Patients with shoulder trauma can come to the hospital with signs and symptoms of arterial insufficiency of the upper extremity, an expanding hematoma, a pulsatile mass, signs of ongoing hemorrhage, or hemothorax. However, because of the rich collateral circulation around the shoulder joint, some patients with significant arterial injuries come to the hospital with minimal or no signs of upper extremity ischemia; they can even have palpable wrist pulses. Signs of hemorrhage can be difficult to appreciate, especially in muscular or obese patients. Therefore, one must have a high index of suspicion to make an early diagnosis of a vascular injury.
Blunt arterial trauma is less likely to result in hemodynamic instability. Patients who come to the hospital with hard signs of vascular injury such as pulsatile bleeding, expanding hematoma, palpable thrill, or evidence of peripheral ischemia should be taken to the operating room without delay. At operation, either an intraoperative angiogram or exploration of the injury is done depending on the hemodynamic stability of the patient and the surgeon’s expertise and preference. In patients without obvious signs of arterial injury, the presence of associated shoulder injuries often provides a clue regarding the presence of an underlying vascular injury. Clavicular fracture, shoulder dislocation, first rib fracture, brachial plexus injury, scapular fracture, or proximal humeral fracture increase the likelihood of an associated major arterial injury. Often, nerve root avulsion causes a devastating brachial plexus injury when the arm is forcibly hyperabducted. Additionally, compression of the brachial plexus by hematoma within the neurovascular sheath can also cause substantial neurologic impairment. In all cases, prompt exploration is indicated.
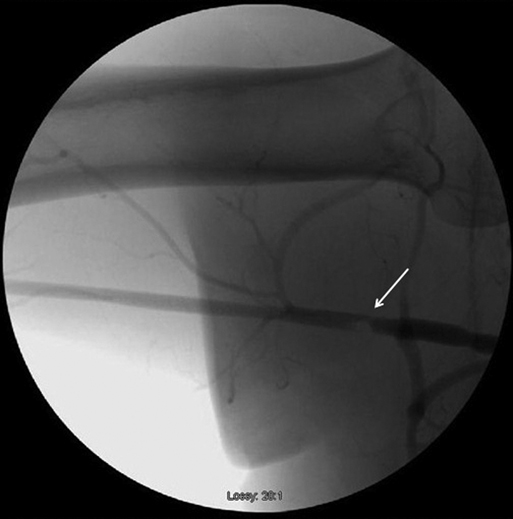
Arteriography has been the cornerstone for diagnosis of arterial injury associated with blunt shoulder trauma (Figure 1). Computed tomography (CT) angiography has largely replaced conventional arteriography for initial evaluation of arterial injuries. All patients who are hemodynamically stable and come to the hospital with signs of upper extremity arterial insufficiency should undergo an imaging study. Such is useful to plan the best operative approach, especially when a proximal subclavian artery injury is identified. A potential advantage of conventional arteriography is that after vascular access has been obtained, the surgeon may consider endovascular options to treat the identified injury.
Patients with axillary or subclavian artery injuries commonly have other concomitant injuries. Treatment priorities for the other injuries need to be established. Because of the excellent arterial collateral circulation around the shoulder, the upper extremity is often at less risk for severe ischemic sequelae. Therefore, treatment of other life-threatening injuries can and should be given priority over arterial repair. However, vascular reconstruction should not be excessively delayed.