AV—Access Forearm Graft
RANDALL SUNG and SETH WAITS
Presentation
A 67-year-old male with a history of end-stage renal disease (ESRD) from non–insulin-dependent diabetes mellitus presents to clinic for ongoing management of his dialysis access. He now undergoes dialysis three times per week through a temporary dialysis catheter. Two weeks ago, he underwent placement of forearm loop graft with polytetrafluoroethylene (PTFE). He is now experiencing hand stiffness, pain, and ulceration of his distal thumb on the ipsilateral hand.
Differential Diagnosis
Several etiologies should be considered for the new complaints in this patient. Although ischemic neuropathy and venous hypertension could cause pain and tissue loss in severe cases, the most likely diagnosis in this patient is arterial steal.
Several risk factors have been associated with the development of arterial steal. Diabetes is present in nearly 80% of patients with this diagnosis, and older women are at particularly high risk. Several preoperative hemodynamic parameters have been suggested to be anticipatory as well, with digital-brachial indices (DBI) of less than 0.6 and digital cuff pressures of less than 50 mm Hg being the most common. It is likely that an inability to increase arterial inflow is the precipitating cause for many patients.
Case Continued
The patient states that the symptoms started 2 days after placement of his graft. He experiences pain continuously, and his wife states that his hand is almost always cold. He had none of these symptoms prior to graft placement.
Workup
A thorough history and physical examination are the mainstay for diagnosis of arterial steal. Upon questioning, symptoms related to arterial steal may have begun early following placement of a fistula or graft. Because grafts tend to have greater flow early after placement than fistulas due to physiologic fistula maturation, symptoms of steal often occur earlier in grafts, while they may take several weeks to develop for fistulas. The patient will frequently complain of hand stiffness or pain, coolness, and tissue loss may occur in the affected extremity. On physical examination, compression of the fistula or graft will relieve ischemic-related symptoms in most patients. Additionally, some patients will demonstrate augmentation of the radial pulse distal to the takeoff of the fistula or graft.
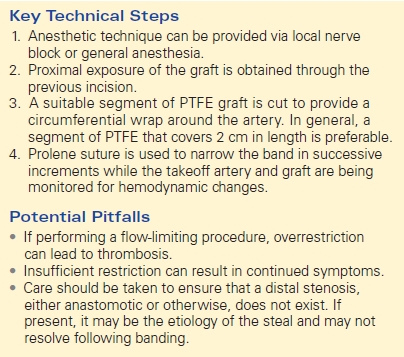
Digital-brachial index can be a reliable adjunct to history and physical examination. Measurements should normalize with occlusion of the arteriovenous (AV) fistula or graft, and a DBI of less than 0.45 is suggestive of arterial steal. Additionally, photoplethysmography (PPG) will demonstrate augmentation of monophasic or flat waveform contours that occur with arterial steal (Fig. 1).
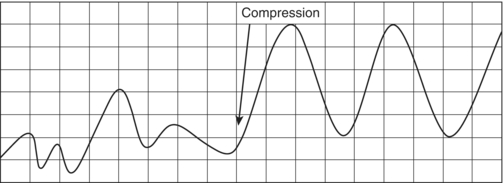
FIGURE 1 Dampened digital photoplethysmography (PPG) waveforms of a patient with radiobasilic arteriovenous fistula and arterial steal. With manual compression, the waveform returns to normal contours.
Diagnosis and Treatment
For the majority of patients without rest pain or tissue loss, watchful waiting is the mainstay of therapy. Debate exists as to the most appropriate treatment for severe cases. Ligation of the fistula or graft will provide the greatest likelihood of success. However, this approach must be balanced with the need to maintain dialysis access in these fragile patients. Losing dialysis access means that the patient must find a new site for dialysis, often a limited prospect.
Increasing resistance within the fistula or graft has been a widely used method for treatment of ischemic steal syndrome. This can be accomplished through a combination of banding, partial clipping, or lengthening of the graft. Intraoperative Doppler flow measurements can assist in titrating the flow to achieve maximal results. Loss of thrill over the fistula or graft can indicate overrestriction of blood flow and the need for intraoperative revision. Data supporting the use of restrictive procedures is mixed, with many authors believing that this procedure leads to an unacceptably high rate of thrombosis. It is the authors’ belief that when done correctly, this procedure can lead to satisfactory results.
Several other surgical options have been described in the literature. Distal revascularization with interval ligation (DRIL) bypasses the AV fistula or graft takeoff location and prevents the retrograde flow that is often associated with arterial steal. The DRIL procedure is best suited for proximal fistulas or grafts and relieves symptoms in over 80% of patients, while maintaining patency in greater than 95% of patients at 1 year. Ligation of the radial artery distal to the fistula or graft takeoff has also been reported in the literature. After assurance of ulnar collateral flow, this procedure reverses retrograde flow and provides symptomatic relief while maintaining the integrity of the AV fistula or graft.
Case Continued
Following history and physical examination, the patient is diagnosed with arterial steal related to his recent AV graft placement. He scheduled for elective banding of his fistula.
Surgical Approach
Anesthesia can be provided by regional nerve block or general anesthesia. The AV graft is accessed through an incision over the prior access point. After proximal and distal control has been obtained, options for ligation include simple suture ligation or division of the fistula or graft. The latter is generally regarded as having better outcomes in diabetic patients.
When performing flow-limiting procedures, such as banding, partial ligation, or hemoclip placement, intraoperative Doppler measurements or blood flow probes may be used. After exposure and control of the artery and fistula or graft, a self-made restrictive band is fashioned out of a piece of 6-mm PTFE. In general, a section that can sufficiently cover 2 cm (length) of AV graft circumferentially is preferable. Alternatively, the access can be narrowed with sequential ligatures spaced several millimeters apart. While intermittently monitoring the graft and distal takeoff artery with Doppler or blood flow probe, the band is placed just distal to the anastomosis and sequentially tightened to achieve maximal flow in both vessels.
In the case of proximal arm grafts or fistulas, the DRIL procedure is frequently cited as the best option for reversal of arterial steal. In the first phase of this procedure, a reversed saphenous vein graft is used to fashion an arterial bypass from the brachial artery (above the antecubital fossa) to the distal brachial artery. The second phase of the procedure involves ligation of the brachial artery proximal to the distal anastomosis. Technical precision is critical as thrombosis of the bypass graft can be limb threatening.
Endovascular approaches are gaining popularity in the treatment of arterial steal. If proximal arterial stenosis is found to be the cause of arterial steal symptoms, balloon angioplasty may correct the arterial steal. Additionally, selective stent placement can be used to cover the graft outflow if ligation is desired or stent the residual arterial stenosis (Table 1).
TABLE 1. AV-Access Forearm Graft