Buerger’s Disease
PARTHY SHAH and SANJAY RAJAGOPALAN
Presentation
A 43-year-old man who is an assembly line worker presents with pain and discoloration in all four extremities. He previously noted a discolored area in the tip of his right fourth and fifth fingers approximately a month ago. He also previously noted pain in his feet bilaterally with exertion that seems to have worsened over the last several weeks with cessation with rest. He has not been able to work the last 2 weeks owing to these symptoms. On further questioning, he notes increasing cold intolerance in his upper and lower extremities over the last 2 years, which he attributes to his age. Past medical history is unremarkable for prior medical illness or rheumatologic disease. He smoked two to three packs of cigarettes a day for the past 25 years and cannot quit. His medications currently include Tylenol with codeine. There is no history of migraine medication or ergot-type derivative use. Although he has worked as an assembly line worker, his job does not include exposure to vibratory tools. There is no family history of premature atherosclerotic vascular disease or death. On physical examination, the patient is afebrile with normal blood pressures in the upper extremities. Examination of the right upper extremities reveals a healed ulcer measuring 2 mm on the tip of the right fourth digit. Radial pulses are normal. Allen’s test reveals severe blanching of the right hand on occlusion of the ulnar artery, suggesting occlusion of the radial artery at the wrist. No Osler nodes or Janeway lesions are noted. Examination of the lower extremities reveals normal femoral, popliteal, and dorsalis pedis pulses but an absent posterior tibial artery pulse on the left lower extremity. Cardiac examination is normal, with no murmurs or rubs on auscultation. No bruits are appreciated.
Differential Diagnosis
The presentation is one of an individual with advanced signs of ischemia in his lower and upper extremities and Raynaud’s symptoms. These symptoms are concerning for small vessel disease involvement in both upper and lower extremities and are therefore suggestive of a systemic process. The presence of a healing ulcer in the upper extremity (evidence of tissue loss) rules out primary Raynaud’s syndrome. The differential diagnosis includes diseases that involve small and medium vessels of both the upper and lower extremities. Consideration should also be given to infectious etiologies (e.g., infective endocarditis) or intracardiac sources of embolism. Table 1 lists potential considerations.
TABLE 1. Etiologic Considerations
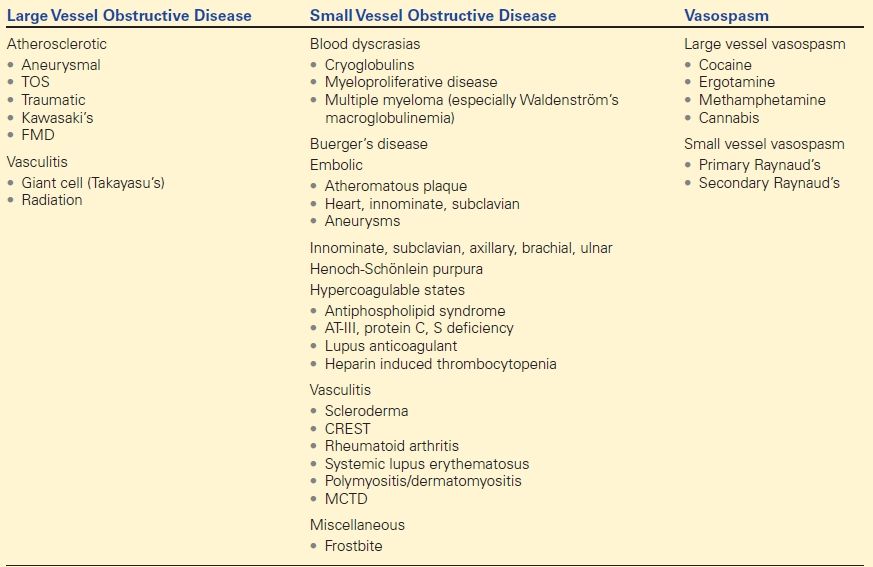
AT-III, anti-thrombin III; CREST, calcinosis, Raynaud’s phenomenon, esophageal involvement, sclerodactyly, telangiectasia (syndrome); FMD, fibromuscular dysplasia; MCTD, mixed connective tissue disease; TOS, thoracic outlet syndrome.
Workup
A complete evaluation is ordered, including laboratory studies as outlined in Table 2 and Figure 1.
TABLE 2. Laboratory Testing in Patients with Suspected Small Vessel Disease
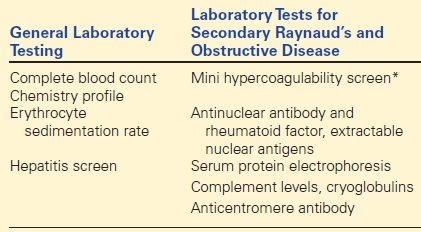
* Mini hypercoagulability screen includes antiphospholipid antibodies, lupus anticoagulant, antithrombin III, protein C (activity) and protein S levels, factor V Leiden, and prothrombin gene mutation.
For large artery obstruction, one may consider performing this workup in addition, when appropriate.
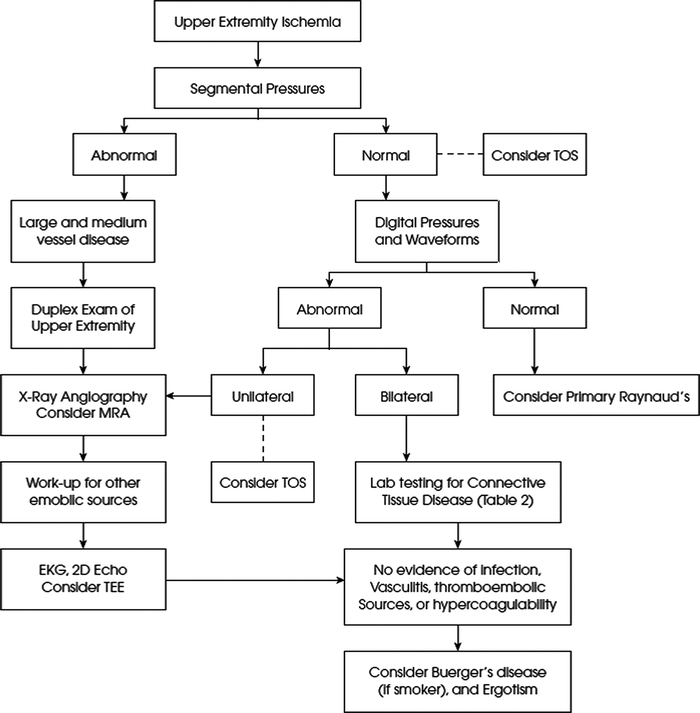
FIGURE 1 Upper extremity ischemia algorithm.
Evaluation Report
Complete blood counts, total cholesterol, lipid profile, and homocysteine levels are normal. A workup for collagen vascular disease and hypercoagulability (including antiphospholipid antibodies, antithrombin III, protein C, and protein S activities) are normal. Erythrocyte sedimentation rate (ESR) is 15 mm/h, and the level of C-reactive protein (CRP) is low.
A transthoracic echocardiogram followed by a transesophageal echocardiogram does not reveal a cardiac or aortic (ascending arch and portion of descending) source.
Segmental pressures in the upper extremity reveal symmetric diminution in pressures at the level of the fingers with a decrease in pressures in most fingers of both upper extremities (40 mm in the right fourth and fifth digits), with damped waveforms in these digits. normal finger pressures should be greater than 80 mm Hg.
Upper extremity duplex testing reveals patent brachial and axillary arteries without evidence of aneurysm or occlusion.
An ankle-brachial index (ABI) and segmental pressures of the lower extremity revealed an index of 0.9 in the right and 0.9 in the left. Toe brachial indices were 0.3 bilaterally with monophasic waveforms in all digits of the feet.
Recommendations
A three-dimensional contrast-enhanced magnetic resonance arteriography (MRA) is ordered of the abdomen and lower extremities to rule out concomitant large vessel disease in the pelvis and thighs. MRA of the lower extremities did not reveal large vessel occlusive disease (iliac and femoral arteries were patent bilaterally). However, it did reveal occlusion of the left posterior tibial artery bilaterally at its origin with reconstitution at both ankles by collaterals. Disease of the tibioperoneal system was noted bilaterally with incomplete visualization of the pedal vessels bilaterally. The pedal vessels were poorly visualized bilaterally.
Diagnosis
This man has systemic disease that selectively affects small and medium vessels of the upper and lower extremities. The patient also has symptoms suggestive of Raynaud’s syndrome. The major etiologies to consider in this case are related to infectious, embolic, and vasculitic causes, and Buerger’s disease. Specific aspects of this case that are of interest and enable one to arrive at the diagnosis are as follows. Unilateral versus bilateral symptoms: Bilaterality of symptoms and signs (asymptomatic involvement of digits) suggests a systemic process. Tissue necrosis in the upper extremity excludes primary Raynaud’s, which is intermittent and shows complete resolution in between attacks. Moreover, the lower extremity symptoms in this case are suggestive of a systemic diagnosis. Digital ulcerations are most commonly caused by vasculitis (50% to 75% of all cases); half of the vasculitis cases are caused by primary Sjögren’s syndrome (PSS); the syndrome of calcinosis, Raynaud’s phenomenon, esophageal involvement, sclerodactyly, and telangiectasia (CREST); Buerger’s; and complications of atherosclerosis (e.g., embolism). The presence of foot claudication suggests small vessel involvement often seen in Buerger’s disease. However, foot claudication is by no means specific for Buerger’s disease (it may also be seen with thromboembolization). Smoking history is almost invariably present, and the absence of smoking should render the diagnosis of Buerger’s disease suspect.
Discussion
Buerger’s disease (thromboangiitis obliterans) is a nonatherosclerotic segmental peripheral arterial disease primarily affecting small- and medium-sized vessels of the arms and legs. It is strongly associated with current or recent tobacco use and appears to be more common in countries with heavier tobacco use. The disease has a male predominance with an onset before age 45 to 50 years. Affected patients often first notice dysesthesias, Raynaud’s phenomenon, and pedal claudication. Ischemic rest pain, ulceration, superficial migratory thrombophlebitis, and digital gangrene are characteristics of disease progression. Multiple limbs are nearly always involved, even in cases where clinical signs and symptoms exist in a single limb. Hence, an Allen test may be positive even in the setting of only lower extremity pain and ulceration.
Diagnosis is by exclusion, as detailed above. Commonly measured markers for inflammatory disease (ESR, CRP) and autoantibodies (antinuclear antibody, rheumatoid factor) are usually normal or negative. Proximal sources of emboli should be considered as part of the differential diagnosis and may be evaluated by transthoracic or transesophageal echocardiogram, depending on clinical suspicion. Arteriography typically shows segmental occlusive lesions of distal vessels surrounded by “corkscrew” or “tree-root” collateral vessels in the absence of atherosclerosis (Fig. 2). These findings are suggestive but not pathognomonic. An excisional biopsy is rarely needed but can be obtained from amputations or acute superficial phlebitis for confirmation of the diagnosis. Histopathologic analysis of an acute phase lesion may demonstrate the classic findings of inflammatory cellular thrombi, with relative sparing of the vessel wall and preservation of the internal elastic lamina. Chronic lesions are characterized by organized thrombus and fibrosis.
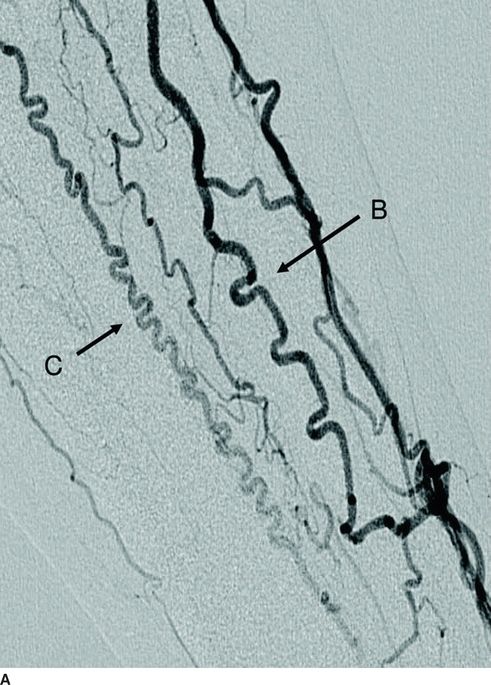
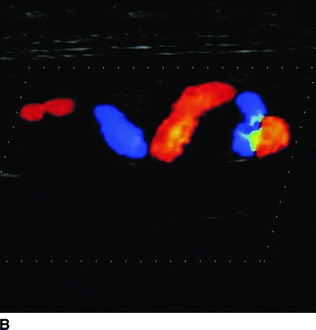
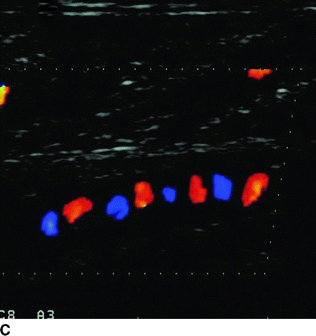
FIGURE 2 A: Digital subtraction angiography shows corkscrew collaterals around the area of occlusions in the right lower leg. Continuous-wave Doppler ultrasound shows corkscrew collaterals as color Doppler flows of a snake sign (A [arrow B] and B) and a dot sign (A [arrow C] and C). (From Fujii Y, Nishioka K, Yoshizumi M, et al. Corkscrew collaterals in thromboangiitis obliterans (Buerger disease). Circulation. 2007;116:e539–e540, with permission.)



