Basilar Lung Zone Disease Distribution
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Idiopathic Pulmonary Fibrosis
Nonspecific Interstitial Pneumonitis
Aspiration
Less Common
Cryptogenic Organizing Pneumonia
Asbestosis
Rare but Important
Alpha-1 Antiprotease Deficiency
Desquamative Interstitial Pneumonia
Immotile Cilia Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Tobacco abuse
Desquamative interstitial pneumonia (90% are smokers)
Alpha-1 antiprotease deficiency
Occupational exposures
Asbestosis
Desquamative interstitial pneumonia (dusts, fumes)
Helpful Clues for Common Diagnoses
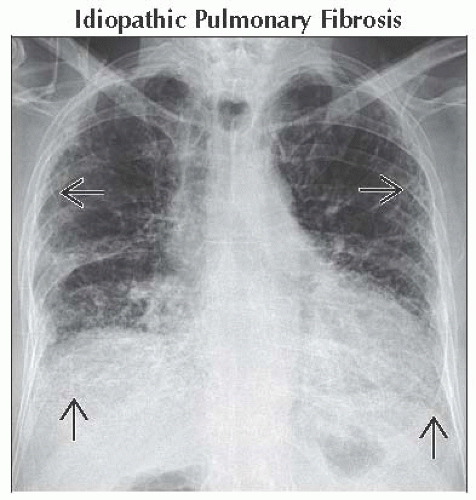
Idiopathic Pulmonary Fibrosis
Characterized histologically by usual interstitial pneumonia (UIP)
Temporal and spatial heterogeneity
Fibroblastic foci
Radiographic findings
Honeycombing
Reticulation
Traction bronchiectasis and bronchiolectasis
Architectural distortion
Subpleural and basal predominant
Nonspecific Interstitial Pneumonitis
Histological pattern of interstitial inflammation characterized by
Spatial and temporal heterogeneity
Cellular, mixed, and fibrotic forms
Most patients have collagen vascular disease (especially scleroderma, mixed connective tissue disease, and polymyositis)
Other causes of nonspecific interstitial pneumonitis (NSIP) pattern
Idiopathic (especially in young women of east Asian ethnicity)
Drug toxicity
Familial fibrosis
Hypersensitivity pneumonitis
Cigarette smoking (rare cause)
Radiographic findings
Basal predominant ground-glass opacity
Superimposed reticulation
Subpleural sparing (suggestive of diagnosis)
Traction bronchiectasis and bronchiolectasis (usually mild)
Esophageal dilation (scleroderma and mixed connective tissue disease)
Aspiration
Ranges from innocuous intake of solids or liquids into airways to extensive lung injury
Common causes
Alcohol and drug abuse
Neuromuscular disease
Loss of consciousness
Disorders of esophagus and pharynx, reflux disease
Radiographic findings
Consolidation in dependent portions of lungs, often peribronchial
May lead to lung abscess formation (cavitation with fluid level)
Associated bronchial wall thickening, endobronchial debris, centrilobular nodules, and tree-in-bud opacities
Esophageal dilation or retained debris or liquid in esophagus suggestive
Helpful Clues for Less Common Diagnoses
Cryptogenic Organizing Pneumonia
Histologic pattern defined by
Granulation tissue polyps in lumens of alveolar ducts and surrounding alveoli
Common causes of organizing pneumonia
Connective tissue disease
Drug reaction
Infection
Inhalational injury
Radiographic findings
Asbestosis
Interstitial fibrosis from asbestos exposure
Histological similar to UIP
Subpleural branching opacities (fibrosis centered on respiratory bronchioles where asbestos fibers deposited) earliest finding on CT
Honeycombing less common except in severe disease
Associated features
Parenchymal bands and subpleural curvilinear opacities
Calcified or noncalcified pleural plaques
Subpleural reticulation
Tractions bronchiectasis and bronchiolectasis
Architectural distortion
Helpful Clues for Rare Diagnoses
Alpha-1 Antiprotease Deficiency
Accounts for < 1% of patients with chronic obstructive pulmonary disease (COPD)
Homozygous deficiency (PiZZ) increases risk of COPD 30x
Cigarette smoking major contributory factor
Manifests in lungs as panlobular (panacinar) emphysema
Radiographic findings
Hyperinflation
Ill-defined absence of normal lung, wispy “cotton candy” lung markings
Homogeneous appearance
Marked basal predominance
Desquamative Interstitial Pneumonia
Histologic pattern of widespread accumulation of intraalveolar pigmented macrophages
Heavy smokers (90%)
Other causes of desquamative interstitial pneumonia-like reaction
Dust inhalation
Drug reaction
Connective tissue disease
Radiographic findings
Basal predominant ground-glass opacity (75%)
Subpleural distribution (50%)
Mild reticulation
Immotile Cilia Syndrome
Autosomal recessive disorders of ciliary structure and function
Patients predisposed to sinusitis, recurrent respiratory tract infections, bronchiectasis, and infertility
Situs abnormalities occur in up to 50%
Radiographic findings
Situs inversus or heterotaxy
Bronchiectasis (50% lower lobe predominant)
Centrilobular nodules and tree-in-bud opacities
Image Gallery
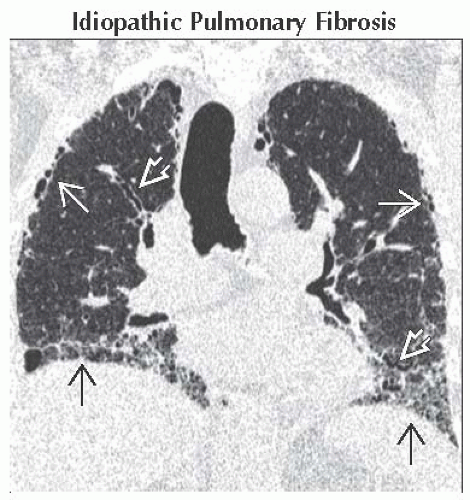 Coronal CT reconstruction shows subpleural honeycombing
 and reticulation and reticulation  with a basal and subpleural predominance. Note traction bronchiectasis with a basal and subpleural predominance. Note traction bronchiectasis  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|