Bypass Graft Angiography
Kellan E. Ashley
Selective angiography of saphenous vein and arterial bypass grafts is usually performed immediately after angiography of the native coronary arteries. The technique for bypass graft opacification is similar to that employed for native coronary artery angiography. Knowledge of common graft locations and familiarity with multiple catheter types are essential to perform a complete study.
Saphenous Vein Grafts
Saphenous veins are the most commonly employed conduits in coronary revascularization. Approximately 87% of saphenous vein grafts (SVGs) remain patent at 6 months, with the patency rates dropping to approximately 63% at 10 years. Because of the high incidence of graft attrition, repeat revascularization often becomes necessary, requiring coronary angiography to assess graft patency.
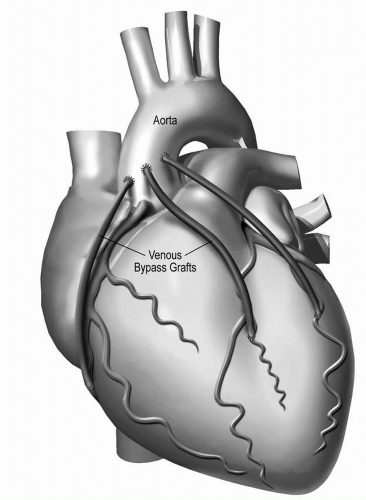
The proximal anastomosis of most aortocoronary SVGs lies on the anterior surface of the aorta, several centimeters above the sinuses of Valsalva. Usually, the location of the various grafts in relation to one another follows a predictable sequence. Grafts to the left circumflex coronary artery (LCX) are typically placed most superior, followed in succession inferiorly by grafts to the diagonal branches of the left anterior descending artery (LAD), the LAD itself, and the right coronary artery (RCA) (Figure 4-1). It should be noted, however, that because of variations in surgical technique, exceptions to this rule commonly exist. If prior angiograms are available, they should be reviewed firsthand prior to diagnostic angiography, as these can be extremely helpful in locating graft ostia and for selection of catheters.
The Judkins right 4 (JR4) catheter is the most common catheter employed in pursuit of vein grafts. Typically, grafts to the RCA can be best visualized and cannulated while in the left anterior oblique (LAO) projection, while grafts to the left coronary artery (LCA)
system are most easily found while in the right anterior oblique (RAO) projection (Table 4-1). The proximal anastomosis sites of these grafts lie superior to the native coronary ostia. Some surgeons place ostial graft markers on the outer surface of the aorta at the time of surgery to facilitate location of the grafts during future catheterizations. Surgical clips may also provide clues as to the location of grafts.
system are most easily found while in the right anterior oblique (RAO) projection (Table 4-1). The proximal anastomosis sites of these grafts lie superior to the native coronary ostia. Some surgeons place ostial graft markers on the outer surface of the aorta at the time of surgery to facilitate location of the grafts during future catheterizations. Surgical clips may also provide clues as to the location of grafts.
Table 4-1 General Graft Views | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Steady “up and down” movements of the catheter in the ascending aorta with slight clockwise or counterclockwise rotations, typically from the second to the fourth sternal sutures, facilitate engagement of the various grafts. The catheter tip often “jumps” forward when it cannulates a graft ostium. Damping of the pressure waveform may indicate that the catheter tip is lying against the vessel wall or that there is an ostial stenosis. In this situation, the catheter should be cautiously withdrawn while simultaneously reversing its torque. Occasionally, the pressure waveform remains damped, and it may be necessary to perform a ramped injection of contrast with quick removal of the catheter in order to rule out critical stenosis or subtotal obstruction of a graft. Remember that injecting through a deep-seated catheter may not define an ostial stenosis. Occluded grafts will appear as a “stump” upon selective injection.
If a graft cannot be cannulated, do not assume that the graft is occluded. Other catheters with different angulation may be necessary. If further attempts fail, aortography via a pigtail catheter may be helpful in locating difficult-to-find grafts. To locate bypass grafts to the left coronary system, an aortogram in LAO projection is recommended. Conversely, for RCA grafts, an RAO projection should be adequate.
A careful review of native coronary angiograms may also provide clues regarding graft patency. For instance, if a bypassed native artery demonstrates competitive distal flow, the graft supplying that artery is likely patent. Conversely, if normal distal flow is seen in the bypassed native artery, without competitive filling, the graft is probably occluded.
Once properly engaged, each graft should be visualized in both the LAO and RAO projections using an injection technique similar to that employed for native coronaries. Usually, several views are needed to fully assess the graft ostium, body, and distal anastomosis. Additionally, the individual views that are best for evaluating each native coronary artery can be helpful in evaluating the distal anastomosis of the graft as well as the distal course of the native vessel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree