, Bryan Wai1 and Quynh A. Truong2
(1)
Harvard Medical School Cardiac MR PET CT Program, Department of Radiology, Massachusetts General Hospital, Boston, MA, USA
(2)
Harvard Medical School Cardiology Division, Department of Medicine and Cardiac MR PET CT Program, Department of Radiology, Massachusetts General Hospital, Boston, MA, USA
Abstract
Non-invasive imaging plays an important role in the management of cardiac diseases. While chest radiography forms a standard part of the diagnostic work-up and follow-up of many cardiac patients, evolving technology related to cardiac computed tomography (CT) and cardiovascular magnetic resonance (CMR) imaging have contributed substantially to the diagnosis and prognosis of various cardiac pathologies. This chapter describes chest radiography findings of cardiopulmonary abnormalities and diseases, including recognition of valvular prostheses as well as pericardial and aortic abnormalities. This is followed by a section on cardiac CT and CMR where scan modes and sequences, indications specific to cardiology and safety issues are addressed.
Abbreviations
ALARA
As Low As Reasonably Achievable
AP
Antero-posterior
bpm
Beats per minute
CABG
Coronary artery bypass graft
CAD
Coronary artery disease
CCS
Coronary calcium score
CHD
Coronary heart disease
CMR
Cardiac magnetic resonance
CT
Computed tomography
CTA
Computed tomography angiography
CXR
Chest X-ray
ECG
Electrocardiogram
Gd
Gadolinium
HR
Heart rate
LA
Left atrial
LV
Left ventricular
mSv
Millisievert
PA
Postero-anterior
RV
Right ventricular
Introduction
Non-invasive imaging plays an important role in the management of cardiac diseases. While chest radiography forms a standard part of the diagnostic work-up and follow-up of many cardiac patients, evolving technology related to cardiac computed tomography (CT) and cardiovascular magnetic resonance (CMR) imaging have contributed substantially to the diagnosis and prognosis of various cardiac pathologies. This chapter describes chest radiography findings of cardiopulmonary abnormalities and diseases, including recognition of valvular prostheses as well as pericardial and aortic abnormalities. This is followed by a section on cardiac CT and CMR where scan modes and sequences, indications specific to cardiology and safety issues are addressed.
Chest Radiography
Advantages
Quick, portable, minimal radiation (0.02 millisieverts [mSv]), useful for serial follow-up
Normal Chest X-ray (CXR) Findings
Heart
Normal cardiothoracic ratio of the heart width to the chest width is <50 % on postero-anterior (PA) projection
Diaphragm
Normal chest expansion on CXR : 6 ± 1 anterior ribs or 9 ± 1 posterior ribs, right hemi-diaphragm higher than the left by up to 3 cm in 95 % of cases
Hila
Left hilum usually higher by approximately 1 cm than the right hilum, equal density
Abnormal CXR Findings
Dextroposition
In situs solitus, the position of the heart is on the right side secondary to a non-cardiac abnormality e.g. scoliosis, pneumonectomy, pulmonary agenesis, right pneumothorax, chronic volume loss or diaphragmatic hernia
Dextrocardia with situs inversus
Heart on the right side with inverted abdominal viscera and lung morphology (Fig. 2-1). Thoracic situs is determined by the anatomy of the trachea and lungs, not the position of aortic arch or cardiac apex

Figure 2-1
Dextrocardia with situs inversus. Frontal CXR demonstrating both the cardiac apical silhouette and gastric air bubble are on the right side. Note the “L” marker on the upper right hand corner signifying left
Dextroversion
Counter-clockwise rotation of a normally developed heart in the right hemithorax. On CXR, the apex is not evident as it lies behind the sternum, the left heart border is formed by the left atrium, the right border is formed by the right ventricle and the right atrium is in a posterior position. The aortic knob is in the normal left-sided position.
