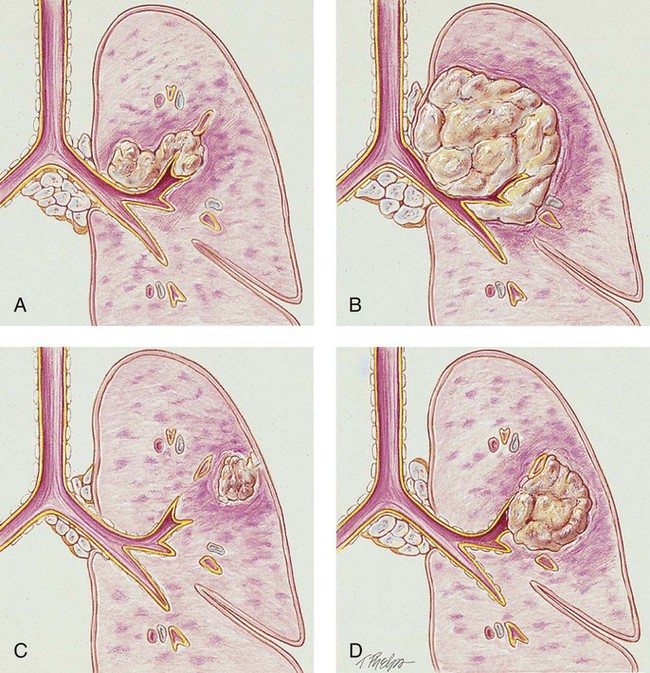
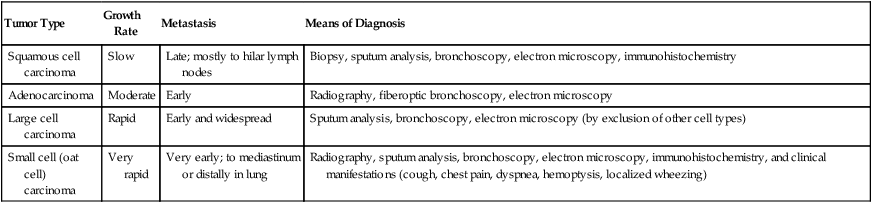
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with cancer of the lung. • Describe the causes of cancer of the lung. • List the cardiopulmonary clinical manifestations associated with cancer of the lung. • Describe the general management of cancer of the lung. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. The major pathologic or structural changes associated with bronchogenic carcinoma are as follows: • Inflammation, swelling, and destruction of the bronchial airways and alveoli • Tracheobronchial mucous accumulation and plugging • Airway obstruction (either from blood, from mucous accumulation, or from a tumor projecting into a bronchus) • Pleural effusion (when a tumor invades the parietal pleura and mediastinum) Environmental or occupational risk factors for lung cancer include the following: • Benzopyrene and radon particles associated with uranium mining • Radiation and nuclear fallout • Polycyclic aromatic hydrocarbons and arsenicals There are four major types of bronchogenic tumors: (1) squamous (epidermoid) cell carcinoma, (2) adenocarcinoma (including bronchial alveolar cell carcinoma), (3) large cell carcinoma, and (4) small cell (oat cell) carcinoma (see Figure 26-1). For therapeutic reasons, these bronchogenic tumors are commonly divided into the following two groups: Each group grows and spreads in different way. For example, SCLC spreads aggressively and responds best to chemotherapy and radiation therapy. It occurs almost exclusively in smokers and accounts for over 20% of all lung cancers in the United States. NSCLC is more common and accounts for about 80% of all lung cancers in America. When confined to a small area and identified early, this type of cancer often can be removed surgically. Table 26-1 provides general characteristics of these cancer cell types, including growth rates, metastasis, and means of diagnosis. A more in-depth description of each cancer cell type follows. Table 26-1 Characteristics of Lung Cancers Modified from McCance KL, Huether SE: Pathophysiology: the biologic basis for disease in adults and children, ed 5, St Louis, 2006, Mosby. The tumor has a slow growth rate and a late metastatic tendency (mostly to hilar lymph nodes). These tumors generally remain fairly well localized and tend not to metastasize until late in the course of the lung cancer. Cavitation and necrosis within the center of the cancer is a common finding. Surgical resection is the preferred treatment if metastasis has not taken place. In about one third of the cases, squamous cell carcinoma originates in the periphery. Because of the location in the central bronchi, obstructive manifestations are generally nonspecific and include a nonproductive cough and hemoptysis. Pneumonia and atelectasis are often secondary complications of squamous cell carcinoma. Cavity formation with or without an air-fluid interface is seen in 10% to 20% of the cases (see Figure 26-1, A). Adenocarcinoma arises from the mucous glands of the tracheobronchial tree. In fact, the glandular configuration and the mucous production caused by this type of cancer are the pathologic features that distinguish adenocarcinoma from the other types of bronchogenic carcinoma. It accounts for 35% to 40% of all bronchogenic carcinomas. Adenocarcinoma has the weakest association with smoking. However, among people who have never smoked, adenocarcinoma is the most common form of lung cancer. Adenocarcinoma tumors are usually smaller than 4 cm and are most commonly found in the peripheral regions of the lung parenchyma. The growth rate is moderate and the metastatic tendency is early. Secondary cavity formation and pleural effusion are common (see Figure 26-1, B). When the cancer is discovered early, surgical resection is possible in a high percentage of cases. Large cell carcinoma accounts for about 10% to 15% of all bronchogenic carcinoma cases. Because this tumor has lost all evidence of differentiation, it is commonly referred to as undifferentiated large cell anaplastic cancer. Although these tumors commonly arise peripherally, they may also be found centrally—often distorting the trachea and large airways. Large cell carcinoma has a rapid growth rate and early and widespread metastasis. Common secondary complications include chest wall pain, pleural effusion, pneumonia, hemoptysis, and cavity formation (see Figure 26-1, C). Small cell carcinoma accounts for about 14% of all bronchogenic carcinomas. Most of these tumors arise centrally near the hilar region. They tend to arise in the larger airways (primary and secondary bronchi). Cell size ranges from 6 to 8 µm. The tumor grows very rapidly, becoming quite large, and metastasizes early. Because the tumor cells often are compressed into an oval shape, this form of cancer is commonly referred to as oat cell carcinoma. Staging for small cell carcinoma is divided into only two categories: limited disease (20% to 30%) or extensive disease (70% to 80%). Small cell carcinoma has the poorest prognosis. The average survival time for untreated small cell carcinoma is about 1 to 3 months. Small cell carcinoma has the strongest correlation with cigarette smoking and is associated with the worst prognosis (see Figure 26-1, A). A routine chest x-ray is the most common screening test used to identify an abnormal mass or nodule in a patient’s lung. Computed tomography (CT) and positron emission tomography (PET) scans are also frequently used to reveal extremely small lesions and determine whether the cancer has spread to other areas. A definitive diagnosis, however, can be made only by viewing a tissue sample (biopsy) under a microscope. Common procedures used to obtain a tissue biopsy include bronchoscopy, thoracoscopy, mediastinoscopy, transbronchial needle biopsy or open-lung biopsy, sputum cytology, thoracentesis, and videothoracoscopy (see Chapter 8). Staging is the process of classifying information about cancer. The staging system describes the cancer cell type, the size of the tumor, the level of lymph node involvement, and the extent to which the cancer has spread. The patient’s prognosis and treatment depend, to a large extent, on the staging results. The system most often used for the staging of lung cancer is the TNM classification (Table 26-2). T represents the extent of the primary tumor, N denotes the lymph node involvement, and M indicates the extent of metastasis. On the basis of the TNM findings, roman numerals are used to identify stages I through IV, with 0 being the least advanced and IV the most advanced. Figure 26-2 provides five representative illustrations of the staging of lung cancer by the TNM classification system. A general overview and description of the staging process for non–small cell lung cancer and small cell lung cancer follows*: Table 26-2 1997 Revised International System for Staging Lung Cancer
Cancer of the Lung
Anatomic Alterations of the Lungs
Etiology and Epidemiology
Types of Cancers
Tumor Type
Growth Rate
Metastasis
Means of Diagnosis
Squamous cell carcinoma
Slow
Late; mostly to hilar lymph nodes
Biopsy, sputum analysis, bronchoscopy, electron microscopy, immunohistochemistry
Adenocarcinoma
Moderate
Early
Radiography, fiberoptic bronchoscopy, electron microscopy
Large cell carcinoma
Rapid
Early and widespread
Sputum analysis, bronchoscopy, electron microscopy (by exclusion of other cell types)
Small cell (oat cell) carcinoma
Very rapid
Very early; to mediastinum or distally in lung
Radiography, sputum analysis, bronchoscopy, electron microscopy, immunohistochemistry, and clinical manifestations (cough, chest pain, dyspnea, hemoptysis, localized wheezing)
Non–Small Cell Lung Carcinoma
Squamous cell carcinoma
Adenocarcinoma
Large cell carcinoma (undifferentiated)
Small Cell Lung Carcinoma
Screening and Diagnosis
Staging of Lung Cancer
Symbol
Definition
Primary Tumor (T)
T0
No evidence of tumor
Tx
Tumor that cannot be assessed or is not apparently radiologically or bronchoscopically (malignant cells in bronchopulmonary secretions)
Tis
Carcinoma in situ
T1
Tumor with the following characteristics:
a
Size: ≤3 cm
b
Airway location: in lobar bronchus or distal airways
c
Local invasion: none, surrounded by lung or visceral pleura
T2
Tumor with any of the following characteristics:
a
Size: >3 cm
b
Airway location: tumor in the main bronchus (within 2 cm of the carina) or tumor with atelectasis involvement of the main bronchus (distance to the carina is 2 cm or more) or presence of atelectasis or obstructive pneumonitis that extends to hilar region but does not involve the entire lung
c
Local invasion: involvement of the visceral pleura
T3
Tumor with the following location or invasion:
a
Size: any
b
Airway location: tumor in the main bronchus (within 2 cm of the carina) or tumor with atelectasis or obstructive pneumonitis of the entire lung
c
Local invasion: invasion of chest wall (including superior sulcus tumors), diaphragm,mediastinal pleura, or parietal pericardium
T4
Tumor with the following location or invasion:
a
Size: any
b
Airway location: satellite tumor nodule(s) within the ipsilateral primary-tumor lobe of the lung
c
Local invasion: invasion of the mediastinum, heart, great vessels, trachea, esophagus, vertebral body, or carina; or presence of malignant pleural/pericardial effusion
Lymph Nodes (N)
Nx
Regional lymph nodes cannot be assessed
N0
Absence of regional lymph node involvement
N1
Presence of metastasis to ipsilateral peribronchial or ipsilateral hilar lymph nodes or both (including direct extension to intrapulmonary nodes)
N2
Presence of metastasis to ipsilateral mediastinal or subcarinal lymph nodes or both
N3
Presence of metastasis to any of the following lymph node groups: contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular
Distant Metastasis (M)
Mx
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access