8 Bifurcation Stenosis Percutaneous Coronary Interventions
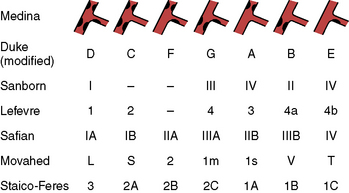
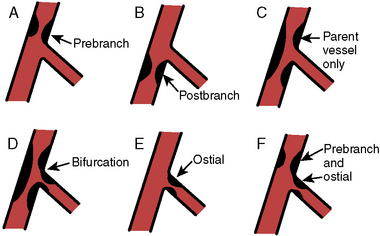
Treating bifurcation lesions involves weighing the risk of side-branch closure and the need for additional stent, sometimes requiring complex techniques. The approach to bifurcation lesions is based on the angiographic configuration of the lesion(s) in the main branch and the side branch. Significant disease (>50% stenosis) in the ostium of the side branch increases the likelihood of side-branch closure as well as the restenosis rate after percutaneous coronary intervention (PCI). Several classification schemes have been developed; these are summarized in Figure 8-1. Side branches at low risk (not likely to be compromised) include prestenosis branches, poststenosis branches, and those branches that do not straddle a stenosis. PCI across an uninvolved side branch carries a less than 1% risk of occlusion. The requirement for side-branch protection for the three side-branch locations above (prestenosis, poststenosis, not straddling a stenosis) is minimal, as the technical difficulty of approaching the target branch is also low.
Classification of Bifurcation Lesions
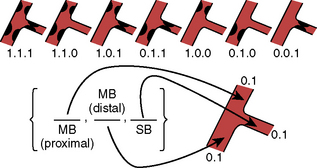
The treatment of bifurcations depends on the distribution of disease, ostial involvement, and size of branch from the parent vessel. The most commonly used classification system is the Medina (Fig. 8-2), which assigns a 0 or 1 to the presence or absence of disease in the proximal segment, distal segment, and branch vessel. The major objection to this scheme is that it does not account for angulation, which significantly contributes to procedure success rates. Another schema is depicted in Figure 8-3.
General Approach to Bifurcation Lesions
Balloon Catheter Selection and Inflation Strategies
Standard balloon catheters can be used, but different balloon sizes may be required for each branch (Table 8-1). Sequential balloon inflations or simultaneous “kissing” balloon inflations can be performed with elimination of plaque shifting being the advantage of the latter. It is important to make sure that the main vessel can accommodate both balloon diameters when performing kissing balloon inflations (proximal vessel should be at least two thirds of the combined balloon diameters). After stent placement in the main branch and the side branch, simultaneous kissing balloon inflations are critical to restore the circular and fully expanded stent to each lumen. Failure to perform final kissing balloon inflation will likely lead to restenosis.
Table 8-1 Approach to Bifurcation Stenosis
| Approach | Advantages | Disadvantages |
|---|---|---|
| Guide Catheter Selection | ||
| Two-guide catheters | Separated devices | Two artery punctures |
| Large variety of catheters | Two-catheter manipulation | |
| Long procedure time | ||
| One-guide catheter | One arterial puncture | |
| Fewer catheter manipulations, low risk of ostial trauma | ||
| Reduced procedure time | ||