“Boot-shaped” heart
Hallmark of Tetralogy of Fallot, due to right ventricular hypertrophy. The apical curvature of the left heart border is elevated “coeur en sabot” (Fig. 2-2a)
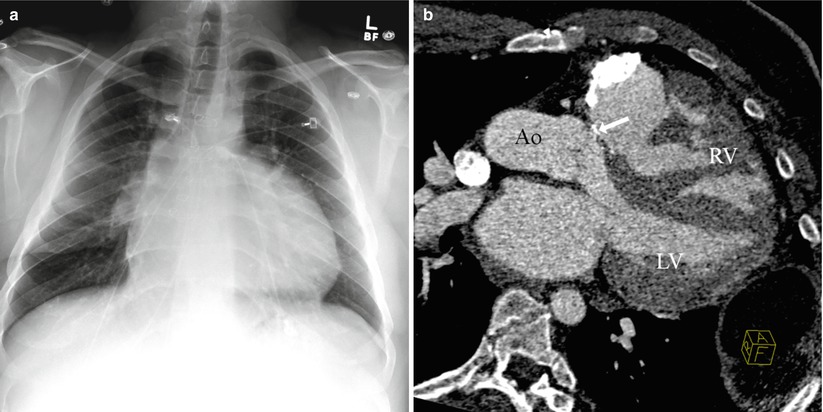
Figure 2-2
Tetralogy of Fallot. (a) CXR showing elevation of the apical curvature of the left heart border known as “coeur en sabot”. (b) Cardiac CT showing an overriding aorta (Ao), ventricular septal defect patch (arrow), and right ventricular (RV) hypertrophy. The pulmonary stenosis is not shown on this CT slice. LV left ventricle
Mediastinal enlargement
Technical factors causing width of mediastinum to appear exaggerated: patient positioning, antero-posterior (AP) projection or incomplete inspiration
Pathological causes: aortic dissection, lymphadenopathy, thyroid, thymus, tumor
Enlarged cardiac silhouette
Pericardial effusion, left ventricular (LV) dilatation, LV aneurysm
Unequal hilar densities
Rotated film, lymph nodes, tumor
Hilar enlargement
Pulmonary hypertension, lymphadenopathy (tuberculosis, sarcoid, lymphoma)
Elevated hemidiaphragm
Loss of lung volume, phrenic nerve palsy (e.g. post coronary artery bypass graft [CABG] surgery), subpulmonic effusion, subphrenic abscess, diaphragmatic rupture (e.g. post trauma), hepatomegaly
Increased translucency in lung fields
Pneumothorax (absent vascular markings with visible lung border), pulmonary hypertension, pulmonary emboli, hyperinflation and bullous changes in chronic obstructive pulmonary disease
Cardiopulmonary Abnormalities/Diseases on CXR
Heart Failure
Cardiomegaly
Kerley A lines: long (2–6 cm), unbranching lines seen coursing diagonally towards the hila caused by distension of anastomotic channels between peripheral and central lymphatics of the lungs. Kerley A lines are not seen without Kerley B or C lines.
Kerley B lines: thickened interlobular septa visible as short linear opacities (1–2 cm) in the subpleural regions indicative of interstitial pulmonary edema
Kerley C lines: seen as fine reticular opacities which may represent anastomotic lymphatics or superimposition of many Kerley B lines. Kerley C lines do not reach the pleura and do not course radially away from the hila
Peribronchial cuffing due to edema of the bronchial walls and peribronchial connective tissues
Poor distinction of lower lobe pulmonary vessels
Greater caliber of upper lobe vessels to lower lung zones
Pulmonary hila become enlarged and hazy
Bilateral patchy alveolar infiltrates (bat’s wing appearance)
Pleural effusions
Chronic left atrial (LA) hypertension results in pulmonary hypertensive changes, right ventricular (RV) dilatation.
LA enlargement
Straightening of LA appendage segment between level of the main pulmonary artery and LV on the left heart border, double density to the right of the spine on PA CXR with increasing LA enlargement, splaying of carina >90°.
Pulmonary embolism
Oligemia
“Westermark sign” a dilatation of the pulmonary vessels proximal to an embolism along with collapse of distal vessels, sometimes with a sharp cutoff
Hampton hump, a triangular or rounded pleural-based infiltrate with the apex pointed toward the hilum, suggestive of pulmonary infarction
Pulmonary hypertension
Gradual taper of caliber between dilated central and hilar pulmonary arteries and smaller peripheral vessels (Fig. 2-3), if secondary to left-to-right shunting, the peripheral shunt vessels branch and extend towards the lung periphery
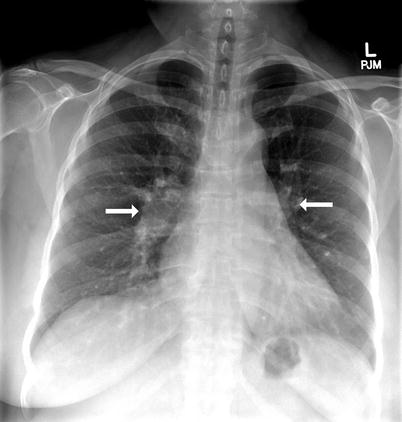
Figure 2-3
Pulmonary hypertension. CXR showing prominence of the main pulmonary artery and dilated left and right pulmonary arteries (arrows) associated with pruning of the peripheral pulmonary vasculature
Reduced pulmonary blood flow
Small caliber central and hilar pulmonary arterial branches, reduced pulmonary vascular markings, seen in Tetralogy of Fallot, pulmonary atresia with ventricular septal defect, Ebstein’s anomaly, tricuspid atresia
Right ventricular hypertrophy
Right ventricle is a midline and anterior structure and thus does not form a cardiac border in the PA projection, however in RV hypertrophy the apex may be elevated from the diaphragm and the left lower cardiac contour may become more rounded
Scimitar syndrome
Partial or total anomalous pulmonary venous return of the right lung veins to the inferior vena cava just above or below the diaphragm, frequently associated with right lung and right pulmonary artery hypoplasia
PA CXR: decrease in the size of the right thorax, shift of mediastinal structures and heart to the right, presence of anomalous vein “scimitar” as a vertical structure coursing towards the right cardiophrenic angle closely in parallel with the right atrial border
Pericardial Abnormalities
Pericardial Effusion
An abrupt asymmetrical change in the dimension of the cardiac silhouette without a change in the cardiac chamber size, larger effusions result in the appearance of a ‘globular’ shaped heart, ‘fat pad’ sign on lateral CXR is positive when an anterior pericardial stripe (separation by pericardial fluid between the pericardial fat posteriorly from the mediastinal fat anteriorly) is thicker than 2 cm
Echocardiography most commonly used to confirm the diagnosis
Pericardial calcification
Irregular calcification along the heart border, coexisting cardiac enlargement if large pericardial effusion (Fig. 2-4)
Figure 2-4
Pericardial calcification. (a) CXR and (b) CT image demonstrating calcification along the inferior cardiac border (arrow)
Pericardial cyst
Well demarcated, rounded mass more commonly near the right cardiophrenic border than the left cardiophrenic border, can have a pointed upper border, pericardial diverticulae changes contours and size during deep inspiration
Congenital absence of the pericardium
“Snoopy sign” with displacement of the LV and pulmonary artery towards the left side
Abnormalities of the Aorta
Calcification usually signifies degenerative intimal change, such as from atherosclerosis
Coarctation
“3” sign due to diminution of aortic arch segment with a concave notch in the proximal descending aorta and interruption of the descending aorta shadow distal to the coarctation, rib notching evident if retrograde collateral flow to the post-coarctation aorta by dilated intercostal arteries (Fig. 2-5a)
Figure 2-5
Aortic coarctation. (a) CXR showing left sided rib notching (arrow) due to retrograde collateral flow to the post-coarctation aorta by dilated intercostal arteries. (b) Cardiac Magnetic Resonance angiography demonstrating the aortic coarctation in the same patient
Thoracic aorta dilatation
Increased curvature of the mid right heart border on PA projection or anterior aortic border on lateral projection suggest ascending aortic enlargement
Aortic dissection
Prominent aortic arch from hypertension, atherosclerosis, connective tissue disorders, vasculitis, bicuspid aortic valve, blunt chest trauma or iatrogenic causes
Abnormal if diameter >4 cm, focal pathological dilatation especially with widening of the arch beyond the origin of the left subclavian artery (Fig. 2-6a)
Figure 2-6
Aortic dissection. (a) CXR demonstrating a widened mediastinum (>4 cm, white arrows) in a patient with aortic dissection after blunt chest trauma. (b) Cardiac CT confirms a DeBakey Type 1 aortic dissection where the intimal tear/dissection flap (black arrows) originates in the ascending aorta and propagates to the aortic arch and descending aorta
Other CXR findings may include obliteration of the aortic knob, tracheal deviation, depression of the left main stem bronchus
Pleural effusions, usually left sided, are associated with descending aortic dissection
Right-sided aortic arch
The descending aorta typically runs parallel to the spine in continuity to the aortic arch on the left side on PA CXR, except in cases of a right sided aortic arch
Identification of Valvular Prostheses on CXR (Fig. 2-7)
Figure 2-7
(a) Frontal and (b) Lateral CXR demonstrating the anatomic relationship of a patient with prosthetic aortic (AV) and mitral valve (MV) replacements and tricuspid valve (TV) annuloplasty ring. The AV is situated higher and is smaller and more anterior to the mitral valve on the lateral CXR. The TV annuloplasty ring is aligned medial-laterally and is positioned to the right of and below the AV
Apart from homografts, prosthetic valves are radio-opaque
Caged valves and heterografts: direction of flow is from the base ring to the struts
Disc valves: the direction of flow is appreciated if the disc is seen in an open position
Aortic valve
The opening of the valve ring is directed more vertically, facing obliquely and to the right, aortic valve is usually higher, smaller and more anterior to the mitral valve on lateral CXR, perceived direction of blood flow is towards the ascending aorta
Mitral valve
Situated lower and more to the left than aortic valves, perceived direction of flow is towards the apex
Tricuspid valve
Aligned in a medial-lateral direction, to the right of mitral valve and below the aortic valve
Cardiac Computed Tomography (CT)
Most current multi-detector CT scanners (64-, 256- and 320-slice scanners) have similar spatial resolution, however the increased detector slices and larger detector width allow more coverage of the heart in each heartbeat. Dual source CT scanners consist of two X-ray tube sources leading to improved temporal resolution to 75 ms. Spatial resolution is how close two objects can be discernible from each other. Temporal resolution is how fast an image could be acquired such that motion does not create image blurring, similar to the shutter speed of a camera.
Advantages and Disadvantages of Cardiac CT (Table 2-1)
Table 2-1
Advantages and disadvantages of cardiac CT
Advantages of CT | Disadvantages of CT |
|---|---|
Rapid scan acquisition | Ionizing radiation |
Excellent isotropic spatial resolution (XYZ plane) | Iodinated contrast complications e.g. extravasation, allergy, nephropathy |
Compatible with metal devices | Metal devices causes beam hardening artifacts |
Contrast able to be hemodialyzed | Diagnostic accuracy may be reduced by heart rate >70 beats per minute (bpm), irregular rhythm, severe coronary calcification, inability to sustain breath hold for at least 5–10 seconds |
Allows arterial, venous and functional cardiac assessment | Less accurate assessment of coronary stents with diameter <3 mm |
CT Scan Acquisition Modes (Table 2-2)
Table 2-2
CT scan acquisition modes
CT scan mode | Scan technique | Advantages | Disadvantages |
|---|---|---|---|
Non-contrast enhanced scans | |||
Calcium score | Non-contrast scan where calcium (>130 Hounsfield Units) is detected | Non-contrast prognostic information | Does not assess stenosis severity or other plaque morphology (non-calcified or mixed plaques) |
Contrast enhanced scans | |||
Non-ECG gated | Scan acquisition without ECG synchronization | More readily available scanners and technologists | Motion artifact |
Adequate for most aorta and pulmonary assessment | Not adequate for coronary or aortic root evaluation | ||
Prospective ECG-triggered | Images acquired at a pre-defined set duration after the QRS complex | Radiation reduction as X-ray tube on only at pre-determined phase of the cardiac cycle | No functional assessment, potential for misregistration or slab artifacts if ectopy or heart rate variability |
Retrospective ECG-gated | X-ray current continuously delivered throughout the cardiac cycle | Functional assessment Allows reconstruction at multiple points in the cardiac cycle | Higher radiation |
Appropriate CT Indications
Appropriate CT indications: 2010 Appropriate use criteria for cardiac computed tomography [1].
A.
Indications for non-contrast coronary calcium score (CCS)
Risk assessment in asymptomatic patients without known coronary artery disease (CAD):
At intermediate risk of CAD (correlates with 10-year absolute coronary heart disease [CHD] risk between 10 and 20 %)
At low risk of CAD (correlates with 10-year absolute CHD risk <10 %) with a family history of premature CAD
Patients with an Agatston score of >400 have a tenfold increased risk of cardiac events compared to a score of 0 [2]
The absence of calcium does not imply no significant coronary stenosis as 8–10 % of stenoses can be caused by non-calcified plaque.
B.




Indications for CT angiography (CTA)
< div class='tao-gold-member'>
Detection of CAD in symptomatic patients without known CAD who present with:
Non acute symptoms (stable chest pain) possibly representing an ischemic equivalent with
intermediate pretest probability of CAD, or
low pretest probability of CAD with uninterpretable electrocardiogram (ECG) or unable to exercise
Acute symptoms with suspicion of acute coronary syndrome, low to intermediate pretest probability of CAD without high risk ECG changes or elevated cardiac biomarkers (Fig. 2-8)

Figure 2-8
Severe stenosis in the left anterior descending artery (LAD) due to non-calcified plaque (arrow). Curved multi-planar reformat cardiac CTA image in a patient presenting with acute chest pain and low-intermediate pre-test probability of acute coronary syndrome without elevated cardiac biomarkers or ischemic ECG changes
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


