Beyond the Cardiac Device: Comprehensive Care of Children and Young Adults with Implantable Cardiac Devices
Caridad M. de la Uz
Katherine Elizabeth Cutitta
Samuel F. Sears Jr.
Introduction
Futuristic television shows exclaimed optimistic taglines such as, “We have the technology,” that promise that implantable medical devices or “bionics” will fully restore health. These exciting visions have been robustly pursued within cardiology in general and in pediatric cardiology. The fundamental belief centers on innovative technologies as sufficient to achieve the ambitious idea of restored health. However, that type of conceptualization elevates the engineering marvels alone over the human factors necessary for the interpretation and utilization of benefit of the technology. The mere existence of amazing technology tends to overshadow the modern conceptualization of health outcomes that span biologic, psychological, and social health. Medical innovation is necessary, but not sufficient, to achieve comprehensive restoration of function. Psychosocial aspects of recovery have often lagged behind innovation, but the call for quality-of-life outcomes has re-ignited its centrality. Examination of patient responses and acceptance of devices have only recently emerged with regular inclusion in research and provide increased understanding of these processes.
The rapid receptivity and innovation of devices within cardiology can broadly be seen as successful. Harvey described the heart’s function as machine-like and may have inadvertently triggered the modern framework or acceptance of devices to assist the heart. Initially, medical devices are designed to address a specific medical problem without full regard to the collateral effects on the patients. Medical innovators have examined both circulatory and electrical devices to support function. Innovations with pacemakers (PMs), implantable cardioverter defibrillators (ICDs), and ventricular assist devices (VADs) have proven to be iterative, inspiring some to describe medical device innovation as a “ready, fire, aim” process (1). This realization may be considered unnerving to some people, but medical device impacts are not always fully anticipated. Pediatric indications are matched by innovations that are primarily driven by adult indications, which are then generalized down to the pediatric population. As a result, the pediatric outcomes research often trails behind the adult research. Success in device implantation creates new patient and family adjustment issues to consider, including constructs such as device acceptance, device literacy, self-management, and monitoring that were not previously needed or possible.
We suggest that medical devices are best conceptualized as safety nets for patients. The safety net is a critical feature to activities in a circus but it is not the star of the show. However, its absence could result in tragedy and change the behaviors of the performers. Pacemaker pulses, ICD shocks, and VAD output flow also represent device actions that provide a “back up” mechanism to cardiac function. Patient and family perception and behavioral responses to those processes broaden the set of potentially important outcomes for these patients.
The purposes of this chapter are to examine the past and present utilization and indications for pediatric devices (PMs, ICDs and VADs), to review research on pediatric psychosocial adjustment, and to identify strategies to improve the outcomes of pediatric patients’ device-specific adjustment and functioning.
Modern Use and Medical Indications for Device-Based Care
Interestingly, device-based care in the form of cardiac pacing had its origins in pediatrics, including the first historical accounts of the use of a pacemaker by physician, Mark C. Lidwell (1878–1968), who developed and successfully used a machine to “drive the human heart” (2). The device was used when patients under anesthesia went into cardiac arrest. In September 1929, at the Australian Medical Congress in Sydney, he reported using an earlier model to resuscitate stillborn infants when injections of epinephrine into the heart did not suffice. Following this innovation, there was no further documentation of the use of this novel device or further developments of similar technology by Lidwell. Physician-scientists, Albert S. Hyman and Paul M. Zoll, would later lay the foundation for modern day implantable cardiac devices with their work in defibrillation.
Modern use of PMs and defibrillators is remarkable. Between 1993 and 2009, approximately 2.9 million adult patients received permanent PMs with 188,700 being implanted in 2009 alone. In the same time period 0.8 million patients received implantable cardioverter-defibrillators (ICD) with an implantation rate of 46.2 per 100,000 (3,4). Pediatric implants comprise a mere 1% of the market share of this technology, but it is the associated complexities of patient selection, device implantation technique, and long-term management of implantable cardiac devices in this unique population that truly distinguish it from the adult device experience. Because of the limited population of pediatric patients and the lack of financial incentive for companies that develop these devices, innovation in pediatrics is mostly relegated to the novel adaptation of adult devices for use in children (5,6).
