Chapter 6 Bronchoscopic Treatment of Idiopathic Laryngotracheal Stenosis with Glottis Involvement
Case Description
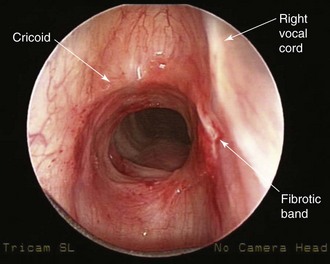
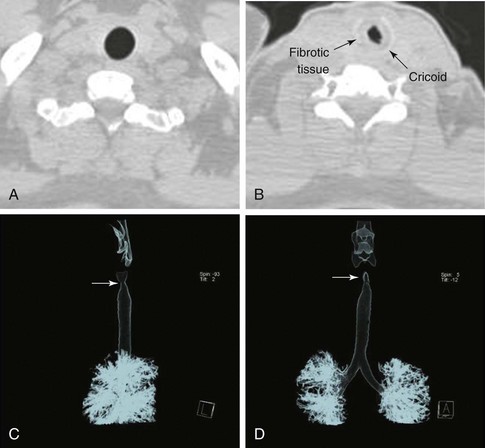
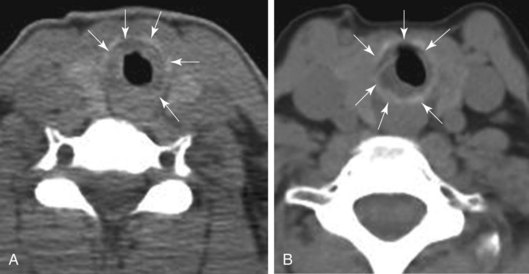
The patient is a 29-year-old woman who had developed mild hoarseness and progressive shortness of breath with exertion. These symptoms interfered with her life to the point that she had to stop working as a teacher because of impaired phonation. Intermittent sensations of nocturnal suffocation improved after coughing up thick mucus. She had no history, clinical signs, or symptoms of connective tissue disorders, and no history of endotracheal intubation. Other findings included asymptomatic mild mitral valve prolapse diagnosed after a routine cardiac examination revealed a 2/6 systolic ejection murmur. The patient had type 2 diabetes mellitus, which was well controlled with metformin. Her physical examination was unremarkable except for a mouth opening of 2 fingerbreadths. After 6 months of unsuccessful antiasthma treatment, a flexible bronchoscopy had revealed a circumferential subglottic stenosis extending for 1 cm with associated inflamed hyperemic mucosa (Figure 6-1). A fibrotic band extended to but did not involve the right vocal cord. The degree of airway narrowing was calculated at 60% on computed tomography and morphometric bronchoscopic analysis (Figure 6-2). No posterior glottis stenosis or cicatricial fusion of the vocal cords was noted.
Discussion Points
1. Mention two demonstrably accurate methods for assessing functional impairment in this patient.
2. Describe how the extent of laryngotracheal stenosis (LTS) affects whether this patient should be referred for surgical intervention.
3. Describe existing evidence for using adjuvant therapies to potentially decrease the rate of recurrence of this type of stricture.
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
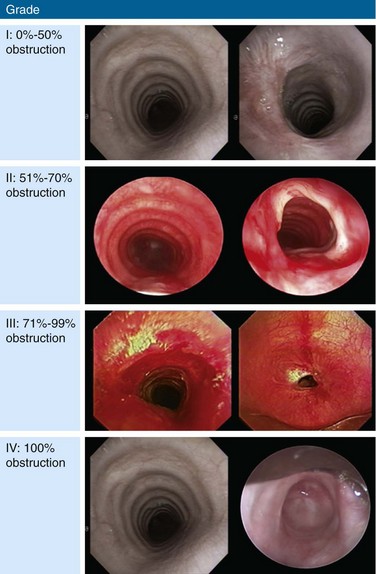
The clinical presentation of this patient is classic for idiopathic laryngotracheal stenosis (LTS). Most patients who suffer from this disease are females in their third, fourth, or fifth decade. Currently, it is not clear why idiopathic LTS is restricted to females, but estrogen and progesterone receptor studies in resected surgical specimens showed positive staining of fibroblasts, suggesting a hormonal role in pathogenesis.1 Many patients will have been misdiagnosed with asthma for months to years before an LTS is discovered. The duration of symptoms in one study was less than 2 years in 28% of patients, 2 to 10 years in 61% of patients, and longer than 10 years in 11% of patients.1 Symptoms at rest in LTS usually are not present until a 70% reduction in tracheal lumen diameter is attained, and stridor, at rest, can be noticed only when the tracheal lumen becomes smaller than 5 mm in diameter.2 Effort intolerance caused by exertional dyspnea is the primary cause of morbidity and early disability in LTS. Its presence in this patient is consistent with moderate stenosis using a bronchoscopic classification, signaled by 50% to 70% airway lumen narrowing.3–5 Under the Myer-Cotton System* for LTS, she would be classified as having a grade II lesion, because her stenotic index (SI)† was 60% (Figure 6-3).6 The patient’s functional status, which probably should be part of a multidimensional evaluation of LTS, can be objectively measured using, for example, the Medical Research Council (MRC) dyspnea scale, which has been shown to be sensitive to the presence of varying degrees of LTS.7
Bronchoscopy, in addition to contributing to an assessment of the severity of airway narrowing, allows precise determination of the extent (craniocaudal length) and location of the stenosis. According to the McCaffrey system,* the patient’s stricture, with extension to the glottis, was stage IV. This system is based on the site and extent of an airway stenosis. Four stages are thus defined: I: lesions confined to the subglottis or trachea that are less than 1 cm in length; II: subglottic stenoses longer than 1 cm within the cricoid and not extending to the glottis or trachea; III: subglottic stenoses that extend into the upper trachea but do not involve the glottis; and IV: lesions involving the glottis. Almost 20% of patients with LTS have combined subglottic and glottis stenosis.8
Comorbidities
Other than having diabetes and mitral valve prolapse without significant mitral regurgitation, confirmed by echocardiography, our patient was healthy. Diabetes is known to impair microcirculation with resultant deleterious effects on wound healing. Diabetes was found to be an important risk factor for anastomotic complications (odds ratio of 3) in patients who undergo laryngotracheoplasty or cricotracheal resection.9 This may be a consequence of impairment of an already compromised collateral circulation at the end of the divided airway. Tension at the anastomosis further increases risk.
Support System
The patient was married to a very supportive husband; her knowledge of the diagnosis was minimal. In addition to receiving information from us during the initial encounter, she was advised to search for support groups, chat rooms, and reliable Internet websites for patients suffering from the same disorder.10,11
Patient Preferences and Expectations
Although the patient was asymptomatic at rest, her disease interfered with her ability to work, exercise, and enjoy outdoor activities. She wanted to have a child and was worried that pregnancy could worsen her symptoms and compromise both her and her baby’s health. She was informed of available therapeutic options for LTS, including flexible or rigid bronchoscopic dilation, laser-assisted mechanical dilation (LAMD), surgery, and even tracheostomy. Because tracheostomy would further compromise her quality of life, this was considered only as a last resort in case of disease progression. She was terrified about the possibility of losing her voice, which would preclude her from working as a teacher. After her symptoms, personal values, and expectations were considered, the likelihood of complications resulting from open surgical resection was believed to outweigh the benefits, in part because of her very high stenosis extending to the glottis, diabetes, and the possibility of dysphonia postsurgical interventions.9 Rigid bronchoscopy with dilation and laser resection under general anesthesia, therefore, appeared to be a reasonable initial therapeutic alternative.
Procedural Strategies
Indications
This patient’s stricture was considered idiopathic because no history of intubation, autoimmune disease, relapsing polychondritis, radiation, trauma, or prior surgery was elicited; therefore, systemic medical therapy with immunosuppressive drugs had no role. A bronchoscopic procedure or open surgery could restore satisfactory airway lumen patency and improve symptoms.4,9
Her active lifestyle caused routinely high flow velocity through her moderately stenotic airway. Improving airway patency to less than 50% narrowing could alleviate her exertional dyspnea.12 In a large series of idiopathic strictures, the point of maximal stenosis was found to be almost always located in the region extending from the upper edge of the cricoid to the lower edge of the first tracheal ring.13 Our patient’s stricture was only 1 cm in length. From a flow dynamics standpoint, longer stenoses (>1 cm) show only a small difference in pressure profiles, with a slightly smaller magnitude of total pressure drop across the stricture and shorter (<1 cm) strictures of comparable diameter.12 Strictures up to 1 cm long are considered of mild extent and, if uncomplicated by malacia, appear to respond well to bronchoscopic laser-assisted dilation. On the other hand, operable patients with longer strictures and patients with associated malacia may be better managed with open surgical interventions.8
The morphology of the stricture, however, was circumferential. Results from studies show that patients with circumferential stenosis require a second endoscopic intervention more often than those with purely eccentric localized hypertrophic tissue (75% vs. 43%) (Figure 6-4). This would support referral for primary surgical resection.14,15 Risks of surgical resection and reanastomosis, however, must be carefully weighed because of the fibrotic band extending to the right vocal cord and the patient’s fear of voice alteration. An incomplete surgical resection could leave behind residual fibrotic tissue, leading to restenosis.16 In addition to the length of the resection, the fixed morphology of the stricture plays an important role in anastomotic tension: Fibrous retracting strictures (i.e., circumferential and hourglass strictures) are very different from dynamic, malacic stenoses (pseudoglottic, triangular stomal strictures); in the former, the healthy trachea is already tractioned, whereas in the latter, it is the normal elasticity of the trachea that tends to worsen the stenosis. Just because stenoses are of the same length, therefore, does not mean that traction across the suture line after surgical resections is the same.9 Taking into account the circumferential and fixed morphology, its extension to the glottis, the patient’s preferences, and her diabetes, we chose to proceed initially with a rigid bronchoscopic intervention.
Expected Results
Our patient’s 1 cm, fixed, circumferential stenosis with hypertrophic fibrotic tissue could initially respond to laser-assisted dilation with an increase in airway cross-sectional area. In patients with idiopathic LTS, however, the therapeutic success of rigid bronchoscopic interventions is variable. Factors impacting success include stenoses that (1) were not completely circumferential (eccentric) (see Figure 6-4), (2) measured less than 1.0 cm in the vertical extent, and (3) were not associated with significant loss of cartilage or remodeling.14 In a retrospective analysis of 16 patients with mean follow-up time of 75.5 months, 14 patients required treatment: 9 patients were controlled effectively using endoscopic laser techniques; endoscopic management failed, however, in 5 patients (noted to have stenosis thicker than 1 cm).17
In a larger study of 30 patients, endoscopic treatment by CO2 (in 4 patients) or neodymium-doped yttrium aluminum garnet (Nd : YAG) laser–assisted dilation (in 26 patients) without or with temporary airway stent insertion (in 4 patients) was considered to be the treatment of choice for initial management of idiopathic LTS. After repeated endoscopic failures (mean, 6.2), open neck surgery by laryngotracheoplasty or reconstruction and anastomosis was performed in 17% of patients, particularly for lesions longer than 1 cm.18 In another series, all patients were treated bronchoscopically. Sixty percent required a second procedure, with a mean interval between procedures of 9 months, and no need for tracheotomy or open surgical intervention was reported.15 Similar results have been reported in several nonrandomized studies of bronchoscopic management.18–20
Team Experience
Laser-tissue interactions are based on biologic, photochemical, or thermal reactions. The treating team’s knowledge of tissue effects in specific settings is important because choosing the wrong laser (e.g., using the Nd : YAG laser to cut or the potassium-titanyl-phosphate [KTP] laser to coagulate) or inappropriate laser settings or resection techniques (e.g., inappropriate use of power density*) in the subglottic area can enhance laser-related adverse effects. Laser-related adverse effects might alter local anatomy. We suggest, therefore, that patients with idiopathic LTS should be managed within the context of a multidisciplinary airway disease program, or, at the least, that their condition should be discussed with surgical colleagues whenever possible before bronchoscopic treatments are initiated.
Risk-Benefit Analysis
A stricture in the subglottic larynx† poses a challenge because of its proximity to the vocal cords, and because this region is the narrowest segment of the airway. Although no prospective randomized studies are available from which to draw conclusions with regard to the best therapeutic intervention, several investigators have retrospectively compared the outcomes of open airway surgery versus endoscopic treatments (laser, dilation) in idiopathic LTS. Initial endoscopic treatment is recommended for lesions less than 1 cm in length and without cartilage collapse because of the high rate of symptomatic relief and the minimal complications reported in this group.17,18 Many proponents of surgical therapies advocate bronchoscopic treatment initially, provided that it is not repeated if the stenosis returns to its initial grade afterward.21 Others propose that primary resection and reanastomosis should be offered to patients with disease refractory to three (not one) bronchoscopic procedures.17
Although treatment algorithms may be helpful in providing guidance, treatment decisions should be individualized according to causes, functional impairment, comorbidities, the site and severity of stenosis, and the function of the vocal cords.21 Our patient, for example, has a very high lesion with glottic extension, associated inflammation, and diabetes. These increase her risk for postoperative complications.13 At the same time, although bronchoscopic treatment is justifiable as an initial treatment, repeated procedures probably should be reserved for patients in whom definitive resection is deemed inappropriate because of unresectability, inoperability, patient choice, or surgeon preference in light of excessive risk for restenosis or procedure-related complications due to anatomy, surgical inexperience, severe inflammation, or proximity to the glottis.
Therapeutic Alternatives for Restoring Airway Patency
• Dilation: One study analyzed a total of 384 procedures performed in 127 patients with multifactorial LTS: 91 (72%) patients underwent primary dilation, of whom 12 (13%) were cured, 4 (4%) had evidence of persistent LTS but did not require further treatment, and 11 (12%) were lost to follow-up.22 Dilation can be performed with tapered Savary-Gilliard dilators, Jackson dilators, bougies, or angioplasty balloons after radial laser or electrocautery incisions.23
• KTP laser: As compared with the CO2 laser, its tissue penetration is significantly deeper, so that special attention must be paid to avoid perforation of the airway.
• Nd : YAG laser: This approach is used in conjunction with dilation to release the tension of the stricture by performing radial incisions in the stenotic tissues.24 Use of Nd : YAG at a low power density in a noncontact mode, however, is considered by some experts to be unacceptable primary treatment that could cause more scarring and could preclude or complicate further open surgical interventions.21
• CO2 laser: This technique is used in suspension laryngoscopy for laryngeal and subglottic stenoses (Figure 6-5), or with a rigid bronchoscope and a CO2 laser coupler for tracheal and bronchial stenoses. In one study, 49 patients with laryngeal stenosis, 6 patients with tracheal stenosis, and 5 patients with combined laryngeal and tracheal stenosis underwent CO2 laser resection (total, 60 patients); follow-up was provided for 1 month to 8 years. Multiple procedures were required in 35 of 49 (71%) patients with laryngeal stenosis. Thirty-nine (80%) of these patients with laryngeal stenosis were successfully managed (average number of procedures in successful cases, 2.18). Factors found to be associated with poor results or failure include circumferential stricture longer than 1 cm in vertical dimension, tracheomalacia, previous history of severe bacterial infection associated with tracheostomy, and posterior laryngeal inlet scarring with arytenoid fixation.14,25 Based on laser-tissue interactions, the CO2 laser (10,600 nm) is the preferred laser for treating benign stenosis, because no scatter and no deep penetration occur; therefore, the risk for collateral mucosal damage or airway perforation, respectively, is lower26; it is used in the ultrapulse mode with a fluence* of 150 mJ/cm2 at a frequency of 10 Hz to avoid charring and heat diffusion into surrounding tissues.21
• Spray cryotherapy: Liquid nitrogen (−196° C) is applied directly to the tissue via a low-pressure, disposable 7-French catheter; the published experience is still very limited for airway applications. In a case series, three patients were successfully treated using balloon dilation and four cycles of 5 second spray cryotherapy with complete thaw of the treated area between applications; no further interventions were required at 9 months’ follow-up.27
• Metal stent insertion is associated with significant complications, including granulation tissue, extension of stenoses, perforation, and hemoptysis.28,29 The Food and Drug Administration (FDA) warns that metallic tracheal stents in patients with benign airway disorders should be used only after all other treatment options (such as surgical procedures or placement of silicone stents) have been thoroughly explored. Use of these stents as a bridging therapy to surgery is not recommended, because removal of these stents is associated with significant complications.29 In one study, all patients with LTS who had undergone covered or uncovered metallic stent placement developed new strictures or granulation tissue, which precluded definitive surgical treatment or required more extensive resections.30
• Silicone stents are placed under rigid bronchoscopy or suspension laryngoscopy for inoperable or unresectable patients with recurrent high LTS despite repeated dilations. When sitting in the subglottic regions, the proximal end of the stent may induce ulceration and granulation tissue formation with subsequent glotto-subglottic restenosis.
• Airway reconstruction, such as laryngotracheoplasty, cricotracheal resection, or tracheal resection, could be the primary treatment considered for patients who become operable candidates after bronchoscopic intervention, as well as for operable candidates who have failed bronchoscopic treatment. Cricotracheal resection with primary thyrotracheal anastomosis is considered by some to be the procedure of choice for the treatment of severe idiopathic LTS (>70% luminal obstruction).31,32 Data suggest that fewer patients required subsequent intervention after primary airway reconstruction (27%) than after a dilation treatment (70%).33 Resection is usually successful. Mortality among patients who had anastomotic complications was 7.4% (6/81), whereas it was 0.01% among those without anastomotic complications. Anastomotic complications are uncommon in idiopathic LTS. Important risk factors are reoperation, diabetes, lengthy resections, laryngotracheal resections, young patient age (pediatric patients), and the need for tracheostomy before operation.9 A laryngotracheal resection with anastomosis to the larynx was also associated with a higher anastomotic failure rate (odds ratio, 1.8). Advantages of major airway reconstruction are that it consists of single-stage, definitive treatments. However, these treatments are associated with higher mortality and morbidity than dilation, including unilateral recurrent laryngeal nerve palsy, neck abscess, pneumothorax, and subcutaneous emphysema. This surgery can also significantly impact the adult female voice, lowering the pitch of the speaking voice into the male range and reducing pitch range. The change in voice that potentially accompanies this procedure should be discussed with patients during a preoperative counseling session.33
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree