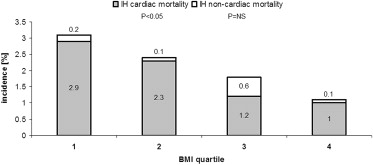
The clinical outcome of acute cardiovascular events may be more favorable in patients with a high body mass index (BMI), although obesity increases the risk for cardiovascular diseases. The authors sought to define the association between BMI and acute and long-term outcome of patients presenting within 12 hours of ST-segment myocardial infarction (STEMI) in a large multinational cohort. A total of 3,579 patients enrolled in the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction trial were stratified according to BMI quartiles: <24.5, 24.5 to <27.1, 27.1 to 30.1, and >30.1 kg/m 2 (quartiles 1, 2, 3, and 4, respectively). Death, myocardial reinfarction, ischemia-driven target vessel revascularization, stroke, and noncoronary artery bypass grafting-related major bleeding events were centrally adjudicated for the acute, 30 days, and yearly follow-up. Patients with a BMI in the highest quartile were younger than patients in the lower BMI quartiles and more frequently had hypertension, hyperlipidemia, and diabetes mellitus. Complete occlusions and noncalcified lesions were more common in patients with a high BMI. In-hospital mortality decreased with increasing BMI due to lower cardiac mortality (2.9%, 2.3%, 1.2%, and 1.0% for quartiles 1, 2, 3, and 4, respectively, p <0.05). Out-of-hospital 3-year mortality was also lower in higher-weight patients due to lower noncardiac mortality (4.2%, 2.6%, 2.3%, and 1.7% for quartiles 1 to 4, respectively, p = 0.01). After adjustment for covariates, BMI was no longer predictive of acute or long-term mortality after STEMI. In conclusion, as BMI increases, patients have a more extensive adjusted cardiovascular risk profile and disease burden and premature STEMI onset but similar adjusted acute and long-term outcomes.
The relation between body mass index (BMI) and mortality is not well understood. Some studies suggest a U-shaped association with an increase in total mortality in both underweight and overweight patients, whereas other studies show a positive linear association. Obesity is associated with a cluster of cardiovascular risk factors and has been associated with an earlier presentation of coronary artery disease (CAD) including acute myocardial infarction (AMI). Paradoxically, however, patients with higher BMI have better outcomes after AMI. Similar results were observed after percutaneous coronary intervention (PCI) ; yet recent data from the National Cardiovascular Data Registry point out worse outcomes among the extremely obese (BMI >40 kg/m 2 ) after primary PCI. Following coronary artery bypass grafting (CABG), low rather than high body weight may be a risk factor for complications and mortality. Finally, long-term mortality risk is lowest among obese patients with stable CAD in general. The reasons for this obesity paradox are presently not clear but may include earlier and more aggressive, guideline-recommended therapies. Alternatively, better outcomes with higher BMI may simply reflect confounding variables, including age and the association of underweight with frailty or cancer, or skewing of data when cohorts are unequally divided into standard categories of BMI. To analyze the influence of BMI on acute and long-term outcomes after AMI, we used the large and closely followed cohort of the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial.
Methods
The design and main results of the HORIZONS-AMI trial have been reported previously. We randomized 3,602 patients with ST-segment myocardial infarction (STEMI) to either unfractionated heparin plus glycoprotein IIb/IIIa inhibitor (1,802 patients) or bivalirudin (1,800 patients) in an open-label design. Following randomization, all patients underwent coronary angiography followed by, at the discretion of the treating physician, PCI, CABG, or medical management. When primary PCI was chosen and once patency in the infarct-related vessel was restored, patients were randomly assigned in a 3:1 ratio to paclitaxel-eluting stents (TAXUS Express, Boston Scientific, Natick, Massachusetts) or identical bare metal stents (Express, Boston Scientific, Natick, Massachusetts). Aspirin and thienopyridine were administered in standard dosing. End points were adjudicated by a clinical events committee unaware of treatment assignment. The prespecified primary 30-day end points were major bleeding (not related to CABG) and combined net adverse clinical events (either major bleeding or a composite of major adverse cardiac events, including death, reinfarction, target vessel revascularization for ischemia, and stroke). Stent thrombosis was defined in accordance with the Academic Research Consortium criteria. Binary angiographic restenosis was defined as a ≥50% diameter stenosis at angiographic follow-up at 13 months. Anemia was defined as a hematocrit value at initial presentation <39% for men and <36% for women, based on the World Health Organization criteria. Renal insufficiency was defined as a creatinine clearance <60 ml/min according to the Cockcroft-Gault equation.
Height and weight measurements were both available for 3,579 patients, who were then stratified by BMI into quartiles: ≤24.5 kg/m 2 (quartile 1), 24.5 to <27.1 kg/m 2 (quartile 2), 27.1 to 30.1 kg/m 2 (quartile 3), and >30.1 kg/m 2 (quartile 4). In addition to this retrospective, population-based approach, results were stratified in keeping with standard, a priori definitions of the World Health Organization for underweight/normal weight, overweight and mild obesity, and moderate to severe obesity, that is, BMI <25, 25 to 35, and >35 kg/m 2 , respectively.
Continuous variables, summarized as medians with interquartile ranges, were compared among quartile groups using the nonparametric Kruskal-Wallis test. Continuous variables, summarized as mean ± SD, were compared among quartile groups using analysis of variance, and only if a statistical difference was noted in this analysis, intergroup differences were tested with Bonferroni post-hoc analyses. Categorical variables are summarized using frequencies and percentages and compared among quartile groups using chi-square tests. Time-dependent outcomes were summarized using Kaplan-Meier estimates and compared between quartile groups using log-rank tests. Multivariate logistic regression analyses were performed to identify independent end point predictors and Cox regression models to identify independent time-to-event predictors of death, re-infarction, stroke, stent thrombosis, and major bleeding not related to CABG. The multivariable Cox/logistic model was performed by stepwise selection with entry/stay criteria of 0.1/0.1. BMI, bivalirudin randomization, age, gender, clopidogrel loading dose, hypertension, hyperlipidemia, diabetes mellitus (DM), previous MI, and symptom onset to balloon time were included in the list of candidate covariates.
Results
The clinical characteristics are listed in Table 1 . Patients in the fourth quartile, with a BMI >30.1 kg/m 2 , were significantly younger than patients in the lower BMI strata. The prevalence of systemic hypertension, hyperlipidemia, and DM increased, whereas the prevalence of smoking decreased with increasing BMI. An inverse correlation was noted between BMI and anemia, defined as hematocrit <39% for men and <36% for women ( Table 1 ).
| Variable | Body Mass Index (kg/m 2 ) | ||||
|---|---|---|---|---|---|
| ≤24.5 (n = 890) | 24.5–27.08 (n = 899) | 27.08–30.12 (n = 898) | >30.12 (n = 892) | p Value | |
| Body mass index (kg/m 2 ) | 23.03 (21.64, 23.88) | 25.83 (25.15, 26.42) | 28.34 (27.68, 29.18) | 32.77 (31.28, 34.99) | <0.0001 |
| Weight (kg) | 67.00 (60.00, 72.12) | 77.00 (71.00, 82.00) | 85.00 (80.00, 90.00) | 99.79 (90.00, 107.25) | <0.0001 |
| Height (cm) | 172.00 (165.00, 176.00) | 172.00 (167.00, 178.00) | 172.72 (167.00, 178.00) | 172.00 (165.00, 178.00) | 0.04 |
| Waist circumference (cm) | 88.00 (81.00, 93.00) | 95.00 (88.90, 100.00) | 101.00 (95.00, 106.00) | 110.00 (103.00, 119.00) | <0.0001 |
| Age (years) | 62.69 (52.87, 72.67) | 61.58 (53.16, 70.63) | 60.45 (52.74, 68.95) | 57.64 (51.01, 65.18) | <0.0001 |
| ≥70.0 years | 32.6% (290/890) | 26.9% (242/899) | 22.7% (204/898) | 16.1% (144/892) | <0.0001 |
| Female | 27.4% (244/890) | 22.0% (198/899) | 18.3% (164/898) | 25.9% (231/892) | <0.0001 |
| Hypertension | 43.5% (387/890) | 48.9% (439/898) | 55.1% (494/897) | 66.5% (593/892) | <0.0001 |
| Hyperlipidemia | 37.8% (336/890) | 40.2% (361/898) | 45.2% (405/897) | 49.0% (437/892) | <0.0001 |
| Current smoker | 50.3% (446/887) | 45.3% (403/889) | 45.9% (411/895) | 42.8% (380/888) | 0.0156 |
| Former smoker | 13.2% (117/887) | 18.2% (162/889) | 19.0% (170/895) | 19.4% (172/888) | 0.0016 |
| Diabetes mellitus | 11.1% (99/890) | 12.5% (112/898) | 16.2% (145/897) | 26.1% (233/892) | <0.0001 |
| Family history of premature coronary artery disease | 30.3% (270/890) | 28.4% (255/898) | 28.4% (255/897) | 30.8% (275/892) | NS |
| Peripheral vascular disease | 5.1% (45/890) | 5.6% (50/898) | 3.7% (33/896) | 3.5% (31/892) | NS |
| Thrombocytopenia | 0.1% (1/890) | 0% (0/898) | 0.3% (3/896) | 0.7% (6/892) | NS |
| Renal insufficiency | 2.4% (21/890) | 2.8% (25/898) | 3.0% (27/896) | 3.7% (33/892) | NS |
| Creatinine (mg/dL) | 0.92 (0.80, 1.10) | 0.99 (0.81, 1.14) | 1.00 (0.84, 1.12) | 1.00 (0.83, 1.16) | <0.0001 |
| Anemia | 16.2% (134/828) | 10.4% (87/840) | 8.3% (71/851) | 7.8% (66/851) | <0.0001 |
| Hemoglobin (g/dL) | 14.20 (13.20, 15.10) | 14.60 (13.60, 15.50) | 14.80 (13.70, 15.70) | 14.80 (13.80, 15.70) | <0.0001 |
| Medications | |||||
| Aspirin | 20.3% (181/890) | 23.3% (209/896) | 24.2% (217/896) | 26.6% (237/891) | 0.02 |
| Thienopyridines | 3.4% (30/890) | 2.1% (19/899) | 2.8% (25/898) | 3.1% (28/892) | NS |
| Glycoprotein IIb/IIIa inhibitor | 48.1% (428/890) | 52.0% (465/895) | 51.6% (461/893) | 51.8% (461/890) | NS |
| Heparin | 49.2% (438/890) | 46.7% (419/897) | 47.5% (425/894) | 48.2% (429/890) | NS |
| Bivalirudin | 50.4% (447/887) | 46.8% (419/895) | 48.0% (430/895) | 50.2% (445/886) | NS |
| Beta-blocker | 16.9% (150/889) | 20.5% (184/896) | 23.4% (210/896) | 25.5% (227/891) | <0.0001 |
| Calcium-channel blocker | 8.4% (75/889) | 9.7% (87/896) | 10.0% (90/896) | 13.5% (120/891) | 0.004 |
| Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker | 20.0% (178/889) | 20.6% (185/896) | 25.4% (228/896) | 29.6% (264/891) | <0.0001 |
Acute presentation metrics did not differ among quartiles (symptom onset to study hospital emergency room: 138 minutes [25th/75th interquartile range 75–245], 125 minutes [76–210], 126.5 minutes [79–215], and 130 minutes [70.5–247]). Door-to-balloon times (outside hospital or study hospital emergency department to first balloon inflation) were similar among the groups (98.5 minutes [25th/75th interquartile range 74–132], 96 minutes [72–132], 99 minutes [75–136], and 100 minutes [72–137]).
Despite presenting with ST-segment elevation, 2.4% of the patients in this study had no angiographic lesions ≥30%. Absence of CAD was most prevalent in the lowest BMI quartile and decreased in prevalence from the lowest to the highest BMI (3.3%, 3.2%, 2.0%, and 1.0%, p <0.05, for fourth quartile vs first and second quartiles). The characteristics of those with angiographic lesions ≥30% are listed in Table 2 .
| Variable | Body Mass Index (kg/m 2 ) | ||||
|---|---|---|---|---|---|
| ≤24.5 | 24.5–27.08 | 27.08–30.12 | >30.12 | p Value | |
| Plaques per patient >30% diameter stenosis | 4.31 ± 2.67 | 4.40 ± 2.75 | 4.55 ± 2.63 | 4.28 ± 2.56 | 0.0839 |
| Three-vessel disease (>30% diameter stenosis) | 48.2% (414/859) | 47.2% (404/856) | 50.1% (436/870) | 44.4% (381/858) | 0.1177 |
| Three-vessel and left main disease | 1.6% (14/859) | 2.3% (20/856) | 1.1% (10/870) | 1.5% (13/858) | 0.2709 |
| Complex plaques (>50% diameter stenosis and 2 criteria) | 75.8% (651/859) | 74.5% (638/856) | 79.0% (687/870) | 74.1% (636/858) | 0.0779 |
| Total occlusions (100% diameter stenosis) | 58.9% (506/859) | 59.1% (506/856) | 64.5% (561/870) | 65.7% (564/858) | 0.0031 |
| Total lesion length per patient | 44.60 ± 28.09 | 46.44 ± 30.36 | 47.22 ± 29.50 | 45.08 ± 29.46 | 0.2029 |
The interventional strategy did not differ among the groups. A radial approach was used in 212 patients (5.9%) and equally in the 4 quartiles (5.6%, 5.5%, 6.0%, and 6.6%). Primary PCI was performed in a similar percentage among the 4 groups (92.6%, 91.3%, 94.0%, and 93.6%, respectively), with nearly all patients who underwent coronary artery stenting (71% drug-eluting stents). In the great majority of patients, only 1 vessel was treated (95.2%, 94.9%, 96.8%, and 96.8%, respectively). The index vessel did not differ among the groups. Reference vessel diameter increased with increasing BMI and so did final minimal lumen diameter and acute gain in the stent area ( Table 3 ). Procedural complications and success rates did not differ and neither did postprocedural thrombolysis in myocardial infarction-3 flow or myocardial blush grade 3 ( Tables 3 and 4 ).
| Variable | Body Mass Index (kg/m 2 ) | ||||
|---|---|---|---|---|---|
| ≤24.5 | 24.5–27.08 | 27.08–30.12 | >30.12 | p Value | |
| Lesion characteristics | |||||
| Target lesion vessel | |||||
| Left anterior descending artery | 42.8% (430/1005) | 39.1% (382/977) | 38.6% (386/999) | 38.9% (374/962) | 0.1844 |
| Right coronary artery | 41.0% (412/1005) | 44.6% (436/977) | 44.2% (442/999) | 45.8% (441/962) | 0.1595 |
| Left circumflex artery | 15.2% (153/1005) | 15.6% (152/977) | 16.1% (161/999) | 13.9% (134/962) | 0.5828 |
| Saphenous vein graft | 1.0% (10/1005) | 0.7% (7/977) | 1.0% (10/999) | 1.4% (13/962) | 0.5814 |
| Lesion length (mm) | 16.71 ± 9.34 | 16.84 ± 10.20 | 17.24 ± 10.43 | 17.35 ± 9.58 | 0.2275 |
| Thrombus present | 68.1% (683/1003) | 70.7% (690/976) | 71.9% (718/999) | 72.5% (697/961) | 0.1390 |
| Thrombus area | 32.48 ± 23.46 | 31.18 ± 22.52 | 33.01 ± 25.14 | 34.07 ± 25.17 | 0.0458 |
| Calcium | |||||
| None | 61.9% (619/1000) | 63.7% (619/972) | 64.1% (638/996) | 69.0% (662/960) | 0.0087 |
| Moderate/severe | 38.1% (381/1000) | 36.3% (353/972) | 35.9% (358/996) | 31.0% (298/960) | 0.0087 |
| Variable | Body Mass Index (kg/m 2 ) | ||||
|---|---|---|---|---|---|
| ≤24.5 | 24.5–27.08 | 27.08–30.12 | >30.12 | p Value | |
| Number of lesions per vessel | 1.16 ± 0.40 | 1.13 ± 0.37 | 1.14 ± 0.39 | 1.13 ± 0.35 | 0.1925 |
| Number of stents per vessel | 1.40 ± 0.79 | 1.39 ± 0.76 | 1.43 ± 0.81 | 1.35 ± 0.78 | 0.1127 |
| Preprocedure | |||||
| TIMI flow | |||||
| Pre TIMI flow 0/1 | 57.6% (499/866) | 58.7% (505/861) | 63.3% (553/874) | 62.0% (530/855) | 0.0501 |
| Pre TIMI flow 2 | 13.9% (120/866) | 12.5% (108/861) | 14.4% (126/874) | 13.9% (119/855) | 0.7040 |
| Pre TIMI flow 3 | 28.5% (247/866) | 28.8% (248/861) | 22.3% (195/874) | 24.1% (206/855) | 0.0027 |
| Pre corrected TIMI frame count | 32.19 ± 20.74 | 32.36 ± 19.68 | 33.67 ± 21.91 | 33.21 ± 19.43 | 0.3503 |
| Preprocedure densitometric blush | |||||
| Blush 0/1 | 81.9% (662/808) | 84.2% (676/803) | 87.4% (719/823) | 85.0% (692/814) | 0.0236 |
| Blush 2/3 | 18.1% (146/808) | 15.8% (127/803) | 12.6% (104/823) | 15.0% (122/814) | 0.0236 |
| Post-procedure | |||||
| TIMI score | |||||
| Final TIMI flow 0/1 | 2.4% (21/864) | 3.3% (28/861) | 2.6% (23/875) | 3.6% (31/855) | 0.4354 |
| Final TIMI flow 2 | 9.4% (81/864) | 10.7% (92/861) | 10.5% (92/875) | 11.3% (97/855) | 0.6049 |
| Final TIMI flow 3 | 88.2% (762/864) | 86.1% (741/861) | 86.9% (760/875) | 85.0% (727/855) | 0.2669 |
| Final corrected TIMI frame count | 22.40 ± 14.45 | 23.60 ± 14.43 | 23.66 ± 14.16 | 24.99 ± 13.89 | <0.001 |
| Postprocedure densitometric blush | |||||
| Blush 0/1 | 24.2% (195/805) | 24.3% (195/803) | 22.7% (187/823) | 24.9% (202/810) | 0.7573 |
| Blush 2/3 | 75.8% (610/805) | 75.7% (608/803) | 77.3% (636/823) | 74.9% (607/810) | 0.7327 |
| Thrombus present | 3.6% (31/864) | 3.5% (30/861) | 2.7% (24/874) | 4.7% (40/854) | 0.1925 |
With regard to in-hospital outcomes, the quartiles did not differ in rates of CABG (2.4%, 3.2%, 2.8%, and 3.6%, respectively), re-infarction (0.9%, 1.4%, 0.9%, and 1.5%, respectively), or stroke (0.3%, 0.2%, 0.4%, and 0.8%, respectively). Major bleeding was most common in the lowest BMI quartile (8.8%, 6.8%, 5.6%, and 6.1%, respectively, p <0.05). There was a graded inverse relation between BMI quartile and in-hospital mortality, which was driven primarily by cardiac mortality ( Figure 1 ). In the adjusted analyses, this association reached borderline significance only when comparing the highest with the lowest quartile (odds ratio 0.48, 95% confidence interval 0.22 to 1.02, p = 0.055).