Cardiac Imaging
Ellen Mayer Sabik • Brian P. Griffin
QUESTIONS
1.The three-dimensional (3D) transesophageal echocardiographic (TEE) image in Figure 14.1 demonstrates a patient with
a.normally functioning bioprosthetic mitral valve replacement (MVR).
b.normally functioning bileaflet mechanical MVR.
c.mitral valve (MV) endocarditis with a vegetation.
d.abnormal mechanical MVR.
e.abnormal bioprosthetic MVR.

Figure 14.1
2.The images in Figure 14.2A–E come from an 18-year-old young man with marked shortness of breath (SOB). The most appropriate course of action would be
a.closed mitral commissurotomy because he has a split score of 0 to 4 and minimal mitral regurgitation (MR).
b.percutaneous mitral valvuloplasty (PMV) because he has a split score of 4 to 8 and minimal MR.
c.surgical MVR because he has a split score of 8 to 12 and minimal MR.
d.surgical MVR because he has a split score of 0 to 4 with significant MR.
e.surgical MVR because he has a split score of 4 to 8 and significant MR.

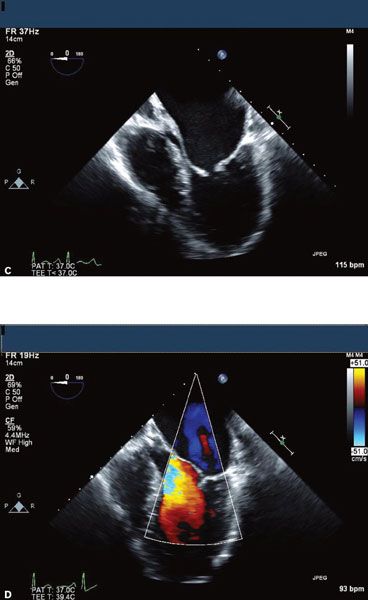

Figure 14.2
3.The images in Figure 14.3A–C belong to a 65-year-old woman with lung cancer and a central venous catheter for chemotherapy. The structure seen on these images is most likely to be
a.prominent Chiari network.
b.implantable cardioverter-defibrillator (ICD) wire.
c.right atrial (RA) thrombus or thrombus on central venous catheter.
d.RA myxoma.
4.The images in Figure 14.4A and B are associated with which of the following?
a.Moderate risk of endocarditis
b.No risk of heart failure
c.Large jugular venous v waves
d.Radiofemoral delay

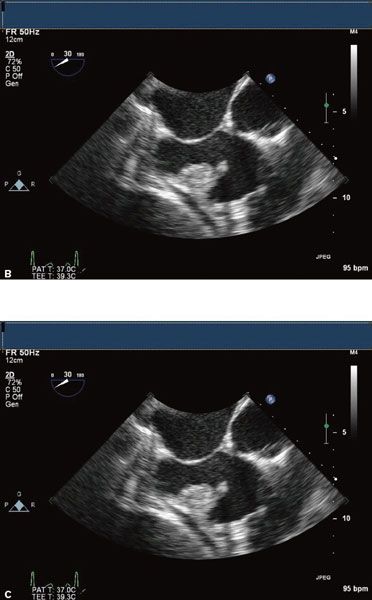
Figure 14.3
5.The images in Figure 14.5A–C are from a 43-year-old s/p carpentier edwards aortic valve replacement (CE AVR) with fevers and night sweats. These images demonstrate all of the following except
a.paravalvular abscess.
b.fistula.
c.aortic stenosis (AS).
d.aortic insufficiency (AI).
e.vegetations.
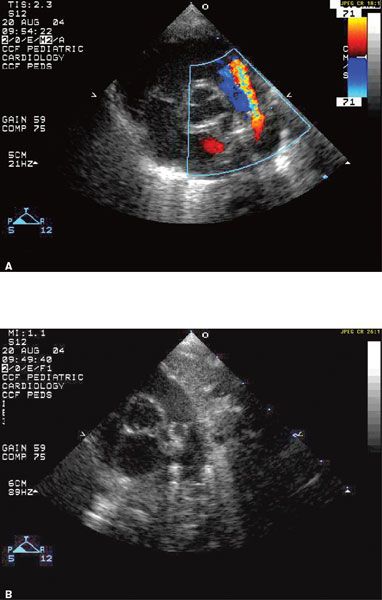
Figure 14.4
6.The images in Figure 14.6A and B are from a transthoracic echocardiogram (TTE) from a patient who is a 57-year-old woman with lung cancer who presents with chest pain (CP) and SOB. The most likely cause of her CP and SOB based on these images is
a.myocardial infarction (MI).
b.aortic dissection.
c.pericardial effusion with pericarditis/tamponade.
d.pulmonary embolus.
e.pneumonia.
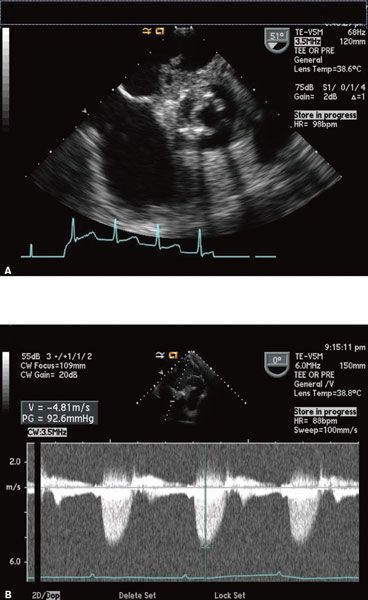

Figure 14.5
7.The patient is a 70-year-old woman with a history of hypertension, but no prior cardiac history, who comes in with sudden onset of CP, which later migrates to her back. She is diagnosed with a computed tomography (CT) of her chest to have a type I aortic dissection. Her blood pressure is 100/70 mmHg and her heart rate is 115 bpm. Images from her TTE are in Figures 14.7A–C. The next step in her care would be
a.aortic stent graft.
b.coronary angiography.
c.intraaortic balloon pump placement.
d.pericardiocentesis.
e.emergent cardiac surgery.
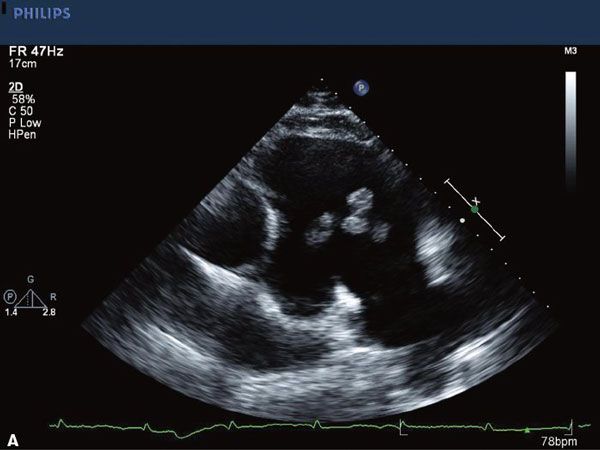
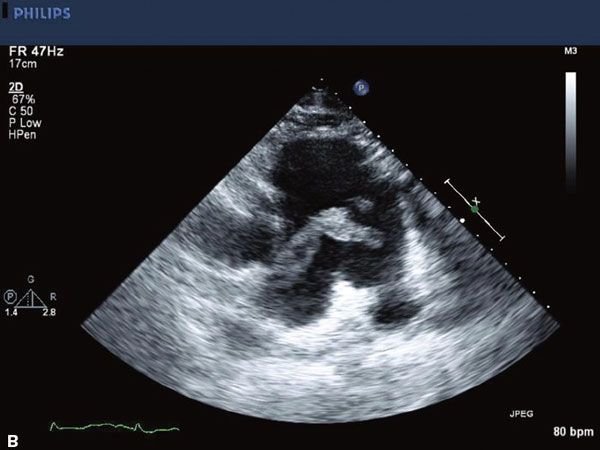
Figure 14.6
8.The finding in the transthoracic images in Figure 14.8A and B is commonly associated with which of the following lesions?
a.Congenitally corrected transposition
b.Cleft MV
c.Coarctation of the aorta
d.Right ventricular (RV) infarction
e.Bicuspid aortic valve (AV)
9.A 36-year-old man with a history of hypertension on medications for 5 years presents to your office with complaints of dyspnea on exertion and is found by his internist to have a heart murmur. Below are some representative views from his TTE (Fig. 14.9A–E). What is the diagnosis?
a.Patent ductus arteriosus (PDA)
b.Rheumatic AV with AI
c.Rheumatic AS
d.Coarctation of the aorta with bicuspid AV with AI
e.Marfan’s with aortic dissection
10.A 37-year-old patient presents with fever, weight loss, and blood cultures that are positive for Pseudomonas and the transthoracic echo finding in Figure 14.10. The patient’s most likely demographic for this clinical scenario is
a.patient with hypertrophic obstructive cardiomyopathy (HOCM) who had a dental procedure 3 weeks ago.
b.patient with myxomatous MV disease with mitral valve prolapse (MVP).
c.patient with subaortic stenosis after dental procedure 3 weeks ago.
d.patient with a patent ductus.
e.intravenous (IV) drug abuser.
11.This M-mode tracing (Fig. 14.11) demonstrates a patient with
a.HOCM with systolic anterior motion (SAM) of the MV leaflets.
b.MVP.
c.AS.
d.rheumatic mitral stenosis (MS).
e.severe left ventricular (LV) dysfunction.
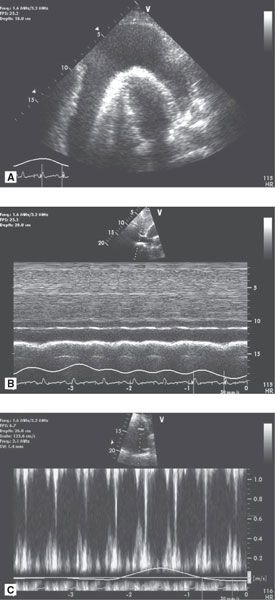
Figure 14.7 • A. Apical four-chamber view (TTE). B. M-mode through the IVC in the subcostal view (TTE). C. Continuous-wave Doppler through the mitral valve showing mitral valve inflow pattern.
12.The following TEE image (Fig. 14.12) demonstrates a patient with
a.trileaflet AV.
b.bicuspid AV with fusion of right coronary cusp (RCC) and noncoronary cusp (NCC).
c.bicuspid AV with fusion of RCC and LCC.
d.bicuspid AV with fusion of left coronary cusp (LCC) and NCC.
e.unicuspid AV.
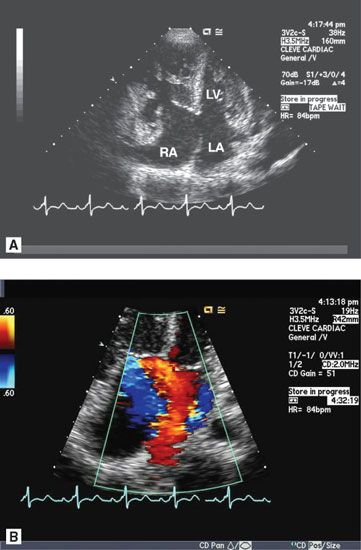
Figure 14.8 • A. Apical four-chamber view (TTE). B. Apical four-chamber view with color Doppler.
13.The patient is a 22-year-old with a systolic and diastolic murmur with the following echo images (Fig. 14.13A and B). These images demonstrate
a.membranous ventricular septal defect (VSD).
b.supracristal VSD.
c.Ebstein anomaly.
d.pulmonic stenosis (PS)/pulmonic insufficiency.
e.PDA.
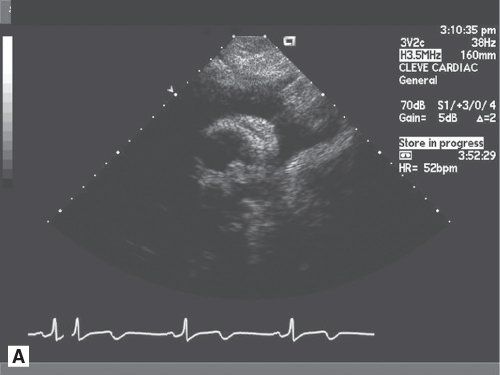
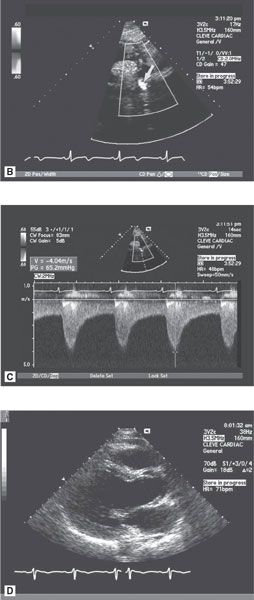

Figure 14.9 • A. Suprasternal notch view in 2D (TTE). B. Suprasternal notch with color Doppler. C. Continuous-wave Doppler in the descending aorta from the suprasternal notch. D. Parasternal long-axis view in systole. E. Parasternal long-axis view with color Doppler.

Figure 14.10 • Mid-esophageal short-axis view of the aortic valve (TEE).
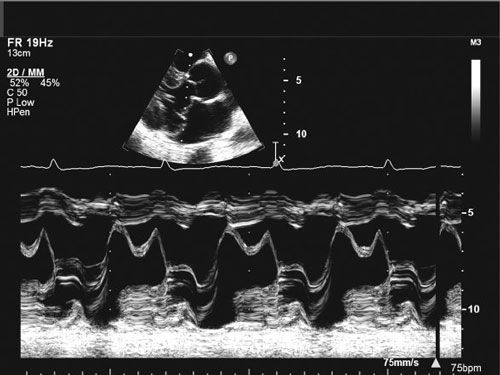
Figure 14.11 • M-mode through the mitral valve.

Figure 14.12 • Mid-esophageal short-axis view of the aortic valve (systole).
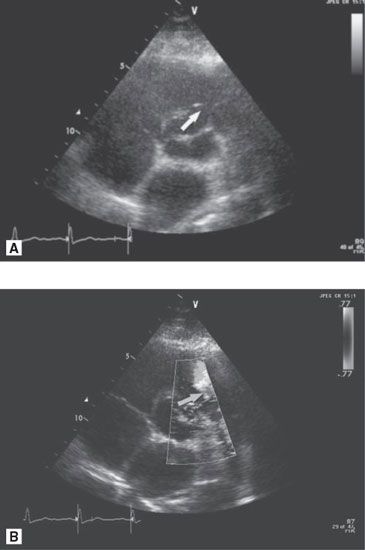
Figure 14.13 • A. Parasternal short-axis view. B. Parasternal short-axis view with color Doppler.
14.A 46-year-old woman with dyspnea on exertion with occasional palpitations has the following surface echo images (Fig. 14.14A–D). Her dyspnea on exertion can be explained by
a.myxomatous MV disease with MR.
b.rheumatic MV disease with MS and MR.
c.endocarditis with vegetation causing MR.
d.severe mitral annular calcification.
e.cleft mitral leaflet.

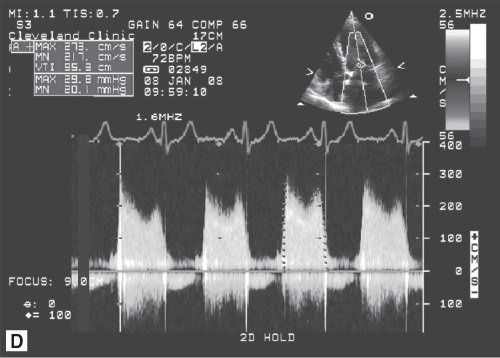
Figure 14.14 • A. Parasternal long-axis view. B. Parasternal long-axis view with color Doppler. C. Apical four-chamber view with color Doppler of the mitral valve. D. Continuous-wave Doppler through the mitral valve.
15.This parasternal short-axis view (Fig. 14.15) would be most consistent with which of the following patients?
a.Patient with severe MR
b.Patient with severe AI
c.Patient with severe tricuspid regurgitation (TR)
d.Patient with severe LV systolic dysfunction
e.Patient with a subaortic membrane

Figure 14.15 • Parasternal short-axis view (diastole).
16.The TEE images below are from a patient who has marked dyspnea on exertion and one episode of presyncope (Fig. 14.16A–C). The patient is now in the operating room for a procedure. The most appropriate operation for this patient would be
a.MV repair.
b.septal myectomy.
c.MVR.
d.coronary artery bypass grafting (CABG).
e.ascending aortic conduit.
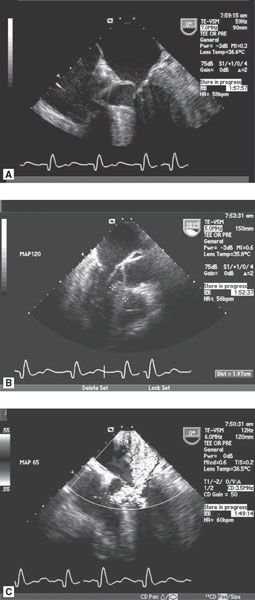
Figure 14.16 • A. Mid-esophageal four-chamber view (TEE). B. Mid-esophageal long-axis view (TEE). C. Mid-esophageal four-chamber view with color Doppler.
17.The following TEE images (Fig. 14.17A and B) demonstrate a large mass noted in the LV apex. This mass is located in a region of myocardial thinning and akinesis in a dilated LV. Although there is some mobility there does not appear to be a stalk. This mass is most likely which of the following possibilities?
a.Teratoma
b.Myosarcoma
c.Fibroelastoma
d.Thrombus
e.Adenocarcinoma
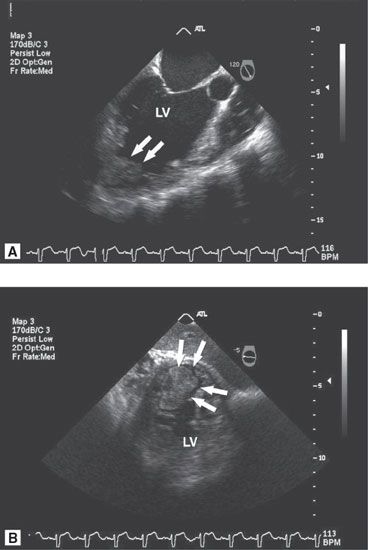
Figure 14.17 • A. Mid-esophageal long-axis view (TEE). B. Transgastric short-axis view of the LV (TEE).
18.The patient is a 56-year-old man with hypertension, diabetes, and obesity who was admitted 6 months ago to an outside hospital with a late presentation of an anterior MI. He presented approximately 3 days post MI and underwent cardiac catheterization at 1 week, which showed a total occlusion in the mid-left anterior descending artery (LAD), severe stenoses of the first and second diagonals, and no significant disease in either the right coronary artery (RCA) or left circumflex artery (LCx). The patient was then referred to your hospital for revascularization. The patient, however, failed to show for his appointment and finally presented 8 months later with CP and SOB. Prior to revascularization you order a positron emission tomography (PET) rubidium (Rb)/fluorodeoxyglucose (FDG) using Rubidium82/F18A (flourine-18–labeled deoxyglucose) to determine the degree of inducible ischemia and viability. The images obtained are in Figure 14.18. The images from the PET scan demonstrate
a.scar in the LAD territory.
b.inducible ischemia in the LAD territory.
c.hibernating myocardium in the LAD territory.
d.a combination of inducible ischemia and hibernation in the LAD territory.
e.scar in the RCA territory.
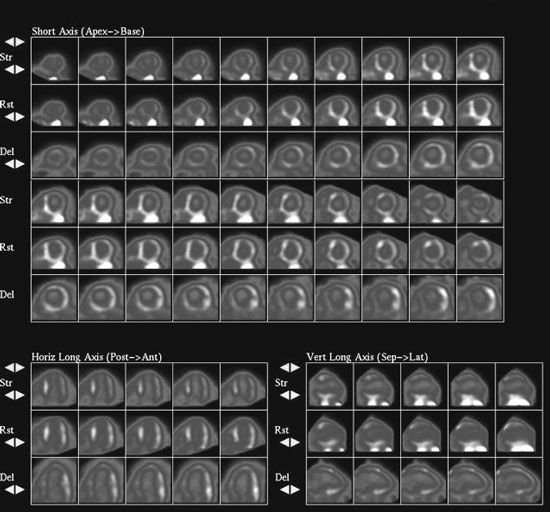
Figure 14.18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


