Bronchiectasis
Jonathan H. Chung, MD
DIFFERENTIAL DIAGNOSIS
Common
Postinfectious
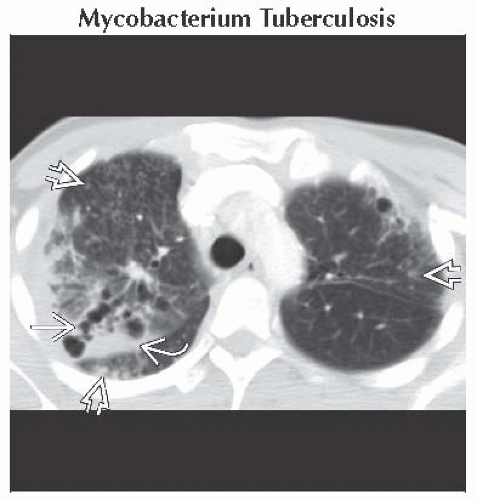
Mycobacterium Tuberculosis
Mycobacterial Avium Complex
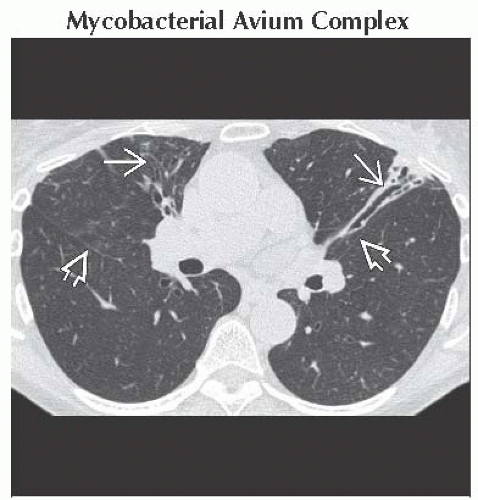
Swyer-James (MacLeod) Syndrome
Aspiration (Recurrent)
Postobstructive
Endobronchial Tumor
Lymphadenopathy
Foreign Body
Traction Bronchiectasis
Cystic Fibrosis
Asthma
Less Common
Allergic Bronchopulmonary Aspergillosis
Immotile Cilia Syndrome
Immunosuppression
Congenital
AIDS
Rare but Important
Williams-Campbell Syndrome
Tracheobronchomegaly (Mounier-Kuhn Syndrome)
Young Syndrome
Yellow-Nail Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Definition: Pathologic, irreversible dilation of bronchi
Helpful Clues for Common Diagnoses
Postinfectious
Mycobacterium Tuberculosis
Upper lung bronchiectasis
Signs of previous tuberculosis: Upper lung fibrocavitary disease, calcified lymph nodes, calcified granulomas
Low-attenuation lymphadenopathy, tree in bud or miliary nodules, or cavitary lung disease in active disease
Mycobacterial Avium Complex
Most common in older women
Cylindrical bronchiectasis most severe in middle lobe and lingula
Tree in bud nodules, larger random nodules (occasionally cavitate)
In minority of cases, mimics upper lung fibrocavitary disease of reactivation tuberculosis
Swyer-James (MacLeod) Syndrome
Due to childhood pneumonia (adenovirus, measles, Mycoplasma, pertussis)
Bilateral but asymmetric process; usually more involvement of 1 lung
Unilateral hyperlucency of more affected lung: Hypoplasia of pulmonary vasculature and constrictive bronchiolitis
Small to normal size of more affected lung
Aspiration (Recurrent)
Predisposition in patients with neuromuscular disorders or esophageal abnormalities
Dependent portions of lungs: Superior and basilar segments of lower lobes (right greater than left)
Postobstructive
Endobronchial Tumor
Squamous cell carcinoma in older patients with history of smoking
Carcinoid tumor in young patients; often low activity on FDG PET
Lymphadenopathy
Chronic extrinsic compression of bronchi
A cause of middle lobe syndrome: Chronic atelectasis and bronchiectasis in middle lobe or lingula
Foreign Body
Abnormal fixed hyperinflation > atelectasis of lung or lobe even with expiration or lateral decubitus positioning
Direct visualization of foreign body (CT > radiographs)
Traction Bronchiectasis
Concomitant end-stage lung disease or pulmonary fibrosis, radiation fibrosis
Reticular opacities, interlobular septal thickening, architectural distortion, honeycombing
Cystic Fibrosis
Upper lung bronchiectasis; air-trapping; tree in bud opacities &/or centrilobular nodules
Fatty atrophy of pancreas
Asthma
Mild cylindrical bronchiectasis with patchy regions of air-trapping and bronchial wall thickening
Helpful Clues for Less Common Diagnoses
Allergic Bronchopulmonary Aspergillosis
Central cystic bronchiectasis and severe mucus plugging or air-fluid levels in asthmatic
Immotile Cilia Syndrome
Middle and lower lobe bronchiectasis, situs inversus/dextrocardiac in 50%, paranasal sinusitis, male infertility
Immunosuppression
Congenital
e.g., primary impaired cellular or humoral immunity, infantile X-linked agammaglobulinemia
Bronchiectasis secondary to recurrent infection
Hypogammaglobulinemia: Lower lung preponderance, severe bronchial wall thickening
Common variable immune deficiency syndrome: Concomitant reticular opacities
AIDS
Likely secondary to recurrent bacterial infection; lower lobe preponderance; air-trapping
Helpful Clues for Rare Diagnoses
Williams-Campbell Syndrome
Defective cartilage in 4th to 6th order bronchi
Central cystic bronchiectasis; collapse with expiration and dilation with inspiration
Tracheobronchomegaly (Mounier-Kuhn Syndrome)
Dilation of trachea and main bronchi; tracheal diverticula along posterior aspect of trachea; ± tracheomalacia
Central cystic bronchiectasis
Young Syndrome
Resembles immotile cilia syndrome: Paranasal sinusitis, bronchiectasis, male infertility
Yellow-Nail Syndrome
Bronchiectasis in setting of abnormally thick, discolored nails; exudative pleural effusions; lymphedema
Alternative Differential Approaches
Unilateral bronchiectasis
Post-primary tuberculosis
Bronchial stenosis: Bronchial atresia, postinfectious, sarcoidosis
Obstructing endobronchial tumor
Foreign body
Bilateral or diffuse bronchiectasis
Congenital: Cystic fibrosis, immotile cilia syndrome, congenital immunodeficiency
Infection: Recurrent aspiration, post-viral, allergic bronchopulmonary aspergillosis
Traction bronchiectasis
Image Gallery
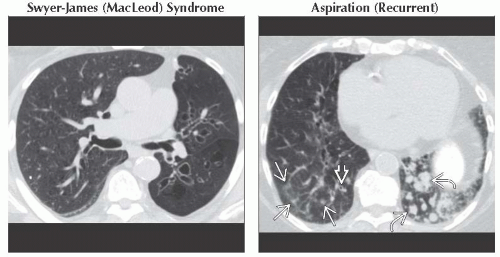 (Left) Axial NECT shows bronchiectasis, paucity of vessels, and decreased density of the left lung, consistent with Swyer-James (MacLeod) syndrome. The patient had a history of a severe childhood respiratory infection. (Right) Axial NECT shows left lower lobe patchy centrilobular opacities
 and mild peribronchial thickening and mild peribronchial thickening  as well as left lower lobe mucus plugging within bronchiectatic airways as well as left lower lobe mucus plugging within bronchiectatic airways  in this patient with a history of chronic aspiration. in this patient with a history of chronic aspiration.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|