Bilateral Pleural Effusion
Toms Franquet, MD, PhD
DIFFERENTIAL DIAGNOSIS
Common
Congestive Heart Failure
Postcardiac Injury Syndrome
Infection
Renal Disease
Metastatic Malignant Pleural Disease
Lymphoma
Trauma/Iatrogenic
Lupus Pleuritis
Abdominal Surgery
Less Common
Asbestos-related Pleural Disease
Pregnancy-related
Rare but Important
Diffuse Pulmonary Lymphangiomatosis
Venoocclusive Disease
Drug-induced Pleuritis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Congestive heart failure (CHF) leading cause of bilateral pleural effusion
Small pleural effusions are not readily identified on conventional chest radiographs
Meniscus sign on PA radiograph (> 200 mL)
Pleural effusions can be entirely overlooked on supine radiographs
Lateral decubitus chest radiograph: Useful for detecting small pleural effusions if clinically indicated
CT scans
Should be performed with contrast enhancement
No reliable distinction between exudates and transudates
Can usually differentiate between benign and malignant pleural thickening
CT criteria for differentiating pleural fluid from ascites
Interface sign: Fluid outside diaphragm is pleural; inside diaphragm, ascites
Diaphragm sign: Indistinct interface between pleural effusion and liver owing to diaphragm
Displaced-crus sign: Crus is anteriorly and laterally displaced from spine by pleural effusion
Bare-area sign: Pleural fluid may extend behind liver at level of bare area
Helpful Clues for Common Diagnoses
Congestive Heart Failure
Pulmonary venous hypertension essential for pleural fluid development
Cardiomegaly, pulmonary vascular congestion, interstitial and alveolar edema
Pleural effusion mainly derives from excess interstitial pulmonary fluid
Bilateral effusions, relatively equal size
Postcardiac Injury Syndrome
Combination of pericarditis, pleuritis, and pneumonitis after variety of myocardium and pericardium injuries
Post-myocardial infarction syndrome (Dressler syndrome)
Post-pericardiotomy syndrome: Pleuropulmonary reaction following extensive pericardiotomy
Pleural effusion (80%): Bilateral or unilateral with nearly equal frequency
Infection
Loculation suggests empyema
Large effusions suggest anaerobic, gram-negative organisms, or S. aureus
Renal Disease
Nephrotic syndrome
Due to hypoalbuminemia, hypervolemia, and increased hydrostatic pressures
Commonly subpulmonary and recurrent
Metastatic Malignant Pleural Disease
Lung, breast, ovary, and stomach
Unexplained pleural effusion in patient with malignancy
CT: Irregular pleural thickening and small nodules (implants)
Metastases may have variable enhancement
Lymphoma
Bilateral pleural effusion in 50%
Chylothorax occasionally encountered
Trauma/Iatrogenic
Hemothorax
Blunt or penetrating chest trauma
Esophageal perforation
Lupus Pleuritis
> 50% of patients with SLE will have pleural disease at some time in course of their disease
Pleural disease usually painful
Exudative pleural effusion usually small, either bilateral or unilateral
Abdominal Surgery
Small early effusions common within 3 days after surgery (70%); bilateral (63%)
Clinically not significant
Predisposing factors: Upper abdominal surgery and postoperative atelectasis
Helpful Clues for Less Common Diagnoses
Asbestos-related Pleural Disease
In approximately 3% of asbestos-exposed individuals
Unilateral or bilateral and generally of small volume (< 500 mL)
Over 50% asymptomatic
As early as 1 year after exposure (mean latency = 30 years)
May predispose to rounded atelectasis
Pregnancy-related
Antenatally and in immediate postnatal period
Normal finding on chest radiograph within 24-48 hours of delivery
Small and bilateral
Due to hypervolemia and high intrathoracic pressures from Valsalva maneuvers
Helpful Clues for Rare Diagnoses
Diffuse Pulmonary Lymphangiomatosis
Rare disease of lymphatic system affecting individuals under 20 years; progressive disease with poor prognosis
Term used when abnormalities are restricted to chest
CT: Thickening of interlobular septa, infiltration of mediastinal fat, areas of ground-glass opacity, and uni- or bilateral chylous effusions
Venoocclusive Disease
Rare cause of pulmonary hypertension affecting postcapillary (venous) pulmonary circulation
CT features: Smooth interlobular septal thickening, ground-glass opacity, and enlarged central pulmonary arteries with normal-caliber veins
Moderate to small bilateral pleural effusions
Drug-induced Pleuritis
Number of medications may cause exudative pleural effusions: Amiodarone, nitrofurantoin, phenytoin, methotrexate, cyclophosphamide, and carbamazepine
Full list at http://www.pneumotox.com
Image Gallery
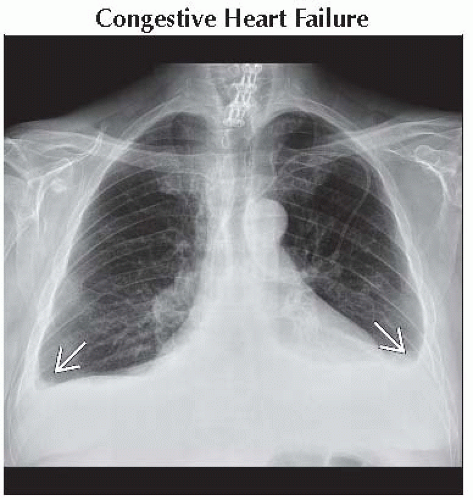 Frontal radiograph in a patient with prior myocardial infarctions and chronic CHF shows blunting of both costophrenic angles
 , representing bilateral pleural effusions. , representing bilateral pleural effusions.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|