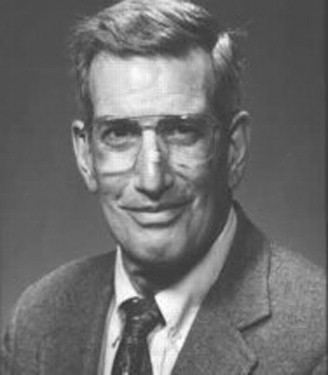
From Eugene Braunwald, MD
I first met Burt in July 1964 when he joined the intramural program of the National Heart Institute (now the NHLBI) as a Clinical Associate. He spent four months as a clinical fellow on the Clinical Cardiology Service which I headed at the time, and I rounded with him daily. Not surprisingly, he had an enormous knowledge base (after all, he was a magna cum laude graduate of Harvard Medical School and had two years of medical house staff training at the (then) Peter Bent Brigham Hospital). But, more important, he showed great clinical intuition—that special sixth sense about patients—which would make him not merely a great, but a truly outstanding clinician.
In addition to their clinical rotations, Clinical Associates could choose a laboratory for their research. Although I tried to persuade Burt to join my laboratory, in which we were studying myocardial function, both in isolated cardiac muscle as well as in patients, he made a pivotal and correct decision by declining my invitation politely in order to work in the Experimental Pharmacology section, where he could immerse himself in and be taught cardiac biochemistry by experts.
After completing his two year stint at the NIH, which satisfied his Selective Service obligations, Burt returned to the Brigham for his senior medical residency. His training in biochemistry made him even more attractive to me and I urged, cajoled and pressured him to return to Bethesda and set up a biochemistry laboratory in Cardiology. He did so with rapidity and efficiency and first authored a widely-quoted paper on mitochondrial function in experimental heart failure.
When I moved to UCSD as chair of medicine in 1968, I got my “claws” into Burt and convinced him and Susan and several other colleagues to leave the security of the NIH and join me in the adventure of helping to start a new medical school in the desert of southern California. Like a cactus, Burt bloomed in the desert. We worked together on attempting to reduce infarct size in dogs. His role in those early experiments was critical. He set up from scratch both a research laboratory to measure creatine kinase concentration in heart muscle of rabbits with myocardial infarction and simultaneously a new Coronary Care Unit.
What I recall most vividly from that period are Burt’s qualities as a physician. We did not have the luxury of having top notch residents or cardiology fellows during the earliest years and whenever a critically ill patient came into his unit, without being asked and without fanfare, Burt stayed in the unit all night and did what could be done for the patient. This was a great morale booster to the faculty, nurses, medical students, and set a standard for all of our trainees. Burt’s mood was always upbeat. He was an inveterate optimist and radiated enthusiasm.
Then after eight wonderful years together in Bethesda and La Jolla, Burt and I went our separate ways—he to St. Louis and then to Burlington, Vermont, and I to Boston, but the bond between us remained unbroken. He went on to play a seminal role in the development of fibrinolytic therapy for acute myocardial infarction and in the development of measurements of infarct size in patients.
The impact of his research was enormous, but his impact on people was, if anything, even greater. He moved effortlessly from being a trainee to an independent scientist, to a gifted mentor, to a truly great academic leader, and ultimately a senior statesman in cardiology. We have lost one of the great leaders of our field.
Eugene Braunwald, MD
Distinguished Hersey Professor of Medicine, Harvard Medical School
Founding Chairman, TIMI Study Group, Brigham and Women’s Hospital, Boston, Massachusetts
E-mail address: ebraunwald@partners.org
From Lawrence S. Cohen, MD
When I first met Burt Sobel his family and friends called him Buddy and that is who he was to us for 50 years. Others will chronicle Buddy’s scientific achievements, which were monumental. I will not repeat them but they have left an indelible mark on the progress of cardiology in the late 20 th century.
The time is July, 1962. Buddy was an intern in medicine at the Peter Bent Brigham Hospital (now the Brigham and Women’s Hospital) in Boston. I was a fellow in cardiology at that same institution. I received a call one morning while I was in the cardiac catheterization laboratory. The call was about a patient who this young intern felt needed an urgent cardiac catheterization. He was correct. The intern was Buddy Sobel. We met over the patient’s bedside a short time later.
I came home that night for dinner and indicated to my wife, Jane, that I had met a very personable, bright young intern that day, Buddy Sobel. She said she had met an equally attractive young woman at the supermarket that afternoon who had asked about the calorie count for a container of yoghurt. Her name was Susan Sobel. Could they be a couple? They were. The four of us spent a close two years together in Boston which formed the foundation for a half century friendship.
We learned, as young marrieds, that turkeys need to be defrosted before they were put in the oven for Thanksgiving dinner. We watched Susan develop as a modern dancer. While Buddy introduced us to Tolkien and the Once and Future King, Susan was devouring Henry James during her pregnancy. Our daughter was born several months before Jonathan, but his was a more dramatic arrival. Buddy was on service when Susan came in with a placenta previa.
Buddy and I next interacted in 1965, when we were at the National Heart Institute, he as a Clinical Associate and I on the staff as head of the clinical program for the Cardiology Branch. Both of us were under the leadership of Gene Braunwald. Early that summer, we received a call that a prominent researcher at the Heart Institute was being brought in with what sounded like a heart attack. Indeed, it was. His electrocardiogram had all of the characteristics of an acute heart attack involving primarily the right ventricle. His blood pressure was 90/60 mm Hg. The first article describing the proper therapy for patients with right ventricular infarction had yet to be published. The proper therapy is now quite basic and is part of Cardiology 101. In a patient with a right ventricular infarct the proper therapy is to give a large intravenous volume of fluid. The wrong therapy is to give medications aimed solely at raising the blood pressure. On that warm summer day Cohen and Sobel gave only small amounts of intravenous fluid and gave an abundant quantity of adrenalin-like drugs to raise his blood pressure. I am happy to tell you that the researcher survived, perhaps in spite of our ministrations, not because of our ministrations. He lived for another productive twenty years.
After Buddy moved to San Diego and then to Barnes, we saw each other at heart meetings where he shared his pride in the achievements of Jonathan and Elizabeth as they grew, and in Susan’s success as a family therapist. His favorite meetings were those at which he could find a piano or a ski slope, because his love of music and passion for skiing, almost matched his love of medicine. I wish I could say that the brilliance he demonstrated in the laboratory, in the clinic, and on the podium was also apparent in his early choice of clothes, but by the time Buddy was at the peak of his profession; his taste had markedly improved, prodded by my wife Jane.
Buddy’s sense of humor was acute and nowhere was it needed more than in 1979 when five cardiologists were on a three-week scientific interchange in China. At the time of our visit, hostages from our Iranian embassy were being held in Tehran. We found ourselves stranded in Xian due to a windstorm from Mongolia which we were told, prevented planes from returning to Beijing. In the military barracks, five men had only the clothes on their backs and one book that Buddy had brought with him. He dismembered the book so that we could each have chapters to occupy ourselves and he somehow got word back to Susan that we were not in need of ransoming as yet. Buddy kept one of the physicians from becoming unglued at the thought of not being able to get back in time for an important meeting; and prevented panic from setting in when we saw only Iran airliners on the tarmac when we finally landed in Beijing.
Liz Sobel provided another point of contact for Buddy and me. Coincidentally, she and our older daughter happened to be on the same bike trip as teenagers and recognized the names they had heard throughout their childhoods. The two became friends. Then, Liz attended Wesleyan which is 45 minutes from where we live. Once again, we were able to spend Thanksgiving with the Sobels’ and get to meet Don when he and Liz began dating.
In his later years, when he was in Vermont, Buddy continued to send me books. The Art of War by Sun Tzu and the End of Faith by Sam Harris were two of his favorites. He gave us updates on Jonathan’s legal career which has been as stellar as Buddy’s own in medicine. He learned about the intricacies of advertising and the wine industry as he kept pace with Liz and Don’s lives. He embraced his daughter-in-law and grandparenthood. He marveled at Susan’s ability to rehab after painful knee surgery and attack the slopes with her usual vigor.
When Buddy developed cancer, he researched his disease with the same probing intellect that he brought to Cardiology. His love of his family, his passion for his work, his devotion to his colleagues and friends, his optimism and his humor remained undiminished. It is we who feel diminished by his loss.
Buddy, we will always miss you.
Lawrence S. Cohen, MD
The Ebenezer K Hunt Professor of Medicine (Emeritus), Yale University School of Medicine, New Haven, Connecticut
E-mail address: lawrence.s.cohen@yale.edu
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


