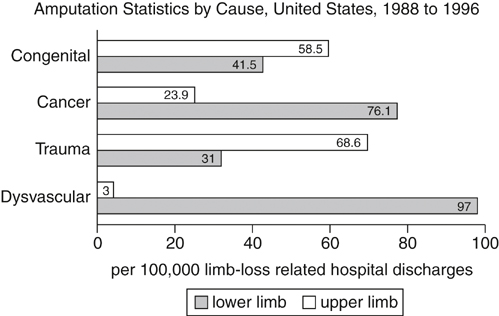
In the United States, between 1988 and 1996, an average of 133,735 hospital discharges/year were for amputations, and the predominant cause was vascular disease in 82% (Figure 1). The rate of amputations occurring in dysvascular patients increased from 38.3/100,000 people in 1988 to 46.19/100,000 people in 1996.
Below-Knee Amputation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree