Bronchiectasis
Allen P. Burke, M.D.
Definition
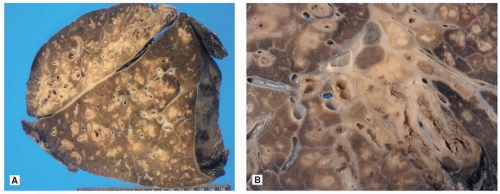
Bronchiectasis is a descriptive term for irreversibly dilated, thickened, and inflamed bronchi. Diffuse bronchiectasis is a hallmark of cystic fibrosis. Non-cystic fibrosis bronchiectasis is caused by recurrent infections of diverse causes, resulting in bacterial colonization of the lower respiratory tract, inflammation, and frequent exacerbations.1 Bronchiectasis syndromes are occasionally divided into three groups: cystic fibrosis, primary ciliary dyskinesia (PCD), and non-cystic fibrosis bronchiectasis.2
The term “traction bronchiectasis” or “bronchiolectasis” is primarily used by radiologists and indicates peripheral bronchiolectasis caused by diffuse interstitial lung disease with fibrosis and is not a primary inflammatory process. The term “bronchiolectasis” is infrequently used by pathologists and may be a histologic feature of honeycomb lung.
Incidence
The incidence of bronchiectasis has declined in developed countries with the decrease in prevalence of pertussis and other illnesses prevented by vaccination, and bacterial and tuberculous pneumonia. The true incidence is difficult to ascertain and depends on location and diagnostic assessment. Based on diagnostic reporting, the annual incidence in Finland was estimated at 3.9 per 100,000, with a range of 0.5 at age 0 to 14 years to 10.4 at 65 years.3 Estimates for the United States are far higher, at 4 per 100,000 at ages 18 to 34 to over 100 per 100,000 over age 65.4 In South Korea, a full 9% of patients were diagnosed with bronchiectasis by screening CT scans of volunteers.5
Etiology
Bronchiectasis is the result of recurrent respiratory infections, with a variety of underlying conditions, including genetic diseases, socioeconomic factors, and subtle alterations in immune function. A list of the more common entities is shown in Table 31.1. Central bronchiectasis is typical, if not pathognomonic, of allergic bronchopulmonary aspergillosis.7 Chronic aspiration, asthma, primary immune deficiency syndromes (e.g., chronic granulomatous disease, common variable immunodeficiency), and ciliary dyskinesia are potential causes for recurrent infections resulting in bronchiectasis. The largest single group is idiopathic. In a retrospective study throughout the country of Ireland, causes of non-cystic fibrosis-related bronchiectasis were idiopathic (32%), postpneumonia (17%), immune deficiency (16%), recurrent aspiration (16%), primary ciliary dyskinesia (9%), chronic aspiration with immune deficiency (5%), post foreign body inhalation (2%), tracheomalacia (1%), and obliterative bronchiolitis (1%).8 Bronchiectasis is prevalent in adults with chronic obstructive lung disease and recurrent pneumonia and is associated with poorer lung function, more frequent exacerbations, and a higher rate of Pseudomonas infections.9
TABLE 31.1 Bronchiectasis, Causes, and Associations | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
An underlying disorder is identified in the majority of children with bronchiectasis, including infections (17%), primary immunodeficiency (16%), aspiration (10%), ciliary dyskinesia (9%), congenital malformation (3%), and secondary immunodeficiency (3%).10
In developed countries, a history of tuberculosis and advanced age are associated with bronchiectasis.5 In developing countries, children with bronchiectasis are more likely to have underlying lung disease (especially asthma), chronic sinusitis, immunodeficiency, central nervous system disorders predisposing to aspiration, and cardiac conditions compared to the normal population.11 Lipoid pneumonia following aspiration of oils is a common predisposing factor in some parts of Africa and the Middle East12.
Patients with autoimmune disorders, including rheumatoid arthritis, Sjögren syndrome, relapsing polychondritis, and inflammatory bowel disease are more likely to develop bronchiectasis.13 The mechanisms are diverse and include immunosuppression, lung involvement, and esophageal hypomotility. Patients with systemic sclerosis and bronchiectasis are characterized by an older age, a high frequency of hiatus hernia, increased respiratory infections, a low incidence of anti-Ro/SS-A, and high frequency of anti-smooth muscle antibodies.14 Bronchiectasis in rheumatoid arthritis often occurs in patients with severe, long-standing nodular disease and causes recurrent pulmonary infections that may result in fatal respiratory failure.15
Primary Ciliary Dyskinesia
PCD is a rare autosomal recessive disease manifest by structural and functional abnormalities of the motile cilia. Disease-causing mutations in at least 16 genes have already been identified, including biallelic mutations in multiple genes.16 Pathologic diagnosis rests on ultrastructural absence of dynein arms of the ciliary microtubules. However, up to 30% of patients may have normal ultrastructure, in whom genetic tests, ciliary motility, and nasal nitric oxide production studies may establish a diagnosis.
The estimated incidence of PCD is conservatively estimated at 1 per 15,000 births. Chronic infections of the ears, sinuses, and lungs are associated with organ laterality defects, typically situs inversus, in ˜50% of cases. There are typically recurrent episodes of respiratory tract infections. Pulmonary function tests show generally obstructive impairment. Lung biopsy shows nonspecific inflammation. Bronchiectasis (usually with situs inversus) is typical on chest imaging. Male infertility due to immotile spermatozoa is often present.
Given the heterogeneity and the rarity of the disorder, therapy is not evidence based and analogous with the treatment for cystic fibrosis.17,18
Cystic Fibrosis
Cystic fibrosis is an autosomal recessive disease caused by dysfunction of the cystic fibrosis transmembrane conductance receptor (CFTR) protein, resulting in an imbalance of chloride secretion and sodium absorption and airway surface dehydration.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree