32 Cardiac Pacemakers and Defibrillators
Indications for Implantation of Cardiac Rhythm Devices
Pacemakers
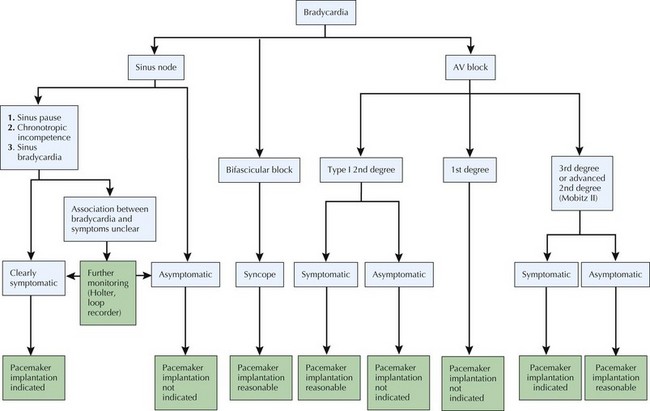
Pacemakers are indicated primarily for patients with symptomatic bradycardia or impressive bradycardia without symptom correlation but associated with a high risk of progression to a symptomatic bradycardia. Precise indications are published in the American College of Cardiology/American Heart Association Guidelines for Pacemaker and ICD Implantation. Symptoms of bradycardia may be subtle (lightheadedness, fatigue) or dramatic (syncope or cardiac arrest). Bradycardia may be the result of dysfunction of the sinus node (referred to as sick sinus syndrome), the atrioventricular node, or the infranodal conduction system. Damage to the conduction system results most commonly from fibrosis or infarction but may be the result of numerous other etiologies, including infection, pharmacologic agents, electrolyte imbalance, or thyroid disease. It is imperative to rule out potentially reversible causes before committing a patient to device-based therapy (Fig. 32-1).
Biventricular Pacemakers
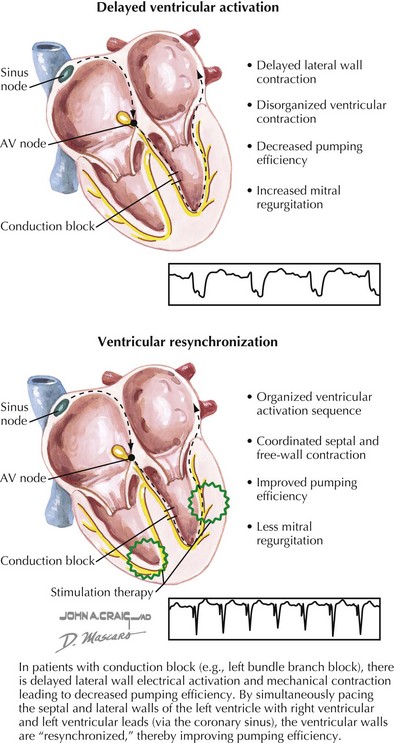
Based on the concept that “dyssynchronous” electrical activation of the left ventricle—as with bundle branch block or right ventricular pacing—translates to inefficiency of cardiac function, biventricular pacing has been developed as a therapeutic approach for patients with impaired cardiac function who would not otherwise have an indication for pacemaker therapy (Fig. 32-2). For instance, in patients with left bundle branch block, delayed electrical activation of the lateral wall of the left ventricle leads to delayed contraction of this same wall. In an individual with normal systolic function, delayed contraction of the lateral wall of the left ventricle may not result in any significant decrement in function. However, in an individual with markedly impaired left ventricular function, the disorganized ventricular contraction resulting from left bundle branch block can result in decreased pumping efficiency and increased mitral regurgitation. By positioning pacemaker leads in the right ventricle and in a lateral branch of the coronary sinus on the epicardium of the left ventricle, simultaneous pacing of both walls of the left ventricle improves ventricular synchrony. Biventricular pacing is indicated for treatment of patients with symptomatic heart failure (New York Heart Association class III or IV) despite optimal medical therapy, reduced left ventricular ejection fraction, and a widened QRS duration (either intrinsically or due to chronic need for pacing).
Implantable Cardioverter Defibrillators
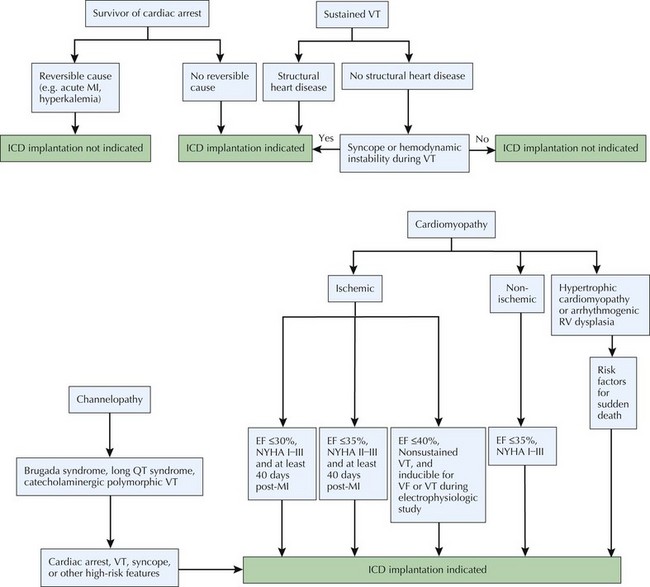
ICDs are indicated for patients with structural heart disease at risk for malignant ventricular tachyarrhythmias (i.e., ventricular tachycardia or ventricular fibrillation). These indications include patients with a prior history of resuscitated cardiac arrest or ventricular tachycardia as well as patients at high risk for future cardiac arrest or ventricular tachyarrhythmia such as a patient with ischemic or nonischemic cardiomyopathy or hypertrophic cardiomyopathy. ICDs are also often indicated in patients with structurally normal hearts who are at high risk for ventricular tachyarrhythmias, such as those with inherited disorders of cardiac rhythm: long QT syndrome, Brugada syndrome, or catecholaminergic polymorphic ventricular tachycardia. The indications for ICD implantation, particularly in patients with tachyarrhythmias, are discussed in detail in this chapter and summarized in Figure 32-3.