Atypical Adenomatous Hyperplasia, Adenocarcinoma In Situ, and Minimally Invasive Adenocarcinoma (Nonmucinous)
Fabio R. Tavora, M.D., Ph.D.
Allen P. Burke, M.D.
Marie-Christine Aubry, M.D.
Introduction
The concept of precursor lesions to adenocarcinomas of the lung has been debated since the 1960s1 and later addressed by several authors who proposed a stepwise process analogous to the adenoma-carcinoma sequence in the colon.2,3,4 Noninvasive lesions include atypical adenomatous hyperplasia (AAH), which is considered a precursor lesion but not malignant (similar to an adenoma in the gastrointestinal tract), and adenocarcinoma in situ (AIS), which is a noninvasive carcinoma with the histologic features of malignancy. A third lesion, minimally invasive adenocarcinoma (MIA), has recently been designated as a lesion composed primarily of adenocarcinoma with lepidic growth and with a degree of invasion that is insufficient to result in a significant risk for metastatic disease.
AAH, by definition, is a nonmucinous proliferation. Mucinous AIS and mucinous MIA are genetically distinct from their nonmucinous counterparts and are considered in Chapter 76. “AIS” and “MIA” when used in this chapter are presumed to denote the nonmucinous (most common) type.
Atypical Adenomatous Hyperplasia
Background
AAH is considered the precursor lesion to pulmonary adenocarcinoma based on epidemiologic, morphologic, immunohistochemical, and, more recently, molecular studies.3,5,6,7,8,9,10 The current belief clearly states a direct relationship of AAH as a precursor to well-differentiated adenocarcinomas. This concept has grown in importance in the past two decades with advances in imaging and screening protocols for patients at risk that have led to an increase in the detection of early lesions such as AAH.6,11,12,13
Radiologic Findings
AAH is found as an incidental lesion on high-resolution CT scans, often in patients with other invasive adenocarcinomas. Recent advances in radiologic techniques have helped increase detection radiologically, generally in the periphery, with a predilection to upper lobes.13 The classic radiologic description of AAH is an oval pure ground-glass
opacity without any central solid component on CT scan,14,15 which is similar to the description of AIS (formerly bronchioloalveolar carcinoma). The detection of ground-glass opacities has increased in the past 5 years, due to screening of a high-risk population, and pathologic sampling of these peripheral nodules is also on the rise.16,17 Radiologic characteristics such as sphericity, nodule size, and internal air bronchogram may be features that help distinguish between AAH and AIS.18,19,20,21
opacity without any central solid component on CT scan,14,15 which is similar to the description of AIS (formerly bronchioloalveolar carcinoma). The detection of ground-glass opacities has increased in the past 5 years, due to screening of a high-risk population, and pathologic sampling of these peripheral nodules is also on the rise.16,17 Radiologic characteristics such as sphericity, nodule size, and internal air bronchogram may be features that help distinguish between AAH and AIS.18,19,20,21
Incidence
AAH is usually found incidentally in surgical specimens of patients with lung cancer.3,20,22 Several reports have identified an incidence of AAH in specimens of lung adenocarcinomas separate from the main tumors in 5% to 20% of cases.2,19,22,23 On imaging, AAH is found up to 30% of patients with nodules of invasive adenocarcinoma.19
Gross Features
Grossly, AAH lesions are not detected, but can be appreciated as poorly defined tan or gray nodules close to the pleura. AAH has also been detected in random sections of normal lung parenchyma.24
Histologic Features
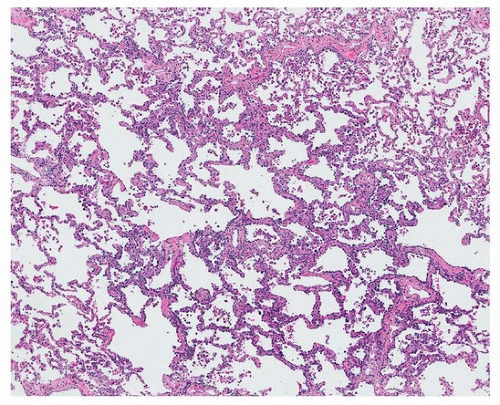
AAH is pathologically characterized by a small (<0.5 cm) proliferation of mildly atypical cells resembling type II pneumocytes or Clara cells, in a lepidic growth, spreading along the alveolar septa. The alveolar septa are mildly thickened but without loss of the normal lung architecture (Fig. 74.1). Mitoses are rare to absent. Cytologically, the cells are mildly atypical with increased nuclear size and nuclear to cytoplasmic ratio. The atypia is less pronounced than in AIS. The cell proliferation appears monotonous, and a gap is present between the cells (Fig. 74.2). Multiple lesions of AAH can be seen in the same sample of invasive tumors.
TABLE 74.1 Pathologic Characteristics of Preinvasive and Minimally Invasive Lepidic Pulmonary Lesions | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
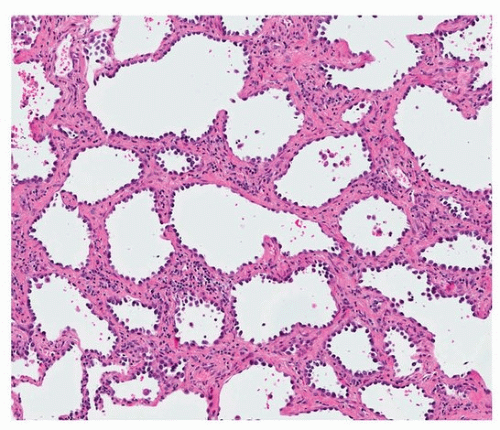 FIGURE 74.2 ▲ AAH, high power. Note cytologic features of AAH: monotonous proliferation of mildly atypical cells with thickened alveolar septa. A space is present between the nuclei.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|