plasma BNP. Age, percentage of women, systolic BP, the use of antihypertensive drugs, prevalence of LVH, and atrial fibrillation increased with increasing levels of BNP. Estimated glomerular filtration rate decreased with increasing levels of BNP.
| Variable | Total (n = 5,865) | Q1 (n = 1,469) | Q2 (n = 1,471) | Q3 (n = 1,456) | Q4 (n = 1,469) | p Value |
|---|---|---|---|---|---|---|
| Interquartile level of BNP (pg/ml) | 10.2–38.2 | 2.5–5.4 | 12.7–15.1 | 23.8–27.2 | 45.5–56.9 | |
| Age (yrs) | 66 ± 8.8 | 61.9 ± 9.0 | 65.2 ± 8.0 | 67.5 ± 8.0 | 70.7 ± 7.2 | <0.0001 |
| Men/Women | 2,145/3,720 | 641/828 | 517/954 | 458/998 | 529/940 | 0.018 |
| Systolic BP (mm Hg) | 142.9 ± 17.9 | 142.8 ± 17.1 | 140 ± 17.5 | 142.6 ± 17.3 | 144.1 ± 19.3 | 0.015 |
| Diastolic BP (mm Hg) | 82.2 ± 10.5 | 86.8 ± 11.4 | 84.2 ± 10.4 | 82.6 ± 9.9 | 80.8 ± 11.5 | <0.0001 |
| Antihypertensive drugs | 58% | 50% | 58% | 60% | 65% | <0.0001 |
| Body mass index (kg/m 2 ) | 24.9 ± 3.4 | 25.1 ± 3.4 | 25.1 ± 3.3 | 24.8 ± 3.3 | 24.6 ± 3.5 | <0.0001 |
| Obesity | 47% | 49% | 50% | 45% | 44% | 0.003 |
| Diabetes | 10% | 11% | 9% | 9% | 9% | 0.075 |
| Hypercholesterolemia | 18% | 22% | 18% | 17% | 14% | <0.0001 |
| Current smoking | 12% | 17% | 11% | 10% | 10% | <0.0001 |
| LVH | 32% | 26% | 30% | 31% | 41% | <0.0001 |
| Atrial fibrillation | 1.7% | 0.2% | 0.1% | 0.3% | 6.4% | <0.0001 |
| eGFR (ml/min/1.73 m 2 ) | 73.7 ± 15.3 | 77.6 ± 15.7 | 74.8 ± 14.9 | 73.1 ± 14.6 | 69.1 ± 14.6 | <0.0001 |
During a mean follow-up period of 5.6 years, 382 participants experienced CV events including heart failure (n = 52), myocardial infarction and sudden unexpected death (n = 72), and stroke (n = 258). The cumulative incidence of CV events was assessed using the Kaplan-Meier method. A quartile-dependent increase in the risk of CV events was seen in BNP testing, with the highest quartile showing a significantly greater incidence than the other 3 (p <0.001; Figure 1 ). A multivariate Cox regression analysis was performed to analyze the relation between the BNP quartiles and the risk of CV events. After adjustment for classical CV risk factors (model 1), the highest BNP quartile showed a significantly elevated HR for CV events compared with the lowest quartile (HR 1.59, 95% CI 1.16 to 2.19; Figure 2 ). In the LVH adjusted model (model 2), the relation between BNP quartile and CV event rate remained significant (HR 1.49, 95% CI 1.07 to 2.10; Figure 2 ).