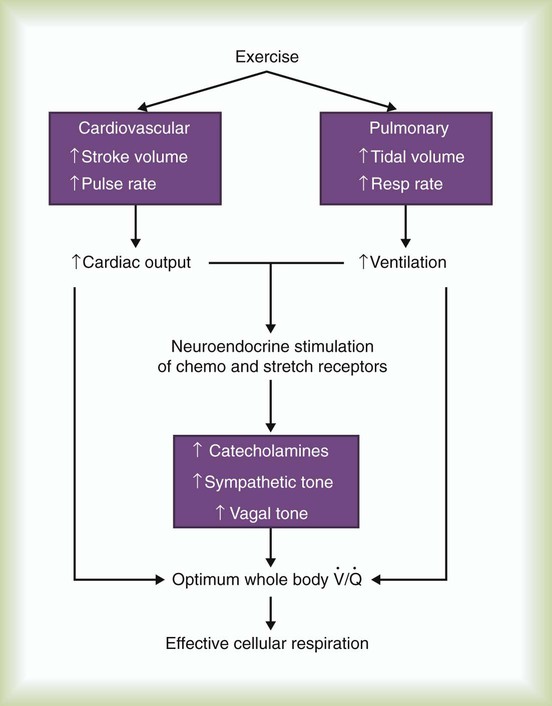
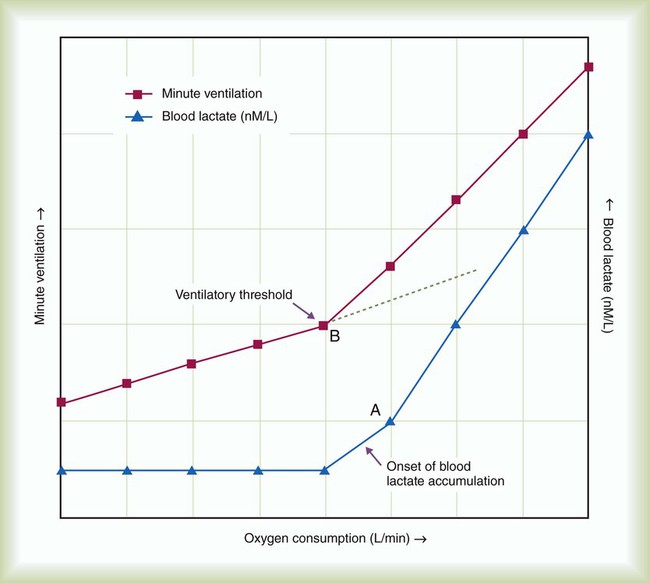
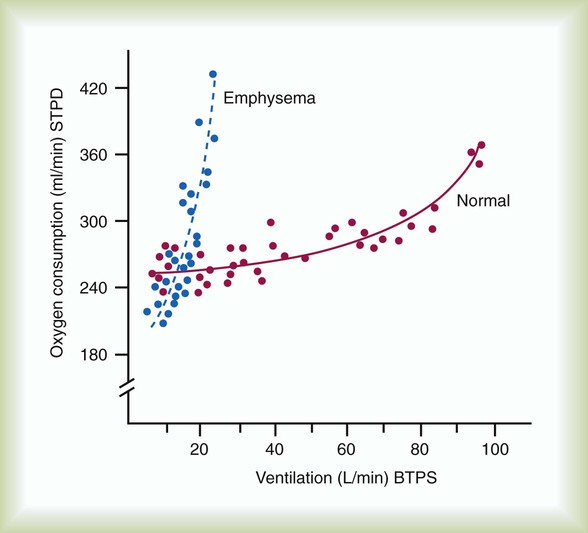
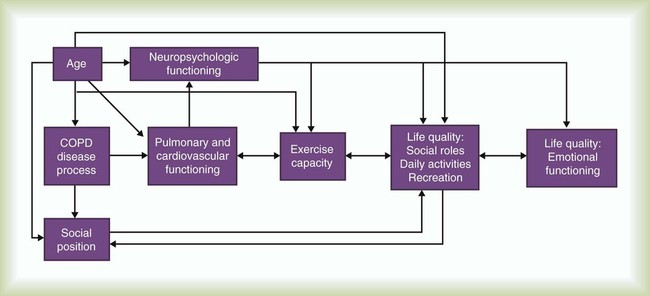
After reading this chapter you will be able to: Steady improvements in acute care are presenting new medical and social problems. As more patients survive acute illnesses, there are increasing numbers of individuals with chronic disorders. These chronic disorders are associated with a wide spectrum of physiologic, psychologic, and social disabilities. Foremost among these individuals with chronic disorders are individuals with chronic cardiopulmonary disease. Chronic obstructive pulmonary disease (COPD) is expected to be the third leading cause of death in the United States by 2020.1 The Council on Rehabilitation defines rehabilitation as “the restoration of the individual to the fullest medical, mental, emotional, social, and vocational potential of which he or she is capable.”2 The overall goal is to maximize functional ability and to minimize the impact the disability has on the individual, the family, and the community. Pulmonary rehabilitation is the “art of medical practice wherein an individually tailored, multidisciplinary program is formulated, which through accurate diagnosis, therapy, emotional support, and education stabilizes or reverses both the physio- and psychopathology of pulmonary diseases and attempts to return the patient to the highest possible functional capacity allowed by his or her pulmonary handicap and overall life situation.”3 The general goals of pulmonary rehabilitation are to control and alleviate symptoms, restore functional capabilities as much as possible, and improve quality of life.4 Pulmonary rehabilitation does not reverse or stop progression of the disease, but it can improve a patient’s overall quality of life. Health care providers from various disciplines are needed to reach these goals. Pulmonary rehabilitation is not a new concept. In 1952, Barach and colleagues5 recommended reconditioning programs for patients with chronic lung disease to help improve their ability to walk without dyspnea. Decades passed before clinicians paid any attention to this concept. Instead of having their patients participate in reconditioning programs, most physicians simply prescribed oxygen (O2) therapy and bed rest. The result was a vicious cycle of skeletal muscle deterioration, progressive weakness and fatigue, and increasing levels of dyspnea including at rest. Patients became homebound, then room-bound, and eventually bed-bound. Improved avenues of therapy and rehabilitation were needed. In 1962, Pierce and associates6 published results confirming Barach’s insight into the value of reconditioning. They observed that patients with COPD who participated in physical reconditioning exhibited lower pulse rates, respiratory rates, minute volumes, and carbon dioxide (CO2) production during exercise. However, they also found that these benefits occurred without significant changes in pulmonary function. Soon thereafter, Paez and associates7 showed that reconditioning could improve both the efficiency of motion and O2 use in patients with COPD. Subsequently, Christie8 showed that the benefits of reconditioning could be achieved on an outpatient basis with minimal supervision. Since Christie’s work in 1968, other investigators have continued to research the benefits of pulmonary rehabilitation. The available evidence at the present time consistently indicates that pulmonary rehabilitation benefits patients with chronic obstructive and restrictive pulmonary disease.9–12 When combined with smoking cessation, optimization of blood gases, and proper medication use, pulmonary rehabilitation offers the best treatment option for patients with symptomatic pulmonary disease. Programs for pulmonary rehabilitation must be founded on the sound application of current knowledge in the clinical and social sciences. In fall 2006, the American College of Chest Physicians (ACCP) and the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) released their evidence-based guidelines relating to pulmonary rehabilitation aimed at improving the way pulmonary rehabilitation programs are designed, implemented, and evaluated through patient outcomes.13 At rest, an individual maintains homeostasis by balancing external, internal, and cellular respiration. Physical activity, such as exercise, increases energy demands. To maintain homeostasis during exercise, the cardiorespiratory system must keep pace. Figure 50-1 shows how the body responds to exercise. Ventilation and circulation increase to supply tissues and cells with additional O2 and to eliminate the higher levels of CO2 produced by metabolism. As depicted in Figure 50-2, O2 consumption and CO2 production also increase in linear fashion as exercise intensity increases. If the body cannot deliver sufficient O2 to meet the demands of energy metabolism, blood lactate levels increase above normal. In exercise physiology, this point is called the onset of blood lactate accumulation (OBLA). As this excess lactic acid is buffered, CO2 levels increase, and the stimulus to breathe increases. The result is an abrupt upswing in both CO2 and Patients with COPD who lack adequate pulmonary function have severe limitations to their exercise capabilities. Their high rate of CO2 production during exercise results in respiratory acidosis and a shortness of breath out of proportion to the level of activity. In addition, as ventilation increases, the rate of O2 consumption in a patient with COPD increases significantly (Figure 50-3). Together, these factors limit patient tolerance for any significant increase in physical activity. Pulmonary rehabilitation must include efforts to recondition patients physically and increase their exercise tolerance. Reconditioning involves strengthening essential muscle groups, improving overall O2 use, and enhancing the body’s cardiovascular response to physical activity (Box 50-1). If the overall goal of pulmonary rehabilitation is to improve the quality of patients’ lives, physical reconditioning alone is insufficient. Psychosocial indicators generally are good predictors of morbidity in patients with COPD. Studies show that the relative success of reconditioning plays less of a role in determining whether patients complete a program than meeting their psychosocial support needs.14 Figure 50-4 presents elements of how chronic lung disease and other variables can have an impact on a patient’s quality of life. It is here that the link between the physical reconditioning and psychosocial support components of rehabilitation becomes most evident. By reducing exercise intolerance and enhancing the body’s cardiovascular response to physical activity, patients can develop a more independent and active lifestyle. For some patients, simply being able to walk to the market or play with their grandchildren can contribute to a greater feeling of social importance and self-worth. For others, physical conditioning may allow a return to near-normal levels of