Indications and Utilization
Pacemakers
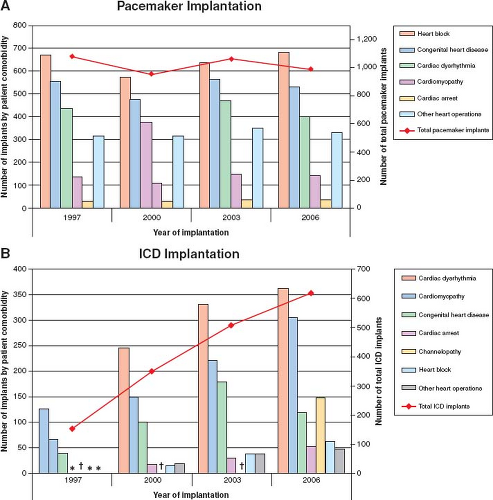
The most common indications for permanent pacemaker implantation in the pediatric population are congenital or acquired heart block, conduction system abnormalities associated with congenital
heart disease, cardiac dysrhythmias, and cardiomyopathy (Fig. 78.1) (7). Recommendations for permanent pacemaker implantation in children and patients with congenital heart disease are outlined in a distinct section of the 2008 ACC/AHA/HSR Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities and parallel the indications for pacing in the adult population (8). In a sample of hospitals from the Kids’ Inpatient Database, a large national database, there were anywhere between 951 and 1,076 PMs implanted annually during that time period with a trend toward more implants in patients over 18 years old, likely owing to the growing adult congenital population (7). These older patients survived complex heart surgeries, but may eventually develop heart failure or arrhythmias as sequelae of their disease or interventions and require implantation of some form of cardiac device. The majority of patients receiving permanent PMs in this study were between 0 and 5 years of age (43% of total) while the age groups of 5 to <12 years and 12 to <18 years were implanted with 22.1% and 24.7% of all PMs, respectively, and patients over 18 years of age made up 10.2% of all pacemaker implants. The majority of those devices were implanted at teaching hospitals (7).
heart disease, cardiac dysrhythmias, and cardiomyopathy (Fig. 78.1) (7). Recommendations for permanent pacemaker implantation in children and patients with congenital heart disease are outlined in a distinct section of the 2008 ACC/AHA/HSR Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities and parallel the indications for pacing in the adult population (8). In a sample of hospitals from the Kids’ Inpatient Database, a large national database, there were anywhere between 951 and 1,076 PMs implanted annually during that time period with a trend toward more implants in patients over 18 years old, likely owing to the growing adult congenital population (7). These older patients survived complex heart surgeries, but may eventually develop heart failure or arrhythmias as sequelae of their disease or interventions and require implantation of some form of cardiac device. The majority of patients receiving permanent PMs in this study were between 0 and 5 years of age (43% of total) while the age groups of 5 to <12 years and 12 to <18 years were implanted with 22.1% and 24.7% of all PMs, respectively, and patients over 18 years of age made up 10.2% of all pacemaker implants. The majority of those devices were implanted at teaching hospitals (7).
ICDs
In pediatric patients, the majority of ICDs are implanted for diagnoses of cardiac dysrhythmias, cardiomyopathy, congenital heart disease, and channelopathies (see Fig. 78.1), according to the database study from Czosek et al. (7). The most recent ACC/AHA/HRS recommendations for ICD implantation in pediatric patients parallel the adult criteria for secondary prevention of sudden cardiac death, but no Class I indications exist for implantation of an ICD for primary prevention in pediatric patients (5,9,10,11). Some Class I indications may be extrapolated from the adult guidelines, such as the use of an ICD in a pediatric or adult congenital patient with an EF of <30% in the setting of ischemic of nonischemic cardiomyopathy, but in pediatrics, rarer diagnoses such as the early detection of channelopathies and hypertrophic cardiomyopathy frequently call into question the need for a primary prevention ICD (5). In addition, the decision to place an ICD in a young patient requires evaluation of the risk of sudden cardiac death versus the procedural risks of implant, commitment to possible decades of therapy (with many patients outliving their devices), risk of inappropriate shocks, and risks associated with multiple potential system revisions throughout the life of the device (5,9,10,11). As the indications for ICD utilization in adults have expanded with the findings of the MADIT II study, there has been a parallel increase in the utilization of ICDs in the pediatric population. The miniaturization of the ICD and the continued development of novel implant techniques have also increased pediatric accessibility to some degree. According to Czosek et al., the utilization of ICDs increased threefold from 1997 to 2006 with approximately 130 pediatric ICDs implanted in 1997 and 396 implanted in 2006. The mean age at implant decreased from 13.6 ± 0.4 years to 12.2 ± 0.3 years in the same time period with a trend toward increased implants in children younger than 5 years of age. Despite the lower mean age and the increased utilization, complication rates associated with ICD implantation decreased from 16% to 10%. This rate, though, is still significantly higher than that associated with adult ICDs (5,9).
VADs
Common indications for VADs in a pediatric population with heart failure include postcardiotomy ventricular failure, viral myocarditis, and idiopathic and congenital cardiomyopathies (12). Indications for pediatric patients are based on a bridge to transplantation (BTT) perspective in the extant literature. Extracorporeal membrane oxygenation (ECMO) therapy is still considered the most commonly used mode of ventricular support within the United States for the
pediatric population (12), although relatively new devices, including the Berlin Heart and the Medos VAD have been used clinically, yielding positive results. The leading issues with pediatric indications for VADs include device ventricle size and ease of mobility for an active patient (13). Newer devices are increasingly equipped with a variety of left and right ventricular (RV) chamber sizes (14). Over the past decade, the use of VADs, particularly the Berlin Heart EXCOR pediatric VAD, has increased by almost 800%. Initial estimates of implant have increased from 1 implant to 86 implants in North American children from 2000 to 2012 (15). As pediatric VAD research continues to progress and technologies continue to match the need of the pediatric heart, we will likely continue to see a rise in VAD implantation.
pediatric population (12), although relatively new devices, including the Berlin Heart and the Medos VAD have been used clinically, yielding positive results. The leading issues with pediatric indications for VADs include device ventricle size and ease of mobility for an active patient (13). Newer devices are increasingly equipped with a variety of left and right ventricular (RV) chamber sizes (14). Over the past decade, the use of VADs, particularly the Berlin Heart EXCOR pediatric VAD, has increased by almost 800%. Initial estimates of implant have increased from 1 implant to 86 implants in North American children from 2000 to 2012 (15). As pediatric VAD research continues to progress and technologies continue to match the need of the pediatric heart, we will likely continue to see a rise in VAD implantation.
Review of Psychosocial Research by Cardiac Device: PMs, ICDs, and VADs
“The idea of entrusting one’s heartbeat to a small computer, a machine implanted within the body, is deeply disturbing to some people, though others are thrilled to see machines contribute in such a direct and intimate way to human well-being.” (2).
Attention to comprehensive health that spans a biopsychosocial model maintains a strong presence in pediatric medicine. The evidence for psychological distress in undermining health outcomes and quality of life across cardiac populations is increasingly evident and formidable (16). A theoretical framework for explaining the unique psychosocial issues experienced by people with implantable devices has emerged and has centered on the concept of patient acceptance. The term patient acceptance has been used in the implantable device literature to describe patients’ “perception of the device, the perception of possible discharge, changing body image, changes in lifestyle, patient and family perceptions, home going concerns, and fear of complications,” (17). It has also been defined as “a process characterized by choosing to live with technology, integrating technology into life, and living life through technology” (18). Pacemaker-specific adjustment measures have been developed (17,18,19) and were demonstrated to be more sensitive to changes in health status than widely used measures such as the SF-36 Health Survey (19). Global measures of health-related quality of life (HRQOL) such as the SF-36 or SF-12 have also been used for assessing pre- and post-implantation differences in quality of life, but may not have the specificity needed to detect subtle differences and changes in health status in device patients. Nonetheless, both disease-specific measures and global quality-of-life measures have persisted in their use, since no gold standard measure exists for all HRQOL variables. The following review focuses on the existing literature in pediatric psychosocial adjustment with cardiac devices (Table 78.1).
Pacemakers
The cardiac pacemaker transcended being an innovation and truly spawned an industry. Pediatric cardiology has benefitted from the innovation with more evidence-based treatments for arrhythmic disorders. Pacemakers operate in a markedly discrete and less dramatic manner than their ICD counterparts, but can still be associated with significant anxiety and alterations in psychosocial functioning and quality of life (20,21). Although concerns surrounding survival, body image, and need for repeated interventions
are generalizable to both adult and pediatric device patients, the impact of pacemaker or ICD implantation during the vulnerable formative periods of a child or adolescent’s development add to the psychosocial complexities of device management (22). A brief look at the stages of child development as proposed by psychologist Erik Erikson in 1968 (Table 78.2) illustrates how a diagnosis of conduction disease and the need for an implantable cardiac device at any point during childhood or adolescence could have profound effects on development (23). In particular, the ability to master one’s physical environment and develop self-esteem during early childhood may be limited by parental overprotection and physical limitations. During pre-adolescence and adolescence, though, the same physical limitations, parental overprotection and the addition of body image issues may hinder the formation of identity and diminish the sense of autonomy that is necessary to achieve separation and independence as the person moves into young adulthood (22).
are generalizable to both adult and pediatric device patients, the impact of pacemaker or ICD implantation during the vulnerable formative periods of a child or adolescent’s development add to the psychosocial complexities of device management (22). A brief look at the stages of child development as proposed by psychologist Erik Erikson in 1968 (Table 78.2) illustrates how a diagnosis of conduction disease and the need for an implantable cardiac device at any point during childhood or adolescence could have profound effects on development (23). In particular, the ability to master one’s physical environment and develop self-esteem during early childhood may be limited by parental overprotection and physical limitations. During pre-adolescence and adolescence, though, the same physical limitations, parental overprotection and the addition of body image issues may hinder the formation of identity and diminish the sense of autonomy that is necessary to achieve separation and independence as the person moves into young adulthood (22).
TABLE 78.1 Psychological Distress in Pediatric Patients with Cardiac Devices | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree