Bilateral Hyperlucent Hemithorax
Dharshan Vummidi, MD
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Centrilobular Emphysema
Panlobular Emphysema
Bronchiectasis
Bronchiolitis
Less Common
Constrictive Bronchiolitis
Asthma
Pulmonary Langerhans Cell Histiocytosis
Lymphangiomyomatosis
Rare but Important
Pulmonary Atresia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Pulmonary causes
Usually related to airways disease
Pulmonary vascular causes much less common
Extrapulmonary causes
Congenital or developmental lack of chest wall soft tissue
Bilateral mastectomy
Technical
Overexposure
Uncommon with digital radiography
Incorrect window and level settings on CT
Helpful Clues for Common Diagnoses
Centrilobular Emphysema
Most common type of emphysema
Almost always smoking related
Predominates in upper lobes and superior segments of lower lobes
Radiography: Hyperinflation, attenuation of vessels in affected areas
CT: Centrilobular foci of low attenuation without perceptible walls
Bulla: Emphysematous space > 1 cm
Panlobular Emphysema
Most commonly associated with α-1-antitrypsin deficiency
Rarely associated with intravenous drug abuse (e.g., methylphenidate [Ritalin])
Predominates in basal portions of lungs
Radiography
Hyperinflation
Attenuation of vessels in affected areas, particularly lower lung zones
CT
Hyperinflation, particularly of lower lobes
Diffusely decreased attenuation of affected lung parenchyma with small vessels
Bronchiectasis
Hyperinflation and air-trapping from associated small airways disease
Related to chronic or recurrent infection
Rarely result of congenital cartilage abnormality (Williams-Campbell syndrome)
Radiography
Pulmonary hyperinflation
Dilated bronchi
“Tram-tracking”: Parallel lines representing nontapering walls of ectatic bronchi seen in profile
Mucoid impaction may be present
CT
Bronchial abnormalities clearly shown
Diffuse low attenuation and small vessels often present in parenchyma supplied by dilated and inflamed bronchi
Extensive air-trapping may be apparent on expiratory CT
Bronchiolitis
Usually infectious
Viral
Mycoplasma
Radiography: Hyperinflation, small lung nodules
CT: Centrilobular nodules, tree in bud opacities
Helpful Clues for Less Common Diagnoses
Constrictive Bronchiolitis
Submucosal and peribronchial fibrosis resulting in luminal narrowing or occlusion
Numerous causes
Infection: Viral (adenovirus and respiratory syncytial virus), Mycoplasma, Pneumocystis
Connective tissue diseases, especially rheumatoid arthritis and Sjögren syndrome
Drug reaction
Inhalational injury (toxic fumes, smoke)
Transplant: Lung and blood stem cell
Radiography: Normal lung volume to hyperinflation
CT: Heterogeneity of lung with smaller vessels in areas of low attenuation
Expiratory imaging confirms presence of air-trapping
Asthma
Chronic airway inflammation with remodeling
Radiography
Most patients have normal or near normal radiographs
Bronchial wall thickening may be evident
Pulmonary hyperinflation in severe cases
CT
Bronchial wall thickening
Bronchial luminal narrowing
Air-trapping (expiratory CT)
Allergic bronchopulmonary aspergillosis should be considered with central bronchiectasis and mucoid impaction
Pulmonary Langerhans Cell Histiocytosis
Nearly all patients are smokers
Radiography
Hyperinflation
Reticular or reticulonodular abnormality sparing costophrenic sulci
CT
Upper lobe predominant cysts: Vary in size and shape
Small nodules ± central lucency progressing to cysts over time
Ground-glass opacity
Spontaneous pneumothorax in < 10%
Lymphangiomyomatosis
Occurs exclusively in women of child-bearing age or patients with tuberous sclerosis
Radiography
Hyperinflation
Diffuse reticular abnormality (from superimposition of cysts)
Pleural effusion (chylous)
CT
Diffuse lung cysts ranging 2-20 mm with thin, smooth walls
Associated findings: Renal angiomyolipomas, retroperitoneal and mediastinal lymphangiomas, chylous pleural effusion
Patients may present with recurrent or chronic pneumothoraces
Helpful Clues for Rare Diagnoses
Pulmonary Atresia
Presents in neonatal period: Cyanosis
Associated with other congenital cardiac malformations (e.g., tetralogy of Fallot)
Radiography
Cardiomegaly
Concave pulmonary artery segment
Pulmonary oligemia
Diagnosis usually confirmed by echocardiography or cardiac MR
Image Gallery
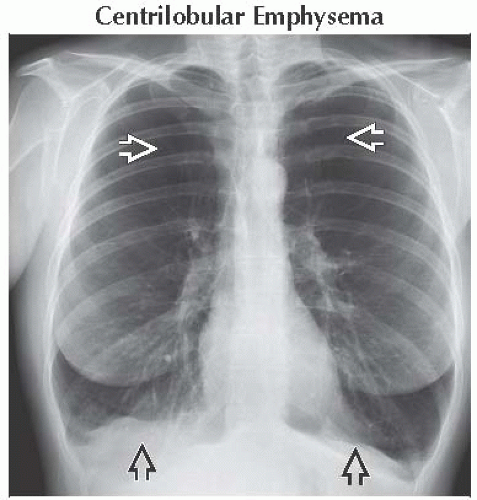 Frontal radiograph shows bilateral pulmonary hyperinflation with marked attenuation of the pulmonary vessels
 in the mid and upper lung zones. Note the depressed hemidiaphragms in the mid and upper lung zones. Note the depressed hemidiaphragms  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|