activity, including vocational pursuits. Pulmonary rehabilitation programs vary in their design and implementation but generally share common goals. Examples of these common goals are listed in Box 50-2. These general goals assist planners in formulating more specific program objectives. When determining objectives, both patients and members of the rehabilitation team should have input. These objectives should always be stated in measurable terms because this helps facilitate the determination of both patient outcomes and the therapeutic success and value of pulmonary rehabilitation. Depending on the specific needs of the participants, program objectives can include the following: • Development of diaphragmatic breathing skills • Development of stress management and relaxation techniques • Involvement in a daily physical exercise regimen to condition both skeletal and respiratory-related muscles • Adherence to proper hygiene, diet, and nutrition • Smoking cessation (if applicable) • Proper use of medications, O2, and breathing equipment (if applicable) • Application of airway clearance techniques (when indicated) Pulmonary rehabilitation programs must have a qualified medical director, usually a pulmonologist, to provide overall medical direction of the program and to screen prospective patients.17 Patient evaluation begins with a complete patient history—medical, psychologic, vocational, and social. A well-designed patient questionnaire and interview form assist with this step. The patient history should be followed by a complete physical examination (see Chapter 15). A recent chest film, resting electrocardiogram (ECG), complete blood count, serum electrolytes, and urinalysis provide additional information on the patient’s current medical status (see Chapter 16). To determine the patient’s cardiopulmonary status and exercise capacity, both pulmonary function testing and a cardiopulmonary exercise evaluation may be performed. Pulmonary function testing includes assessment of pulmonary ventilation, lung volume determinations, diffusing capacity (DLCO), and spirometry before and after bronchodilator use (see Chapter 19). The cardiopulmonary exercise evaluation serves two key purposes in pulmonary rehabilitation. First, it quantifies the patient’s initial exercise capacity. This quantification provides the basis for the exercise prescription (including setting a target heart rate) and yields the baseline data for assessing a patient’s progress over time. In addition, the evaluation helps determine the degree of hypoxemia or desaturation that can occur with exercise; this provides the objective basis for titrating O2 therapy during the exercise program. To guide practitioners in implementing exercise evaluation, the American Association for Respiratory Care (AARC) has published clinical practice guidelines on exercise testing for evaluation of hypoxemia or desaturation or both18 and pulmonary rehabilitation. Excerpts from these guidelines appear in Clinical Practice Guidelines 50-1 and 50-2.19 Modified Borg Dyspnea Scale (With Dyspnea Descriptors) The exercise evaluation procedure involves serial or continuous measurements of several physiologic parameters during various graded levels of exercise on either an ergometer or a treadmill (Box 50-3). To allow for steady-state equilibration, these graded levels are usually spaced at 3-minute intervals. Work levels are increased progressively until either (1) the patient cannot tolerate a higher level or (2) an abnormal or hazardous response occurs.
Cardiopulmonary Rehabilitation
 State the definition and general goals of pulmonary rehabilitation programs.
State the definition and general goals of pulmonary rehabilitation programs.
 Explain the rationale for exercise conditioning and psychosocial support of patients with chronic pulmonary disease.
Explain the rationale for exercise conditioning and psychosocial support of patients with chronic pulmonary disease.
 Describe how to evaluate and select patients for pulmonary rehabilitation.
Describe how to evaluate and select patients for pulmonary rehabilitation.
 Describe pulmonary rehabilitation program design including format and content.
Describe pulmonary rehabilitation program design including format and content.
 List the educational content to be addressed in a pulmonary rehabilitation program.
List the educational content to be addressed in a pulmonary rehabilitation program.
 Describe the implementation of a pulmonary rehabilitation program, including staffing, facilities, scheduling, class size, equipment, costs, and reimbursement.
Describe the implementation of a pulmonary rehabilitation program, including staffing, facilities, scheduling, class size, equipment, costs, and reimbursement.
 Discuss the outcome measures that can be used to evaluate pulmonary rehabilitation programs.
Discuss the outcome measures that can be used to evaluate pulmonary rehabilitation programs.
 Identify the potential hazards associated with pulmonary rehabilitation.
Identify the potential hazards associated with pulmonary rehabilitation.
Definitions and Goals
Historical Perspective
Scientific Basis
Physical Reconditioning
 (referred to as the ventilatory threshold). Beyond this point, metabolism becomes anaerobic, the efficiency of energy production decreases, lactic acid accumulates, and fatigue sets in.
(referred to as the ventilatory threshold). Beyond this point, metabolism becomes anaerobic, the efficiency of energy production decreases, lactic acid accumulates, and fatigue sets in.
Psychosocial Support
Structure of A Pulmonary Rehabilitation Program
Program Goals and Objectives
Patient Evaluation and Selection
Patient Evaluation
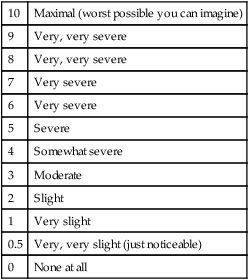
10
Maximal (worst possible you can imagine)
9
Very, very severe
8
Very, very severe
7
Very severe
6
Very severe
5
Severe
4
Somewhat severe
3
Moderate
2
Slight
1
Very slight
0.5
Very, very slight (just noticeable)
0
None at all

 and
and  during submaximal exercise. Point A represents OBLA. At the same time,
during submaximal exercise. Point A represents OBLA. At the same time,  and
and  “break” from their extrapolated rate of increase and abruptly rise (point B). This is referred to as the ventilatory threshold.
“break” from their extrapolated rate of increase and abruptly rise (point B). This is referred to as the ventilatory threshold. 

 )
) or METS)
or METS)

