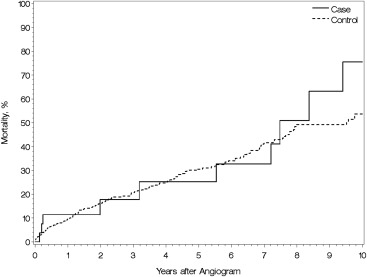
Although rare, numerous case reports suggest that Thebesian veins confer increased morbidity and mortality. No study has evaluated their effects on cardiac structure or long-term patient outcomes. Patients undergoing coronary angiogram at the study institution from October 2002 and January 2015 were assessed for a diagnosis of prominent Thebesian veins. A matched control group was created and comparisons between clinical, echocardiographic, and survival measures were made. Of 50,116 total patients, 31 (0.06%) were found to have prominent Thebesian veins on angiography and were compared with a matched control group of 596 patients. Patients were matched for age, gender, angiogram date, location and extent of coronary disease, and dominance. Demographic and clinical data were similar between cohorts, with a median follow-up period of 26 months. Patients with Thebesian veins had lower Doppler E wave (0.7 vs 0.8; p = 0.007) and A wave (0.6 vs 0.8; p = 0.001) mitral inflow velocities suggesting some decrease in normal mitral inflow, potentially due to direct shunting into the ventricle from the Thebesian vein network. However, there was no observed difference in left ventricular size or ejection fraction between groups. There was also no significantly increased mortality associated with the presence of Thebesian veins (hazard ratio 1.11, 95% CI 0.58 to 2.13). In conclusion, although previous reports have suggested adverse outcomes from Thebesian veins, our case–control study demonstrated no significant associated adverse cardiac structural changes or increase in mortality, although patients with Thebesian veins were noted to have a decrease in mitral inflow velocities.
Although small studies have identified the possibility of Thebesian veins to be the cause of pathologic changes to the heart, there is no study assessing long-term patient outcomes, and all studies to date have lacked a control group for comparison. In this study, we sought to clarify the hemodynamic effects of Thebesian veins on left ventricular structure, function, and impact on mortality by reporting the largest series to date using matched controls as a comparator group. Based on previous reports, we hypothesized that patients with prominent Thebesian veins would have evidence for left ventricular dysfunction and higher prevalence of heart failure compared with patients without prominent Thebesian veins.
Methods
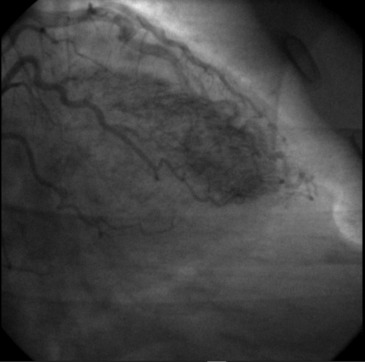
A retrospective analysis of all patients undergoing coronary artery angiography at the study institution (Mayo Clinic, Rochester, Minnesota) from October 2002 to January 2015 was performed to identify all patients with Thebesian veins prominent enough for the angiographer to include them as one of the clinical diagnoses ( Figure 2 ). All angiograms with the diagnosis of Thebesian veins were reviewed independently by 2 of the investigators (DS and YNVR), and any discordance was resolved by review of the third investigator (ACL). All angiograms were graded according to the following criteria developed by the study investigators: grade 1 was defined as visible Thebesian network that clears of contrast with each systole; grade 2 as a visible Thebesian network that remains until contrast clears coronary system completely with no or minimal opacification of the ventricle; grade 3 as a visible Thebesian network with incomplete opacification of ventricle; and grade 4 as a visible Thebesian network with complete opacification of ventricle. A matched cohort of patients without Thebesian veins who underwent coronary angiography over this same period was developed for comparison. The restrictions used to identify matched controls for each case were age within 5 years, gender, angiogram within 3 years, presence of coronary artery disease (≥50% stenosis) for each major coronary artery (left main, proximal left anterior descending, mid to distal left anterior descending, circumflex, and right coronary artery), and coronary artery dominance (if disease present in left main or proximal left anterior descending). Exclusion criteria included cardiac transplantation, age less than 18 years, presence of other coronary fistulae, or other significant intracardiac shunting, and refusal to allow the use of medical records for research. Institutional review board approval was obtained before study initiation.
All data were obtained through the electronic medical record and the cardiac catheterization internal database. Data collected included pertinent clinical data, the co-morbidity burden as per the Charlson Index, coronary artery distribution and extent of disease, baseline creatinine at time of angiogram, and echocardiographic parameters on a comprehensive transthoracic echocardiogram within 1 year of catheterization. All echocardiographic variables were obtained per the American Society of Echocardiography and Mayo Clinic Echocardiogram Laboratory guidelines.
