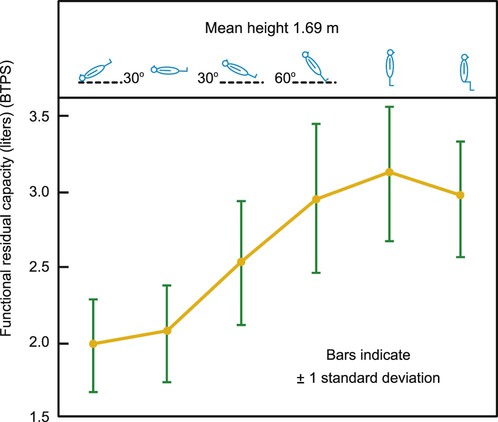
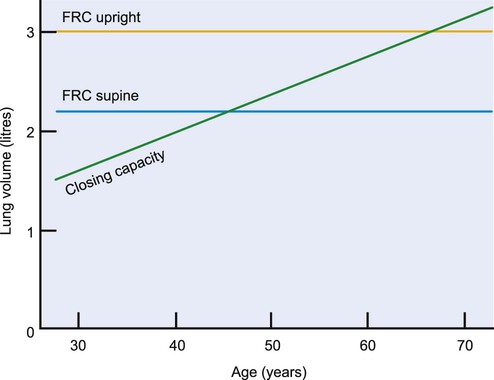
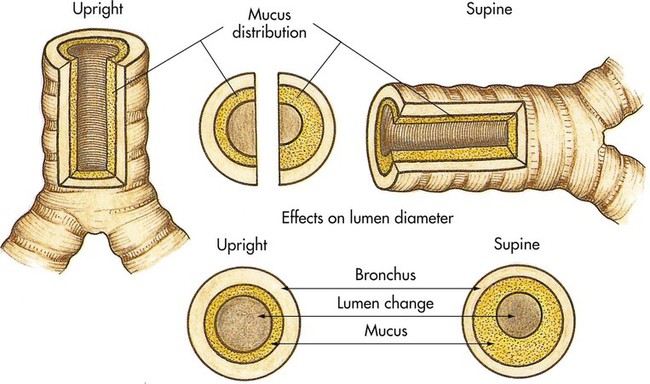
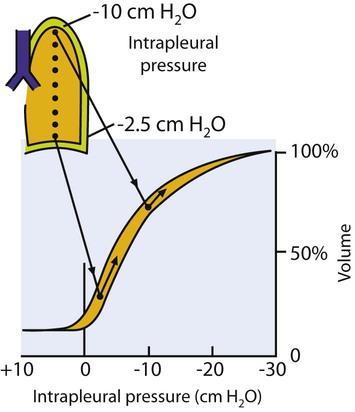
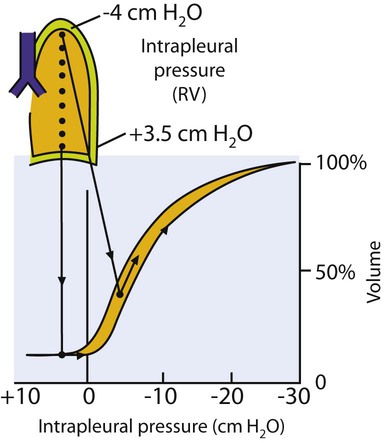
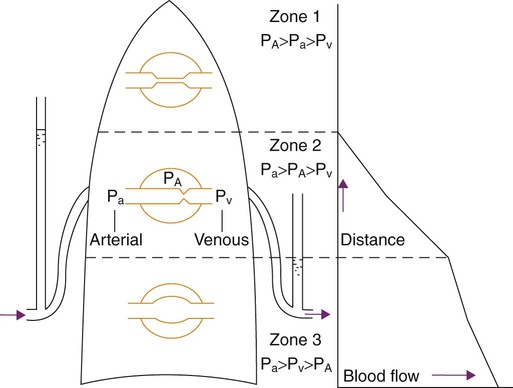
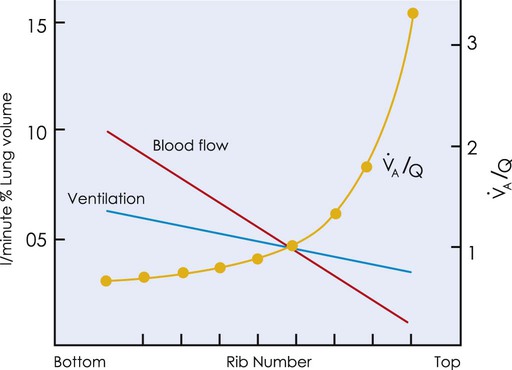
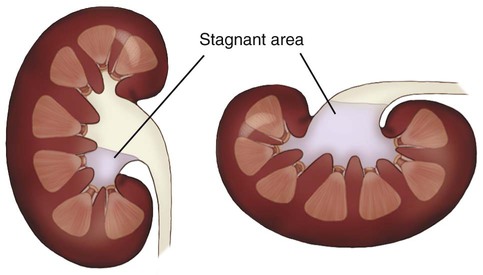
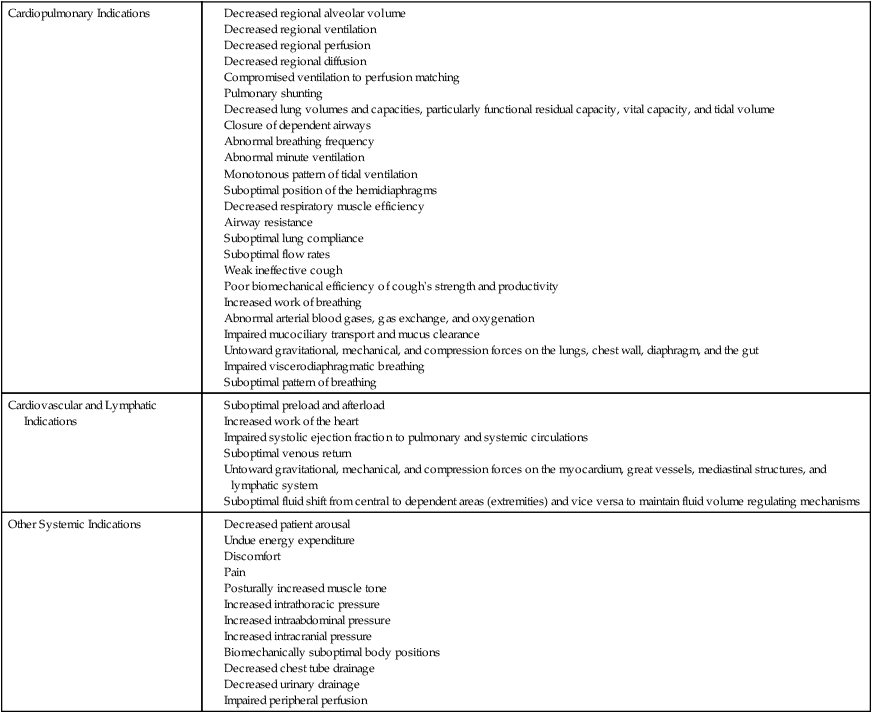
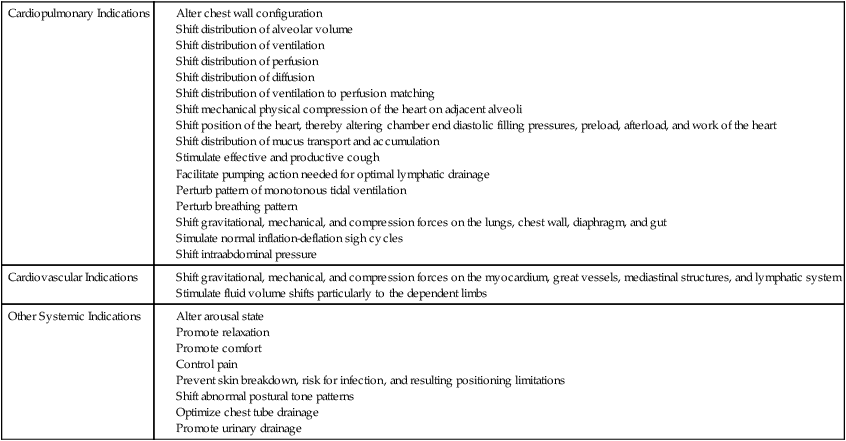
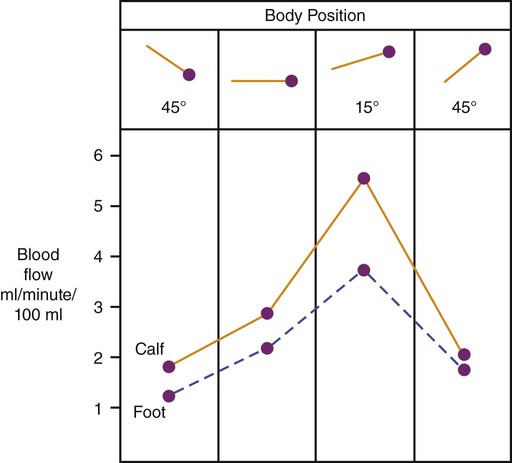
Specific indications for body positioning and the decision-making process are highlighted. The chapter does not provide treatment prescriptions for given conditions because no specific patient is being considered. Understanding the physiological effects of body position on oxygen transport and how pathophysiology disrupts these normal processes is fundamental to prescribing body positioning for a given patient. An optimal body position can be prescribed only on the basis of consideration of all factors that impact on oxygen transport: the effects of the patient’s pathophysiology and its specific presentation in that individual, the effect of restricted mobility and recumbency, the effect of extrinsic factors related to the patient’s care, and the effect of intrinsic factors related to the patient (Chapter 17). It is only with an integrated analysis of these factors overall that (1) the most beneficial body positions can be predicted; (2) the least beneficial body positions can be identified and used minimally; and (3) the appropriate outcome measures can be selected. The human is an orthograde organism. From moment to moment, gravity exerts its influence on the human body and particularly affects oxygen transport. The combined effects of gravity on the lungs, heart, and peripheral circulation are central to their interdependent function and to establishing normal oxygen transport. Knowledge of the effects of gravity on cardiovascular and pulmonary function in health and the deleterious effects of pathophysiological states on cardiovascular and pulmonary function (both primary pathology of the cardiovascular and pulmonary system and pathology of this system secondary to pathology in one or more other systems, as described in Chapter 6) provides a foundation for therapeutic body positioning as a primary intervention to optimize oxygen transport. Because of its potent and direct effect on oxygen transport, therapeutic body positioning can maintain or augment arterial oxygenation so that invasive, mechanical, and pharmacological forms of respiratory support can be postponed, reduced, or avoided—a primary objective of cardiovascular and pulmonary physical therapy. In health, normal oxygen transport is maintained by being upright and moving—the physiological body position. A patient who may have prolonged periods of recumbency is also exposed to gravity continuously, but not to the same extent as in the upright position. Each body position the patient assumes differentially affects the steps of the oxygen transport pathway as a result of alterations in gravitational stress. Oxygen transport can be improved, maintained, or worsened with changes in body position. Despite being essential to normal cardiovascular and pulmonary function, gravity is the principal contributor to inhomogeneity of physiological function down the lungs.1 Figure 20-1 illustrates the effect of this gradient with respect to alveolar ventilation ( Based on a detailed analysis of all factors contributing to impaired oxygen transport and gas exchange (Chapter 17), the body positions that will have an optimal effect on oxygenation and those that may be deleterious must be distinguished from one another. In this way, a greater proportion of time can be spent by the patient in beneficial positions and less time in deleterious positions. Body positions themselves are associated with energetic stress, particularly in positions with greater gravitational stress, so the upright position can be more energetically demanding than supine positions, which are more demanding than lateral positions.2 Compression forces also affect the heart and cardiac output. Lying on the left side, for example, can compromise cardiac output, particularly within 12 hours after surgery in patients whose cardiac index is less than 2.3 L/min/m2.3 The length of time a body position is maintained is response-dependent rather than time-dependent,4 and it reflects individual differences, including pathology, severity, age, and body mass. Knowledge of the deleterious effects of prolonged periods in a single position supports the prescription of both frequent body position changes and extreme sequential body positions. These perturbations simulate the normal perturbations that the cardiovascular and pulmonary systems experience in health during normal mobility and body position changes in daily life. The ability to weigh the relative beneficial and deleterious effects of each possible body position (through 360 degrees in the horizontal plane and 180 degrees in the vertical plane, ranging from approximately 20 degrees head down to 20 degrees leaning forward) on a given patient’s gas exchange is critical in prescribing body positioning. The literature supports the benefits of frequent body position changes, particularly for a patient who is relatively immobile, not alert, severely debilitated, obtunded, breathing at low lung volumes, obese, aged or very young, or has lost the sigh mechanism. Even though the effectiveness of routinely turning patients every 2 hours has not been firmly established, it continues to be an accepted standard of care (although intensive care units fall short of this minimal guideline).5 The practice is based on the belief that the deleterious consequences associated with assuming a static position for a prolonged period will be prevented. More frequent turning, however, may have greater physiological benefits in patients who are critically ill, and this suggests that patients who are less severely ill may also benefit from being gravitationally challenged systematically. The preventive effects of a routine turning regimen are distinct from the acute effects of body positioning on oxygen transport, which is the primary focus of this chapter. Body positioning has potent and direct effects on most steps of the oxygen transport pathway, so it can be prescribed to elicit these effects preferentially. Because humans function optimally when upright and moving, therapeutic interventions that elicit or simulate being upright and moving (i.e., elicit both gravitational and exercise stress) are most justified physiologically (see Chapter 17). The recumbent supine position, a common position assumed by patients who are hospitalized, is nonphysiological and is deleterious to oxygen transport. The side-lying positions have an effect that is intermediate between that of upright and supine. The prone position, which is underutilized clinically, can have such a significant powerful effect on oxygen transport that a good rationale must be made for not incorporating this position into the treatment prescription. The indications for therapeutic body positioning and for frequent body position changes to optimize oxygen transport are shown in Tables 20-1 and 20-2. For each of the indications listed, an optimal therapeutic body position can be selected for a given patient. A description of the physiological effects of several primary body positions follow, namely, the upright/supine, side-lying, head-down, and prone positions. However, this information cannot be applied out of context. The specific positions prescribed for a given patient are based on consideration of the multiple factors that impair oxygen transport (Chapter 17) in conjunction with a physiological analysis of the most justifiable positions. Table 20-1 Indications for Body Positioning to Optimize Oxygen Transport Table 20-2 Indications for Frequent Changing of Body Position Because of the potent and direct effects of body positioning on the steps in the oxygen transport pathway in health and in disease, it is unknown whether the beneficial effects reported with the use of postural drainage are attributable to enhanced mucociliary transport; or to the direct effect of positioning the good lung down on improving the gas exchange of that lung by increasing alveolar volume of the affected, nondependent lung; or to both of these mechanisms. Typically, studies evaluating conventional chest physical therapy, including postural drainage, have failed to control for the direct effect of body positioning on oxygen transport or for the direct effects of increased arousal and mobilization that occur when a patient’s body position is changed.6,7 This is a serious methodological problem that pervades the literature evaluating conventional practices, so-called chest physical therapy, and one that has to be considered when interpreting the results of studies of these procedures. Unless these potent confounding variables are controlled, the degree to which conventional chest physical therapy has a beneficial effect over and above the effects of positioning, as well as of mobilization and increased arousal, cannot be established.8 Although the upright position is common to the physiological and anatomical positions, movement in the upright constitutes the true physiological position in that the upright position coupled with movement (e.g., walking, cycling, or movement in sitting) is consistent with the requirements of daily activities. To meet the energetic demands of these activities, oxygen transport is optimized to the greatest degree, in that ventilation and perfusion are more uniform than they would be without the additional exercise stimulus. The upright standing position maximizes lung volumes and capacities, with the exception of closing volume, which is decreased.9 Functional residual capacity (FRC), the volume of air remaining in the lungs at the end of end-tidal expiration, is greater in standing than in sitting and exceeds that in the supine position by as much as 50% (Figure 20-2). Maximizing FRC is associated with reduced airway closure and maximal arterial oxygenation.10,11 Figure 20-3 illustrates the relationship of FRC and closing capacity as a function of age. Because of age-related pulmonary changes, the closing capacity of the dependent airways increases with age; this effect is further accentuated with recumbency. Airway closure is evident in the supine position in the healthy 45-year-old person and in the upright seated position in the healthy 65-year-old person.12 Compression atelectasis results from cardiac weight, abdominal pressure, and pleural effusions, the effects of which are determined by the specific position of the patient.13 These positional effects are further accentuated in patient populations with cardiovascular and pulmonary, thoracic, and abdominal pathologies, so the upright position is favored, and the supine position should be minimized so as to prevent airway closure and impaired gas exchange. With respect to pulmonary function testing, the upright sitting position with legs dependent is the standard reference position.14,15 When upright, the diameter of the main airways increases slightly. If the airways are obstructed, even small degrees of airway narrowing induced by recumbency can increase airway resistance (Figure 20-4). When a person is upright, the vertical gravitational gradient is maximal, the anteroposterior dimension of the chest wall is the greatest, and compression of the heart and lungs is minimized.16 The shortened position of the diaphragmatic fibers is countered by an increase in the neural drive to breathe when a person is in the upright position.17 Maximal expiratory pressure is augmented with progressively upright positions in patients with chronic obstructive lung disease, as well as in those in health; standing results in the highest values and head-down positions the lowest.18 Thus coughing and other forced expiratory maneuvers should be encouraged when the individual is in the optimal erect, upright position. The distribution of ventilation is determined primarily by the effect of gravity, which changes down the lung because of the anatomical position and the suspension of the lungs within the chest. At FRC in the upright position, the intrapleural pressure at the apex is −10 cm H2O and at the base −2.5 cm H2O (Figure 20-5). The intrapleural pressure is less negative in the base because of the suspended mass of the lungs. As a result of the greater negative intrapleural pressure in the apices, thus low compliance, these lung units have a larger initial volume; hence smaller volume changes occur during respiration. Because the lung units at the base have a smaller initial volume, thus high compliance, larger volume changes occur during respiration. Therefore, depending on their relative position with respect to gravity, different regions of the lung are at different points on the pressure volume curve. A common clinical concern is patients breathing at low lung volumes—for example, patients in pain, patients who have undergone thoracic or abdominal incisions, older and younger patients, obese patients, pregnant patients, patients with gastrointestinal dysfunction (such as paralytic ileus and ascites, organomegaly, or intrathoracic or intraabdominal masses) patients who are malnourished, and patients who are mechanically ventilated or have spinal cord injuries). Breathing at low lung volumes reverses the normal intrapleural pressure gradient such that in the upright lung the apices have a negative intrapleural pressure compared with the bases, which have a positive intrapleural pressure (i.e., exceeding airway pressure) (Figure 20-6). This results in the apices being more compliant, thus better ventilated, than the bases. The bases are prone to airway closure in individuals breathing at low lung volumes. Another factor that reverses the normal intrapleural pressure gradient is mechanical ventilation. Despite its necessity in the management of patients in respiratory failure, mechanical ventilation can contribute to hypoxemia in several ways. First, it reverses the normal intrapleural pressure gradient so that the uppermost lung fields are preferentially ventilated. Because the dependent lung fields are preferentially perfused, Although gravity is the primary determinant of interregional differences in the distribution of ventilation in the healthy lung, intraregional differences, secondary to differences in compliance and resistance of contiguous lung units, also contribute.22 These effects are exaggerated in patient populations.23 The distribution of perfusion down the upright lung is also primarily dependent on gravity (Figure 20-7). The pressures affecting blood flow through the pulmonary capillaries and resulting in the typical uneven distribution (inhomogeneity) of blood flow are alveolar pressure and the arterial and venous pressures. In zone 1, at the apex, alveolar pressure predominates over arterial and venous pressures, so there is little or no blood flow. Zone 2, in the middle zone, reflects the blood flow from the recruitment of pulmonary vessels. Arterial pressure exceeds alveolar pressure and blood flow. Zone 3, in the lower area of the lung, reflects the blood flow from the distension of pulmonary vessels; arterial and venous pressures exceed alveolar pressure. And zone 4 (not illustrated), in the most dependent portion of the lung, has little or no pulmonary blood flow because of the interstitial pressure acting on the pulmonary blood vessels and creating a compression force.1 The matching of The upright position is associated with marked hemodynamic effects. These effects reflect primarily the central blood volume, which is shifted from the thoracic compartment to the dependent venous compartments when a person assumes the upright position from the supine.25–27 End-diastolic volume and stroke volume are decreased, which results in a compensatory increase in heart rate.28 Cardiac output is correspondingly decreased. The net effect of these physiological changes is a reduction in myocardial work.29 This finding is corroborated by the observation that the anginal threshold is increased in patients with cardiac conditions when they are upright.30 Further, intermittent gravitational stress following myocardial infarction or bypass surgery maintains orthostatic tolerance and thereby prevents bed rest deconditioning.31 Peripheral vascular resistance increases and blood flow decreases with the assumption of an upright position greater than 45 degrees to offset dependent fluid shifts and potential blood pressure drop (Figure 20-9). An upright angle of at least 60 degrees is needed to optimize cardiac output and sympathetic tone.32 Another important effect of body position on fluid volume is the promotion of urinary drainage from the renal pelvi to the bladder when in the upright position, as a result of the reduced area for urinary stasis when in this position as opposed to the supine position (Figure 20-10). Optimal renal function is essential to preserving normal hemodynamic status. Older individuals who are relatively immobile tend to sit for prolonged periods. Without frequent exposure to standing upright, however, the phenomenon of seated postural hypotension may result.33 In addition, dependent circulatory stasis and other consequences of restricted mobility such as deconditioning are promoted in this position.
Body Positioning
Gravity and Normal Physiological Function: Physical Therapy Implications
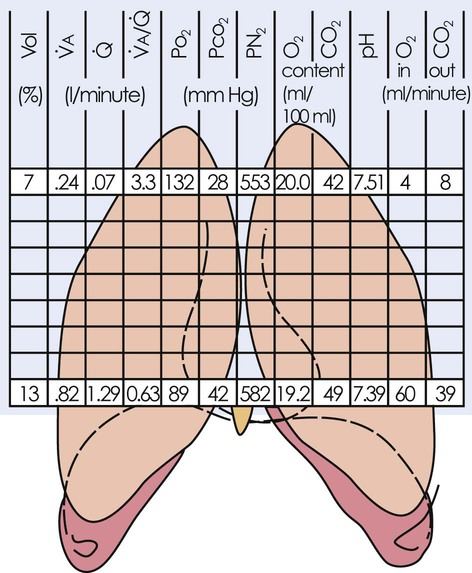
 ), perfusion (Q), ventilation and perfusion ratio (
), perfusion (Q), ventilation and perfusion ratio ( ), PaO2, PCO2, PN2, oxygen content, carbon dioxide (CO2) content, pH, and the flow of oxygen and CO2 in and out of the lungs. Thus the lungs should not be likened to balloons, either physiologically or anatomically.
), PaO2, PCO2, PN2, oxygen content, carbon dioxide (CO2) content, pH, and the flow of oxygen and CO2 in and out of the lungs. Thus the lungs should not be likened to balloons, either physiologically or anatomically.
Prescriptive Versus Routine Body Positioning
Physiological Effects of Various Body Positions
Upright Positions
 mismatch is promoted. Positive pressure ventilation has the additional complication of increasing intrathoracic pressure and reducing venous return and cardiac output. These factors, in addition to the negative pressure required to open the inspiratory valve, can increase the work of breathing associated with mechanical ventilation.19–21
mismatch is promoted. Positive pressure ventilation has the additional complication of increasing intrathoracic pressure and reducing venous return and cardiac output. These factors, in addition to the negative pressure required to open the inspiratory valve, can increase the work of breathing associated with mechanical ventilation.19–21
 and Q reflects the interfacing of the distributions of
and Q reflects the interfacing of the distributions of  and Q down the upright lung. Both
and Q down the upright lung. Both  and Q increase down the upright lung; however,
and Q increase down the upright lung; however,  increases disproportionately more than Q (Figure 20-8). As a result, the optimal area for
increases disproportionately more than Q (Figure 20-8). As a result, the optimal area for  matching is in the midzone, where the ratio is about 1.0.24
matching is in the midzone, where the ratio is about 1.0.24
Body Positioning

 , ventilation-perfusion ratio.
, ventilation-perfusion ratio.  ) and perfusion (Q), and optimize
) and perfusion (Q), and optimize  matching commensurate with physiological demand. When body positions that are initially beneficial to the patient are assumed for too long, hydrostatic, gravitational, and compression forces acting on the heart, blood volume, lymphatic system, lungs, and chest wall, including the diaphragm, eventually compromise oxygen transport, offsetting any benefit. Therefore close monitoring is essential to ensure that the patient is turned to another position before the effects become detrimental. Frequent changes in body position and avoidance of prolonged periods in any single position minimize this risk.
matching commensurate with physiological demand. When body positions that are initially beneficial to the patient are assumed for too long, hydrostatic, gravitational, and compression forces acting on the heart, blood volume, lymphatic system, lungs, and chest wall, including the diaphragm, eventually compromise oxygen transport, offsetting any benefit. Therefore close monitoring is essential to ensure that the patient is turned to another position before the effects become detrimental. Frequent changes in body position and avoidance of prolonged periods in any single position minimize this risk.