Our concepts of heart disease are based on the enormous reservoir of physiologic and anatomic knowledge derived from the past 80 years of experience in the cardiac catheterization laboratory. As Andre Cournand remarked in his Nobel lecture of December 11, 1956, “the cardiac catheter was … the key in the lock.”
1 By turning this key, Cournand and his colleagues led us into a new era in the understanding of normal and disordered cardiac function in humans.
According to Cournand,
2 cardiac catheterization was first performed (and so named) by Claude Bernard in 1844. The subject was a horse, and both the right and left ventricles were entered by a retrograde approach from the jugular vein and carotid artery. In an excellent review of the history of cardiac catheterization, angiography, and interventional cardiology, Mueller and Sanborn
3 describe and cite references for experiments by Stephen Hales and others whose work antedates that of Claude Bernard. It is Stephen Hales who perhaps can be credited with the first invasive hemodynamic assessment, as he measured the blood pressure of a horse by inserting a brass rod in the femoral artery and observing the column of blood rising in a 9-foot glass tube connected to the brass rod. In further experiments, which he published in 1733, he proceeded toward identifying how much blood goes through the heart in one minute and determining the capacity of the left ventricle.
4Although Claude Bernard may not have been the first to perform cardiac catheterization, his careful application of scientific method to the study of cardiac physiology using the cardiac catheter demonstrated the enormous value of this technical innovation and provided the inspiration for the future development of cardiac catheterization. In 1861, Chaveau and Marey published their work on the measurement of intracardiac pressure. They were able to determine that ventricular systole and apical beat are simultaneous, and they were able to perform the first simultaneous measurement of left ventricular (LV) and central aortic pressures. An era of investigation of cardiovascular physiology in animals then followed, resulting in the development of many
important techniques and principles (pressure manometry, the Fick cardiac output method), which awaited direct application to the patient with heart disease.
Werner Forssmann is credited with performing the first cardiac catheterization of a living person—himself.
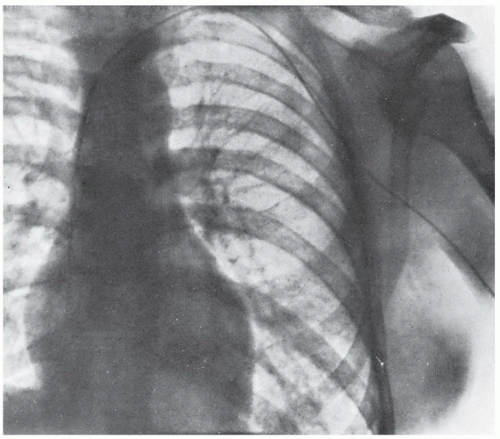
5 At age 25, while receiving clinical instruction in surgery in Germany, he passed a 65 cm catheter through one of his left antecubital veins, guiding it by fluoroscopy until it entered his right atrium. He then walked to the radiology department (which was on a different level, requiring that he climb stairs), where the catheter position was documented by a chest roentgenogram (
Figure 1.1). During the next 2 years, Forssmann continued to perform catheterization studies, including six additional attempts to catheterize himself. Bitter criticism, based on an unsubstantiated belief in the danger of his experiments, caused Forssmann to turn his attention to other concerns, and he eventually pursued another catheterrelated career as a urologist.
6 Nevertheless, for his contribution and foresight he shared the Nobel Prize in Medicine with Andre Cournand and Dickinson Richards in 1956.
Forssmann’s primary goal in his catheterization studies was to develop a therapeutic technique for the direct delivery of drugs into the heart. He wrote:
If cardiac action ceases suddenly, as is seen in acute shock or in heart disease, or during anesthesia or poisoning, one is forced to deliver drugs locally. In such cases the intracardiac injection of drugs may be life saving. However, this may be a dangerous procedure because of many incidents of laceration of coronary arteries and their branches leading to cardiac tamponade, and death. … Because of such incidents, one often waits until the very last moment and valuable time is wasted. Therefore I started to look for a new way to approach the heart, and I catheterized the right side of the heart through the venous system.
5Others, however, appreciated the potential of using Forssmann’s technique as a diagnostic tool. In 1930, Klein reported 11 right heart catheterizations, including passage to the right ventricle and measurement of cardiac output using
Fick’s principle
7. In 1932, Padillo and coworkers reported right heart catheterization and measurement of cardiac output in two subjects.
2 Except for these few early studies, application of cardiac catheterization to study the circulation in normal and disease states was fragmentary until the work of Andre Cournand and Dickinson Richards, who separately and in collaboration produced a remarkable series of investigations of right heart physiology in humans.
8,
9,
10 In 1947, Dexter reported his studies on congenital heart disease and passed the catheter to the distal pulmonary artery, describing “the oxygen saturation and source of pulmonary capillary blood” obtained from the pulmonary artery “wedge” position.
11 Subsequent studies from Dexter’s laboratory
12 and by Werko
13 elaborated the use of this pulmonary artery wedge position and reported that the pressure measured at this position was a good estimate of pulmonary venous and left atrial pressure. During this exciting early period, catheterization was used to investigate problems in cardiovascular physiology by McMichael and Sharpey-Shafer in England,
14 Lenègre and Maurice in Paris,
15 and Warren, Stead, Bing, Dexter, Cournand, and others in the United States.
16,
17,
18,
19,
20,
21,
22,
23Further developments came rapidly in the 1950s and 1960s. Retrograde left heart catheterization was first reported by Zimmerman and others
24 and Limon-Lason and Bouchard
25 in 1950. The percutaneous (rather than cutdown) technique was developed by Seldinger in 1953 and was soon applied to cardiac catheterization of both the left and right heart chambers.
26 Transseptal catheterization was first developed by Ross
27 and Cope
28 in 1959 and quickly became accepted as a standard technique. Selective coronary arteriography was reported by Sones and others in 1959 and was perfected to a remarkable excellence over the ensuing years.
29,
30 Coronary angiography was modified for a percutaneous approach by Ricketts and Abrams
31 in 1962 and Judkins
32 in 1967. In 1970 Swan and Ganz introduced a practical balloon-tipped, flow-guided catheter technique enabling the application of catheterization outside the laboratory,
33 and in 1977, Andreas Gruntzig introduced the technique of balloon angioplasty, generally known as percutaneous transluminal coronary angioplasty (PTCA),
34,
35 thus expanding the use of cardiac catheterization to therapeutic interventions and spearheading its future exponential growth.
INTERVENTIONAL CARDIOLOGY
The most significant change in the last 30 years has been the evolution of the therapeutic potential of the cardiac catheter. With rapidly evolving technology and expanding indications, PTCA grew to equal stature with coronary artery bypass grafting (CABG) as the number of annual PTCA procedures grew to 300,000 by 1990. Encouraged by the success of PTCA but challenged by its shortcomings, physician and engineer inventors have developed and introduced into clinical practice a panoply of new percutaneous interventional devices over the past decade. This includes various forms of catheter-based atherectomy, bare metallic stents, and drug-eluting stents, which together have largely solved earlier problems relating to elastic recoil, dissection, and restenosis of the treated segment (see
Chapters 28,
29,
30 and
31). These newer techniques are usually subsumed (along with conventional balloon angioplasty) under the broader designation of percutaneous coronary intervention (PCI). Similar techniques have also developed in parallel for the treatment of peripheral arterial atherosclerotic disease, which is a common cause of morbidity and even mortality in patients with coexisting coronary disease (see
Chapters 19,
34, and
37).
The evolution of PCI has also stimulated the development of other techniques for the treatment of
structural heart disease (see
Chapter 32). Catheter devices developed to close intracardiac shunts in pediatric patients have now been adapted to close adult congenital and acquired defects (see
Chapter 35). Balloon valvuloplasty was developed in the mid-1980s and remains successful for the treatment of rheumatic mitral stenosis. Due to early recurrence, balloon aortic valvuloplasty is now used as a treatment for aortic stenosis only in patients who are not candidates for aortic valve replacement surgery or in preparation for percutaneous aortic valve replacement. Newer technologies for percutaneous aortic valve replacement and percutaneous reduction of mitral regurgitation are now available as alternative therapies to open heart surgery in selected patient populations (see
Chapter 33).
In essence, these new procedures have made interventional cardiology a new field in cardiovascular medicine, whose history is well summarized by Spencer King,
36 and the interested reader is referred there for further historical details. But it is thus clear in the 21st century that interventional cardiology—by virtue of its new technologies, potent adjunctive drug therapies, expanding indications, and improving results—has blossomed. In many ways, these therapeutic modalities (rather than purely diagnostic techniques) have now become the centerpiece within the broad field of cardiac catheterization.
Although the emphasis thus lies appropriately on this dynamic field of catheter-based intervention, we can ill afford to lose sight of the basic principles of catheter insertion, hemodynamic measurement, high-quality angiography, and integration of catheterization findings with the overall clinical scenario as the foundations on which all current interventional techniques are built and from which future evolution of cardiac catheterization will proceed.
INDICATIONS FOR CARDIAC CATHETERIZATION
As performed today, cardiac catheterization is a combined hemodynamic and angiographic procedure undertaken for diagnostic and often therapeutic purposes. As with any invasive procedure, the decision to perform cardiac catheterization
must be based on a careful balance of the risk of the procedure against the anticipated benefit to the patient. Indications for the use of catheterization and coronary intervention in the management of stable angina, unstable angina, and ST-elevation myocardial infarction (MI) have been developed by the American College of Cardiology (ACC) and the American Heart Association (AHA),
37,
38,
39 and are available online at <http://www.cardiosource.org/>.
The basic principle is that cardiac catheterization is recommended to confirm the presence of a clinically suspected condition, define its anatomic and physiologic severity, and determine the presence or absence of associated conditions when a therapeutic intervention is planned in a symptomatic patient. The most common indication for cardiac catheterization today thus consists of a patient with an acute coronary ischemic syndrome (unstable angina or acute MI) in whom an invasive therapeutic intervention is contemplated. The goal of cardiac catheterization in such patients is to identify the culprit lesions and then to restore vessel patency via PCI. In a few such patients, the diagnostic portion of the catheterization procedure may reveal other features (e.g., complex multivessel or left main coronary disease, severe associated valvular disease), which provide critical information for the decision and planning of open heart surgery.
Although few would disagree that consideration of heart surgery is an adequate reason for the performance of catheterization, clinicians differ about whether
all patients being considered for heart surgery should undergo preoperative cardiac catheterization and coronary angiography. According to the most recent update of the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease, “
Coronary angiography is not indicated in young patients undergoing nonemergency valve surgery when no further hemodynamic assessment by catheterization is deemed necessary and there are no coronary risk factors, no history of CAD, and no evidence of ischemia. (
Level of Evidence: C)”.
40 Thus, many young patients with echo-proven valvular disease and no symptoms of myocardial ischemia are sometimes operated on using only noninvasive data. However, the risks of catheterization in such patients are extremely small, particularly compared to the risk of embarking on cardiac surgery on a patient for whom an incorrect clinical diagnosis or the presence of an unsuspected additional condition greatly prolongs and complicates the planned surgical approach. Therefore, the current guidelines still recommend cardiac catheterization in patients who might be at higher risk of coronary artery disease independent of age, or in patients for whom additional information might be required. By providing the surgical team with a precise and complete road map of the course ahead, cardiac catheterization can permit a carefully reasoned and maximally efficient operative procedure. Furthermore, information obtained by cardiac catheterization may be invaluable in the assessment of crucial determinants of prognosis, such as LV function, status of the pulmonary vasculature, and the patency of the coronary arteries. For these reasons, we recommend cardiac catheterization (or at least coronary angiography) in nearly all patients for whom heart surgery is contemplated, even if the severity of valve disease and ventricular function have been determined by preoperative echocardiography.
Catheterization data can also inform other nonsurgical therapeutic considerations. For example, the decision for pharmacologic intervention with heparin and/or a thrombolytic agent in suspected acute pulmonary embolism, the use of high-dose beta-blocker and/or calcium antagonists in suspected hypertrophic obstructive cardiomyopathy (versus catheter-based alcohol septal ablation) might well be considered of sufficient magnitude to warrant confirmation of the diagnoses by angiographic and hemodynamic investigation prior to the initiation of therapy. Although a clinical diagnosis of primary pulmonary hypertension can often be made by echocardiography, cardiac catheterization is usually required (a) to confirm the diagnosis and (b) to assess potential responsiveness to pharmacologic agents. Catheterization can also be used to optimize pharmacologic therapy for advanced congestive heart failure.
Another broad indication for performing cardiac catheterization is to aid in the diagnosis of obscure or confusing problems, even when a major therapeutic decision is not imminent. A common instance of this indication is presented by the patient with chest pain of uncertain cause, when there is confusion regarding the presence of obstructive coronary artery disease. Both management and prognosis of this difficult problem can be greatly simplified when it is known, for example, that the coronary arteries are widely patent. However, more recently CT angiography (CTA) has emerged as a new imaging modality and has been replacing invasive coronary angiography as a diagnostic tool to rule out coronary artery disease in this setting. Another example within this category is the symptomatic patient with a suspected diagnosis of cardiomyopathy. Although some may feel satisfied with a clinical diagnosis of this condition, the implications of such a diagnosis in terms of prognosis and therapy are so important that we feel it worthwhile to be aggressive in ruling out potentially correctable conditions (e.g., hemochromatosis, pericardial effusive-constrictive disease) with certainty, even though the likelihood of their presence may appear remote on clinical grounds.
Research
On occasion, cardiac catheterization is performed primarily as a research procedure. Although research is conducted to some degree in many of the diagnostic and therapeutic studies performed at major medical centers, it usually relates to the evaluation of new therapeutic devices (e.g., new stent designs) in patients who would be undergoing diagnostic and therapeutic catheterization in any event. All such studies
41 require prior approval of the Food and Drug Administration (FDA) in the form of an Investigational Device Exemption, of the local Committee on Human Research at the institution (Institutional Review Board, or IRB), and attainment of informed consent after the details of the risks and potential
benefits of the procedure and its alternatives have been thoroughly explained. Doing such research also requires meticulous attention to protocol details, inclusion/exclusion criteria, data collection, and prompt reporting of any complications.
Even so, this is quite different from a catheterization that is performed solely for the purpose of a research investigation (as a 6-month follow-up angiogram after a new stent might be). Such studies should be carried out only by or under the direct supervision of an experienced investigator who is expert in cardiac catheterization, using a protocol that has been carefully scrutinized and approved by the IRB (Human Use Committee) at the investigator’s institution.