Figures 38.1 and 38.2
If the extent of contamination and inflammation of the surrounding regions is limited and it is assumed to be localized within the chest, right thoracotomy, necrosectomy, and primary closure of the perforation should be performed, if possible with local reinforcement. A double-lumen endotracheal tube is required for single-lung ventilation. A broad-spectrum antibiotic should be given before skin incision. Because of uncontrollable conditions due to the perforation, no nasogastric tube should be inserted before surgery. The patient is placed in the typical left lateral decubitus position. The table is flexed at the hips, and the right arm is adequately supported. All pressure points are carefully padded. The surgeon stands on the right, at the back of the patient, with the first assistant opposite. Dorsolateral thoracotomy is performed. The incision is carried from the anterior edge of the latissimus dorsi muscle at the level of the mamilla surrounding the lower scapula edge upward in parallel to the paravertebral muscles. The latissimus dorsi muscle is dissected, and the scapula and anterior serratus muscle are lifted off the chest wall. Above the fifth rib, the intercostal muscles and pleura are dissected, and the rib spreader is placed and opened carefully. After exploration of the chest space, mobilization of the esophagus, and assessment of the wound edges, the indication for primary closure must be reevaluated. If the extent of contamination and inflammation of the surrounding regions is limited, a primary closure of the perforation should be performed. At this point, it is possible to move the nasogastric tube within the esophagus, inspecting the esophagus while leading and passing the tube across the perforation. The wound may be reapproximated by a running suture placed only in the mucosa. A second layer of interrupted sutures is placed in the muscular wall of the esophagus. The closure may be reinforced by a pleural flap, which may be used to cover the sutures. The adjacent mediastinal pleura is incised widely to ensure adequate drainage into the pleural space, which in turn is drained in the usual manner. The fascia and skin are closed via standard techniques. If there is additional involvement of the abdominal space, subsequent laparoscopy with exploration, lavage, and selected placement of drains is indicated. (a) Approach. (b) Closure of the lesion
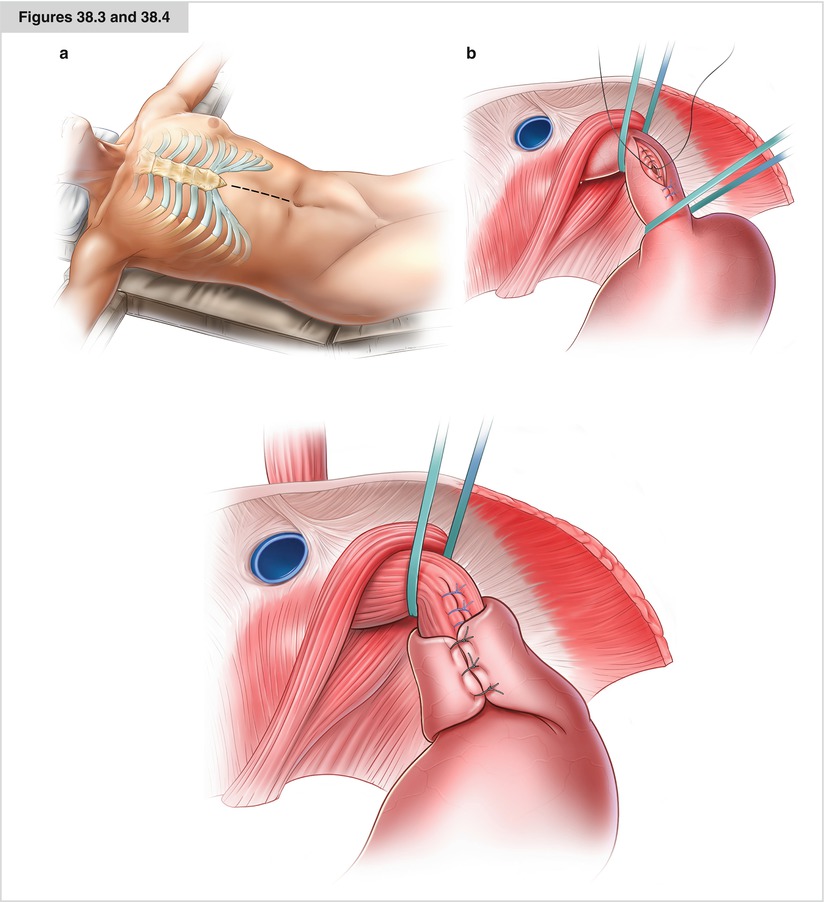
Figures 38.3 and 38.4




If the extent of contamination and inflammation of the surrounding regions is limited and assumed to be localized in the abdominal space, median laparotomy, necrosectomy, and primary closure of the perforation with a (hemi)fundoplication to cover the suture should be performed. A broad-spectrum antibiotic should be given before skin incision. Because of uncontrollable conditions due to the perforation, no nasogastric tube should be inserted before surgery. Under general anesthesia, the patient is placed in the typical supine decubitus position. The table is slightly flexed at the hips with the arms extended at the side. All pressure points are carefully padded. The surgeon stands on the right, the first assistant opposite. Median laparotomy is performed. The incision is carried from the xiphoid process down to the navel. The fascia and peritoneum are dissected carefully, and a Rochard retractor is placed. After exploration of the abdominal space and mobilization of the left liver lobe, the gastrohepatic ligament is dissected and divided. Care should be taken to identify and avoid dissection of an aberrant left hepatic artery within the gastrohepatic ligament. Next, the crura of the diaphragm are exposed at the gastroesophageal junction. While assessing the wound edges, the surgeon must reevaluate the indication for primary closure. The space between the esophagus and the crura is opened bluntly. The retroesophageal space is dissected under direct vision. The distal esophagus should be mobilized until the whole perforation is exposed. At this point, it is possible to move the nasogastric tube within the esophagus, inspecting the esophagus while leading and passing the tube across the perforation. If the extent of contamination and inflammation of the surrounding regions is limited, primary closure of the perforation should be performed. The wound may be reapproximated by a running suture placed only in the mucosa. A second layer of interrupted sutures is placed in the muscular wall of the esophagus. The adjacent mediastinum should be opened enough to ensure adequate drainage into the abdominal space, which in turn is drained in the usual manner. (Hemi)fundoplication is used to cover the suture. To achieve a tension-free wrap, it is necessary to mobilize the gastric fundus. The fundus is pulled gently across the back of the gastroesophageal junction. With the same segment of stomach pulled around the esophagus, a 360° or 270° wrap is created and fixed in a length of 2–3 cm and should be located and fixed over the suture of the perforation. Lavage of the whole abdominal space is necessary, and the hiatus should be drained. The fascia and skin are closed using standard techniques. If there is further involvement of the thoracic space, subsequent thoracoscopy with exploration, lavage, and selected placement of drains is indicated. (a) Approach. (b) Closure of the lesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