Variable summaries are presented as mean (SD) for continuous variables and frequency (percentage) for discrete variables. Kaplan–Meier methods were used to estimate mortality over time. Summary statistics for controls are weighted such that each set of matched controls contributes equal weight, rather than each control. In this way, the summary statistics are not skewed toward cases with more matched controls. Comparisons of patient characteristics were made using conditional logistic regression. Survival comparisons were assessed using Cox proportional hazards model with a frailty term for each set of case and matched controls. Statistical analysis was performed using SAS (SAS Institute Inc., Cary, North Carolina) statistical software. All significance tests were 2 tailed with a 0.05 significance level.
Results
A total of 69,699 angiograms were performed during the study period on 52,488 unique patients. About 2,299 patients were excluded due to their records not being authorized for use in medical research. Of the 50,116 patients included, only 31 patients (0.06%) were coded for the presence of Thebesian veins. A total of 3 patients were defined as grade 2 Thebesian vein network, 11 as grade 3, and 17 as grade 4. No patients were defined as grade 1 and the median score was grade 4. Little interrater variability was present (kappa 0.83, 95% CI 0.65 to 1.01), and 3 angiograms were reviewed by a third investigators because of discordance in initial grading. About 596 patients were matched as controls.
The average age in both cohorts was 66 years (p = 0.66), and most patients were women (67.7%). Most patients were right dominant, and the majority had no significant coronary artery disease. A trend toward a greater proportion of patients with a diagnosis of congestive heart failure (n = 14, 45.2%) was seen in the Thebesian vein group compared with controls (n = 189, 31.7%; p = 0.11), but this was not statistically significant. The groups were well matched and Charlson Comorbidity Index was similar between both cohorts. Importantly, there was no difference in the baseline prevalence of heart failure (29% vs 28%, p = 0.88) or myocardial infarction (26% vs 20%, p = 0.35) between the matched groups.
Table 1 represents the echocardiographic comparisons between the case and control groups. Ejection fraction was similar between both groups. There was a lower Doppler mitral inflow E and A wave in the Thebesian vein group, suggesting a decrease in normal mitral inflow through the mitral valve, potentially due to direct shunting from the coronary artery to left ventricle. Despite this shunting, there was no difference in measured left ventricular systolic or diastolic dimensions in patients with prominent Thebesian veins. Shunting through the Thebesian veins was also not associated with an increase in valvular regurgitation. There was no difference between groups in right ventricular size, function, right atrial, or right ventricular systolic pressure.
| Variable | Thebesian Veins (n=29) | Control (n=481) | p-value |
|---|---|---|---|
| Ejection Fraction (%) | 57 +/- 15 | 56 +/- 14 | 0.79 |
| LVEDD (mm) | 49 +/- 7 | 49 +/- 7 | 0.70 |
| LVESD (mm) | 32 +/- 9 | 33 +/- 9 | 0.44 |
| Left Atrial Volume Index (mL/m 2 ) | 40 +/- 30 | 38 +/- 16 | 0.96 |
| Lateral E′ Velocity (m/s) | 0.08 +/- 0.04 | 0.08 +/- 0.04 | 0.85 |
| Septal E′ Velocity (m/s) | 0.06 +/- 0.03 | 0.07 +/- 0.03 | 0.92 |
| E Wave Velocity (m/s) | 0.66 +/- 0.2 | 0.84 +/- 0.29 | 0.007 |
| A Wave Velocity (m/s) | 0.58 +/- 0.22 | 0.84 +/- 0.59 | 0.001 |
| RV Function | 0.48 | ||
| Normal | 16 (67%) | 310 (76%) | |
| Mild | 5 (21%) | 57 (14%) | |
| Moderate | 2 (8%) | 32 (8%) | |
| Severe | 1 (4%) | 11 (3%) | |
| RV Size | 0.37 | ||
| Normal | 16 (67%) | 322 (73%) | |
| Mild | 4 (17%) | 67 (15%) | |
| Moderate | 2 (8%) | 36 (8%) | |
| Severe | 2 (8%) | 18 (4%) | |
| Estimated RA Pressure (mm Hg) | 9 +/- 6 | 8 +/- 4 | 0.21 |
| Estimated RVSP (mm Hg) | 34 +/- 17 | 38 +/- 13 | 0.37 |
| Mitral Regurgitation | 0.57 | ||
| None | 1 (5%) | 8 (2%) | |
| Mild | 15 (75%) | 315 (81%) | |
| Moderate | 4 (20%) | 42 (11%) | |
| Severe | 0 | 24 (6%) | |
| Aortic Regurgitation | 0.45 | ||
| None | 6 (35%) | 150 (52%) | |
| Mild | 10 (59%) | 121 (42%) | |
| Moderate | 1 (6%) | 14 (5%) | |
| Severe | 0 | 4 (1%) | |
| Tricuspid Regurgitation | 0.54 | ||
| None | 2 (10%) | 1 (0.2%) | |
| Mild | 15 (71%) | 329 (78%) | |
| Moderate | 2 (10%) | 63 (15%) | |
| Severe | 2 (10%) | 32 (8%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


