Chapter 24 Bedside Surgical Procedures
A number of factors have combined to increase the frequency and appropriateness of operative procedures performed at the bedside in the intensive care unit (ICU) for critically ill surgical patients. These include the following: increasing severity of illness in critically ill surgical patients; acceptance of staged and damage control management strategies for severe abdominal, soft tissue, and orthopedic pathology; advances in endoscopic and percutaneous techniques; increasing competition for operating room (OR) space; difficulty of transporting severely critically ill patients; and resource cost of repetitive operative procedures. For abdominal procedures, in particular, the introduction of the open abdominal approach for the management of abdominal catastrophes and abdominal compartment syndrome has created the need for frequent and repetitive abdominal procedures that can safely and efficiently be done at the bedside. Also, acceptance by many surgeons of the usefulness of early tracheostomy with the introduction of percutaneous tracheostomy and endoscopically guided feeding access has resulted in a number of procedures being performed at the ICU bedside that formerly had been performed in the OR. As an example, over the 9-year period between July 2001 and December 2009, our Division of Trauma and Surgical Critical Care performed more than 13,000 bedside surgical procedures, including more than 2800 tracheostomies, 1240 gastrostomy or gastrojejunostomy tubes, 4000 bronchoscopies, and 900 laparotomies. Our monthly bedside laparotomy rate has increased from 1.9/month during 1996 to 2000 to 8.7/month during 2001 to 2009. During these two time periods, the indications for laparotomy shifted significantly from emergency indications toward the elective and semielective indications of washout or closure—27% of laparotomies were performed for elective and semielective indications during the earlier time period, which increased to 75% in the later time period.1,2
Documenting the safety and cost-effectiveness of bedside surgical procedures is made difficult by the breadth of procedures, diverse populations, and variable indications for these procedures. For the most common procedures, sufficient data support safety and cost-effectiveness. Early reports of combined analyses of common bedside procedures, including percutaneous dilational tracheostomy (PDT), percutaneous endoscopic gastrostomy (PEG) placement, inferior vena cava (IVC) filter placement, and laparotomies have demonstrated results with similar complication rates as those performed in the OR, with a significant cost reduction.3–5 Also, other reports examining PDT, PEG, and bedside laparotomy individually have also shown these procedures to be safer and more cost-effective than those performed in the OR.1,2,6–9 Bedside procedures avoid the risk and difficulties introduced by the required transport of the patient for procedures performed in the OR. Although progress has been made in regard to the safe transport of critically ill, high-risk patients, serious adverse events and death can occur.10 A small group of patients are simply not transportable because of the severity of pulmonary dysfunction or the rapidity with which the underlying process must be addressed. In this population, rapidly performed bedside procedures can be lifesaving.
Although bedside operative procedures can be performed safely, with complication rates equal to those in the OR suite, doing so mandates that cases be appropriately selected and that appropriate safety practices be consistently implemented. The ICU represents a complex environment in which to perform complex processes and procedures. Recognition of the potential for error and adverse events in these settings is important. Based on the experience of industrial safety practices and those of other organizations, prevention of error and adverse events requires standardization of processes and elimination of variability.11 Protocols and safety practices specifically for bedside operative procedures should be in place to ensure that these procedures are safely performed, with low infection rates and the assurance of comfort and anesthesia. In this chapter, we will discuss the rationale for bedside surgical procedures and the process of bringing the OR to the ICU:
Rationale for Bedside Surgical Procedures
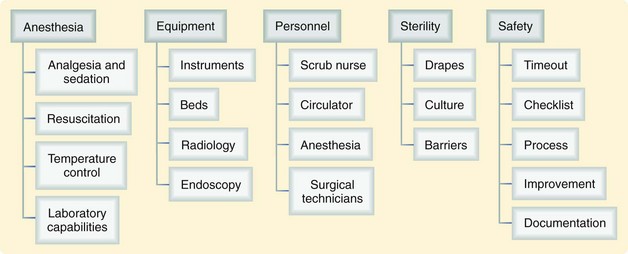
For good reasons, most surgical procedures are performed in the OR. The centralization of resources including anesthesia personnel and equipment, surgical equipment, radiology, specialized nursing and procedural support staff, and safety policies and principles make the modern surgical suite an ideal venue for most operations (Fig. 24-1). The supply of ORs, although not fixed, frequently cannot meet the demands of surgery and require significant resources to expand.
Taking the Operating Room to the Intensive Care Unit
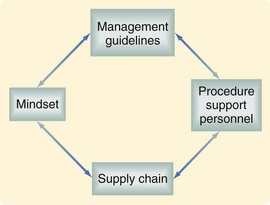
By creating and applying a well-constructed system, the major benefits of the OR can be reproduced at the bedside (Fig. 24-2). As seen in this figure, there are a number of factors required to create and maintain a successful system for performing bedside procedures. Management guidelines may include standard operating procedures, preprocedure checklists, including timeout procedures, and sedation protocols. Dedicated procedure support personnel not only decrease the variability in how an individual procedure is performed, they also play important roles in guideline compliance, both of which are significant factors in reducing error. Appropriate access to supplies may require temporary storage of core equipment in an individual ICU with standardized restocking mechanisms, thus streamlining the supply chain. Finally, a facilitative mindset among staff is vital to the success of such a system.
Safety Practices
To ensure the safety of operative procedures performed at the bedside, systematic measures should be undertaken to ensure the appropriate selection of patients and adequate expertise of support personnel, reduce procedural variability, and prevent communication errors. Implementation of the World Health Organization (WHO) “Safe Surgery Saves Lives” program has been associated with a significant global reduction in perioperative morbidity and mortality.12 Objectives outlined for procedures performed in the OR also apply to those done at the bedside. These are the 10 safety objectives outlined in the WHO guidelines13:
Management guidelines, protocols, and standard operating procedures should be in place before the routine performance of bedside operative procedures. They should be in line with those developed for the OR and be easily accessible and compliance monitored. Because of variations in specific personnel and practice patterns in various ICUs, our documents are customized to each location to ensure their appropriate application during bedside operative procedures. These documents should address issues such as the selection of appropriate cases, mandatory personnel, equipment, medications, and monitoring. An example of our bedside operative guideline is provided in Box 24-1.2 All patients should have blood pressure, electrocardiogram (ECG), pulse oximetry, and ventilation routinely monitored throughout the procedures. Adequate personnel must be present to allow performance of the procedure, monitoring of sedation and anesthesia, medication administration, manipulation of ventilation if required, and documentation. The actual number of individuals required varies, depending on procedure and that person’s expertise. Both analgesia and sedation must be ensured with appropriate medications under the direction of the critical care staff. In addition, guidelines and protocols should include standards for adequate preparation, equipment, and instrument accounting.
Box 24-1 Adapted from Vanderbilt University Medical Center, Division of Trauma & Surgical Critical Care: Emergency general surgery protocols: Bedside surgery protocol, 2005 (http://www.mc.vanderbilt.edu/surgery/trauma/Protocols/EGSBedsideSurgery.pdf).
Bedside Surgery Protocol
Indications
Decompressive celiotomy for abdominal compartment syndrome
Exploratory celiotomy for intra-abdominal hemorrhage after damage control and packing
Reexploration of a previously open abdomen for washout or closure
Protocol
ICU attending and operating surgeon will be present for the entire surgical procedure.
Informed consent obtained (if possible)
Preprocedure checklist to be reviewed by the bedside nurse
Indications to proceed to the OR (level 1):
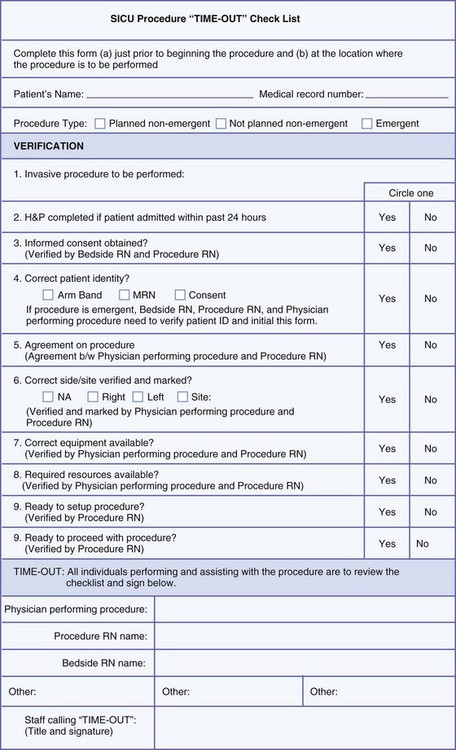
The use of preprocedure time-out and procedural checklists aids in the implementation of appropriate safety practices. Use of these tools helps limit communication errors and facilitates compliance with standard operating procedures, and can be used to assist in documentation and compliance monitoring. Again, these tools should be consistent with practices used in the OR to reduce variability, where appropriate. Figure 24-3 provides an example of a procedural checklist. Ideally, these tools can be combined with forms required for documentation and information can be captured for quality and performance analysis.