(1)
Department of General surgery, Fuwai Hospital, Beijing, China
12.1 General Consideration
Atrioventricular septal defects (AVSDs) have also been called endocardial cushion defects and atrioventricular canal defects, excluding isolated ASDs and isolated VSDs.
12.2 Embryology
In common circumstances, the superior and inferior endocardial cushions grow continuously toward each other while protruding wing shaped to both sides to form the left and right nodules. They gradually join to produce the medial endocardial cushion and to divide the atrioventricular canal into two channels. The left and right nodules of the endocardium form the anterior leaflet of the MV and the septal leaflet of the TV, respectively. The main body of the endocardial cushion may be part of the septum. The malformation of the atrioventricular cushion will make the atrioventricular annulus discontinued, and the annulus of the MV will descend to the level of the septal leaflet of the TV. In those cases, the four chambers can communicate with each other.
12.2.1 Ostium Primum Atrial Septum Defect (ASD)
The inferior rim of the septum primum fuses with the endocardial cushions to close the ostium primum. The maldevelopment of the endocardial cushions or the septum primum results in an ostium primum ASD.
12.2.2 Ventricular Septum Defect (VSD)
The endocardial cushions, muscular ventricular septum, and conal septum merge to close the interventricular foramen. Abnormal development of the endocardial cushions may result in variable sizes of VSDs, which influence the membranous septum or conal septum and lead to obstruction of the LVOT.
12.2.3 Translocation of the Atrioventricular Node
The atrioventricular node and the atrioventricular bundle derive from the tissue of the primary annulus, coursing posteriorly to the endocardial cushion. As the interventricular foramen gradually diminishes, the atrioventricular bundle continues along the posterior and inferior edge of the membranous septum. When the endocardial cushions develop abnormally, the atrioventricular node and the His bundle are displaced posterior to the defect and right posterior and inferior to the entry of the coronary sinus. The left bundle branches occasionally are influenced, and particular electrocardiographic characteristics can be observed.
12.3 Classification of Atrioventricular Defects
12.3.1 Partial Atrioventricular Septal Defect
A partial AVSD is similar to the ostium primum ASD, which has no VSD and the atrioventricular valves are variably cleft. A partial AVSD differs by having a fiber connection between the MV and the septal leaflet of the TV, both of which directly attach to the ventricular septum (Fig. 12.1a–k).
12.3.2 Complete Atrioventricular Septal Defect
A complete AVSD includes an ostium primum ASD and a complete cleft that divides the atrioventricular valve into the common superior valve and the common inferior valve. The basic parts of those two common valves are not attached to the ventricular septum directly but by chordae tendineae, with the result that both leaflets float above a VSD (Figs. 12.2a–e, 12.3a–g, and 12.4a–e).
12.3.3 Transitional Atrioventricular Septal Defect
This type of AVSD is on a spectrum between the partial and the complete types, as only a small VSD exists inferior to the leaflets.
12.4 Surgical Management
A partial AVSD is similar to the ostium primum ASD. It requires closure of the interatrial communication and repair of the cleft of the MV (Fig. 12.5a–f). Surgical treatment of a complete AVSD is directed basically toward remolding the ventricular septum, raising the atrioventricular annulus back to the normal level, and closing the ostium septal ASD (Figs. 12.6a–f, 12.7a–f, 12.8a–d, 12.9a–d, 12.10a–e, 12.11a–e, 12.12a–c, 12.13a–c, 12.15a–e, 12.16a–d, 12.17a–e, and 12.18a–d).
12.4.1 Special Considerations
Operations should be performed so as to avoid damage to the conduction system in the posterior and inferior edge of the VSD and the AV anterior and superior to the VSD. The chordae tendineae are always attached to the edge of the defect, like barriers, so using a patch for repair is difficult. Because visualization is poor, measuring the size of the defect also is difficult, especially when it is not clear if a defect exists below the inferior common valve.
It is important to avoid having an obstruction of the LVOT. In the case of a huge complete AVSD, a LVOT obstruction is due partly to the conal septum being affected; the medial ventricular septum also is affected. As a result, the atrioventricular annulus descends and is concaved to the apex. Repairing only the defects without raising the atrioventricular annulus to an ordinary level may leave an important LVOT obstruction.
The MV regurgitation should be corrected. If the cleft of the MV is not accompanied by marked regurgitation, dealing with the MV may not be necessary. The coronary sinus may be used as an anatomical landmark to explore the cardiac anatomy and to locate the conduction system.
12.4.2 Technical Difficulties and Risks
12.4.2.1 Residual Mitral Valve Regurgitation
The cleft of the MV may lead to various degrees of regurgitation. The malformation of the MV and the descent of the annulus may result in a more difficult repair.
12.4.2.2 Complete Atrioventricular Block
The incidence of complete atrioventricular block is high in treating ostium primum ASDs, and it is necessary to keep a certain distance from the defect while suturing the posterior inferior rim (Fig. 12.12a).
12.4.2.3 Left Ventricle Outflow Tract Obstruction
An LVOT obstruction is due to the downward movement of the mitral annulus and may cause postoperative left-heart dysfunction.
12.5 Specimen Demonstration
12.5.1 Partial Atrioventricular Septal Defect
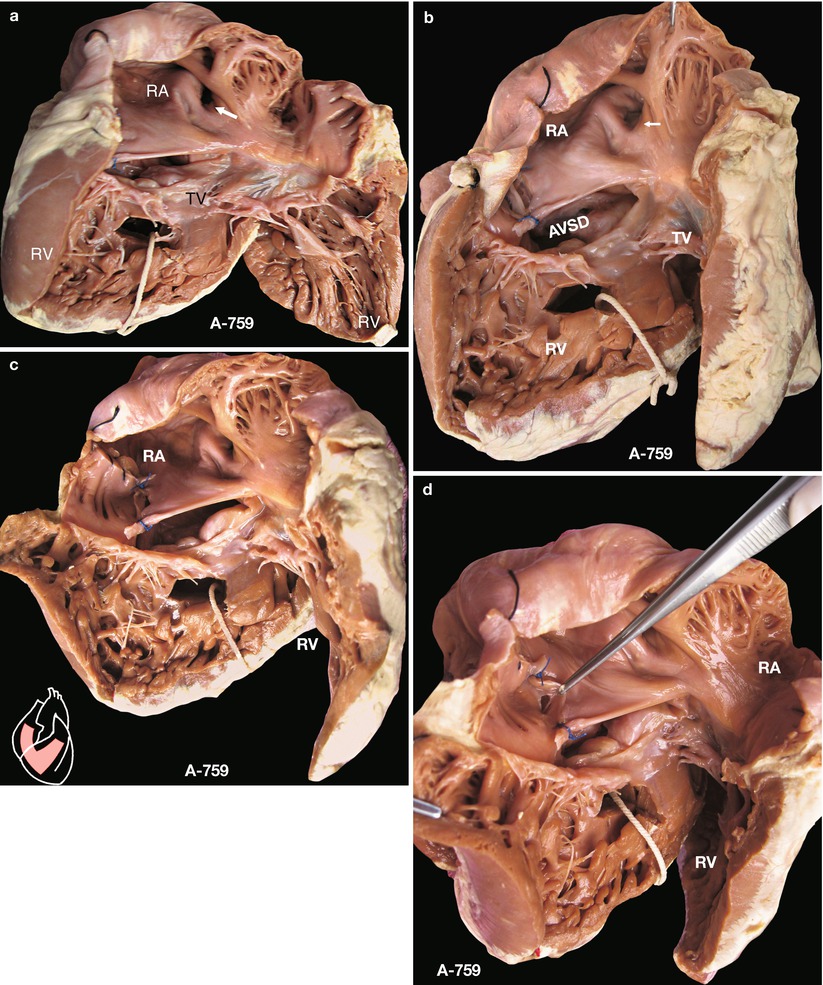
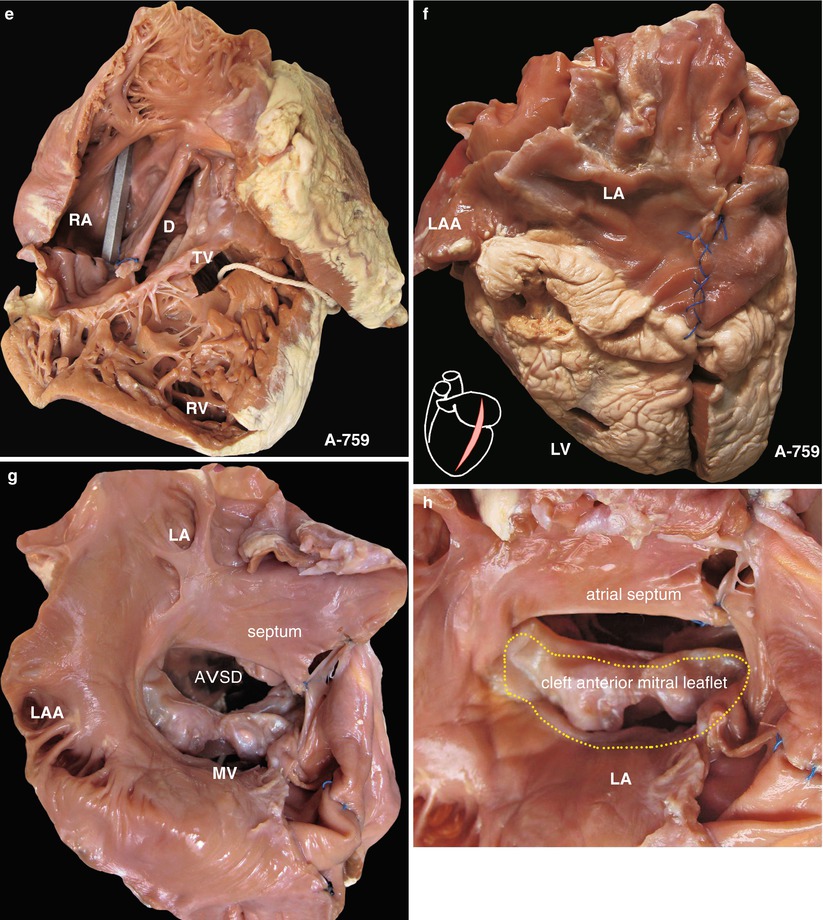
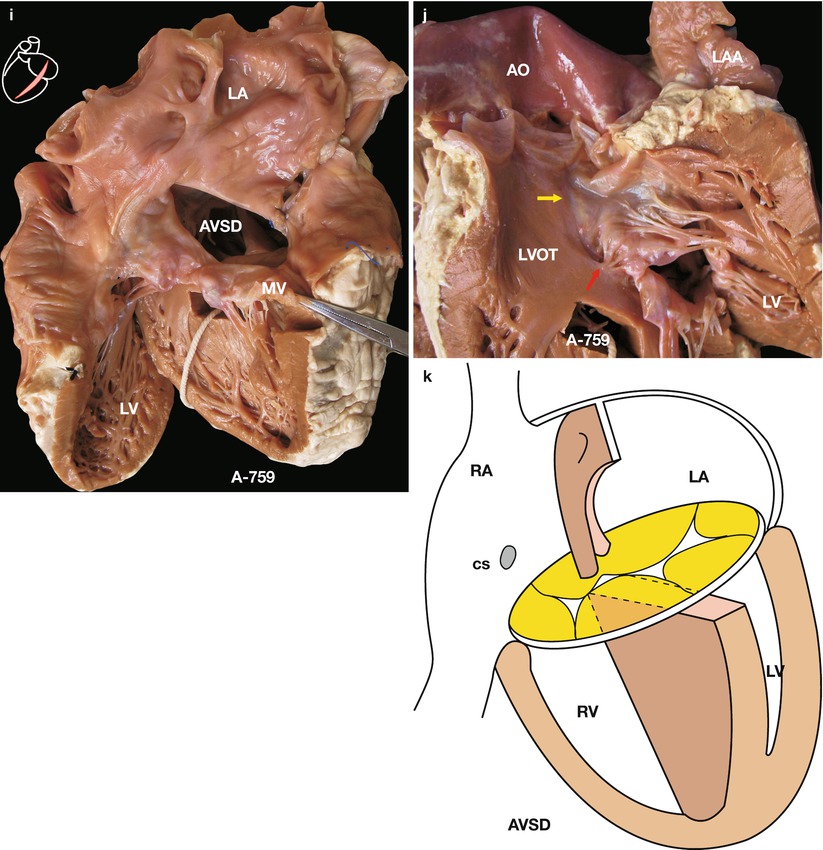
Fig. 12.1
(a) Specimen 759. Partial atrioventricular septal defect. This defect resembles an isolated ostium primum ASD, without interventricular communication. Fibrous connections exist between the mitral and tricuspid valves, and common atrioventricular valves are formed. Those characteristics may distinguish an AVSD from an ostium primum ASD. This figure is viewed from the right atrial and ventricular sides. The MV can be seen across the defect. The mitral annulus has descended to the same level as that of the TV. The white arrow marks the FO, which verifies that the defect belongs to a type of ostium primum. MV mitral valve, RA right atrium, RV right ventricle, TV tricuspid valve. (b) Specimen 759. Emphasized fossa ovalis and cleft in the tricuspid valve. This figure is typical of a partial AVSD, viewed from the RA. It is important to investigate the malformation during surgery. Common atrioventricular valves are beneath the defect. The white arrow show fossa ovalis. (c) Specimen 759. Viewed from the right atrium. Cleft in MV is seen across the defect. MV mitral valve, RA right atrium, RV right ventricle. (d) Specimen 759. Orifice of the coronary sinus viewed from the right atrium. The Thebesian valve is lifted by using forceps. The inferior edge of the defect is the tricuspid annulus. Seeing through the defect, a marked cleft in the MV is present, but coaptation is good, and there is no significant regurgitation. MV mitral valve, RA right atrium, RV right ventricle. (e) Specimen 759. Relation between partial AVSD and venae cavae. The metal bougie is put in the superior and inferior vena cavae. D partial atrioventricular defect, RA right atrium, RV right ventricle. TV tricuspid valve. (f) Specimen 759. Viewed from exterior of left heart. LA and LV are normal. LA left atrium, LV left ventricle. (g) Specimen 759. Partial AVSD viewed from the left atrial aspect. Cleft in MV can be seen. MV mitral valve. (h) Specimen 759. Overhead view of the left atrium. Dash line marks the mitral annulus. Note that the MV leaflets have connected with the contralateral TV leaflets to form a common atrioventricular valve, so this specimen is confirmed to be a case of a partial AVSD. MV mitral valve, TV tricuspid valve. (i) Specimen 759. Viewed from the left ventricular inflow tract. The MV is exposed. Mitral and tricuspid annuli are at the same level. Seen through the defect, common atrioventricular valves are formed by fusion of the left and right atrioventricular valves, and there is a cleft in the MV. MV mitral valve. (j) Specimen 759. Viewed from the left ventricular outflow tract. The MV leaflets and chordae are exposed. The yellow arrow marks a slightly inferior displacement of the mitral annulus, but there is no important LVOT obstruction. The red arrow indicates that an area of the ventricular septum is deficient, with chordae attached, and no interventricular communication is present. MV mitral valve. (k) Specimen 759. Diagram of partial atrioventricular septal defect. Diagnosis is AVSD, common atrium. A common atrioventricular valve and cleft MV are present
12.5.2 Complete Atrioventricular Septal Defect
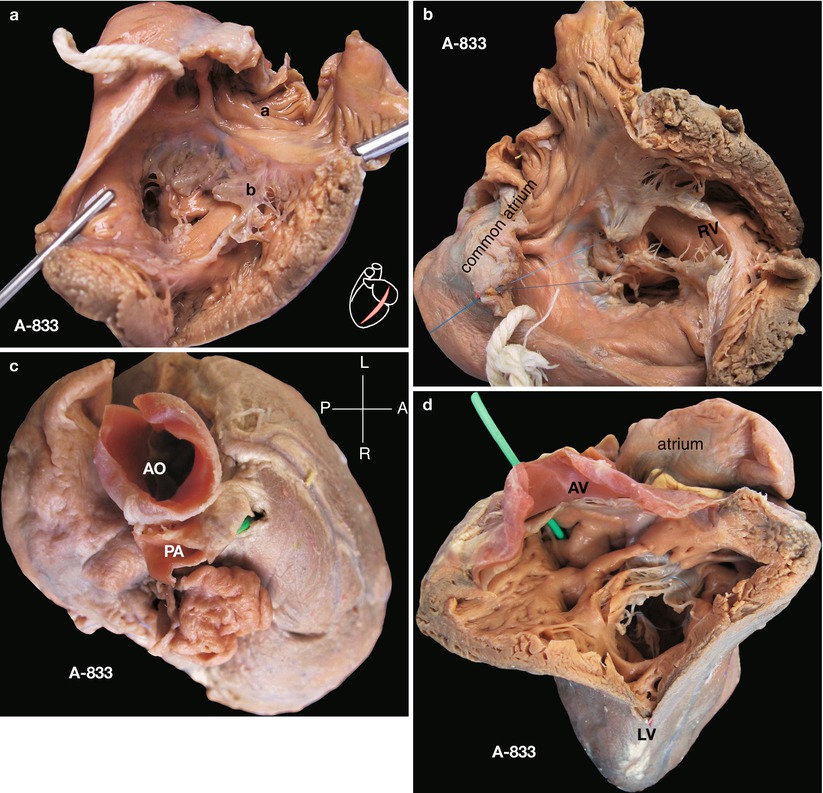
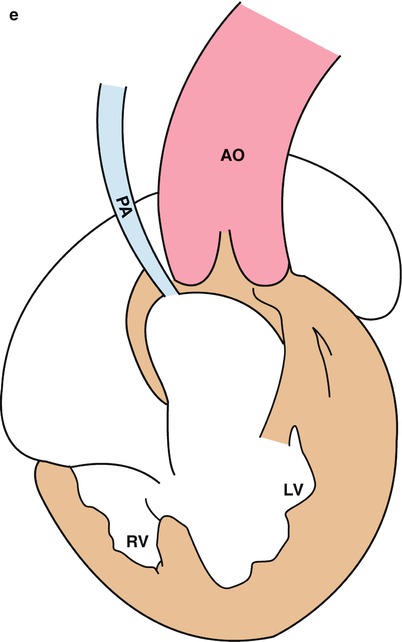
Fig. 12.2
(a) Specimen 833. Complete atrioventricular valve septal defect, common atrium, accompanied with pulmonary stenosis. Overhead view of RA and RV. No definite atrial septum is present. a: atrium, b: common atrioventricular valves. (b) Specimen 833. Ventricular structure seen beneath the common atrioventricular valves by overlooking. The RV is small, and the LV beneath the AV is large; together they function as a single ventricle. A common atrium is present due to deficiency of the atrial septum. AV aortic valve, LV left ventricle, RV right ventricle. (c) View of the heart from cephalic side. The large aorta, enormous common atrium behind the aorta, and the hypoplastic pulmonary artery, which has tiny lumen on the right of the aorta, are shown. The aorta and pulmonary artery are side by side. AO ascending aorta, PA pulmonary artery. (d) Viewed from the left ventricular outflow tract. The AV can be seen. There is a narrow fissure in the muscle below the AV, through which a bougie of 3 mm is placed. The bougie is in the pulmonary artery, resembling a functional pulmonary atresia. LV left ventricle. (e) Specimen 833. Diagram. Complete AVSD, common atrium, hypoplastic pulmonary artery, and hypoplastic RV are seen. AO ascending aorta, LV left ventricle, PA pulmonary artery, RV right ventricle
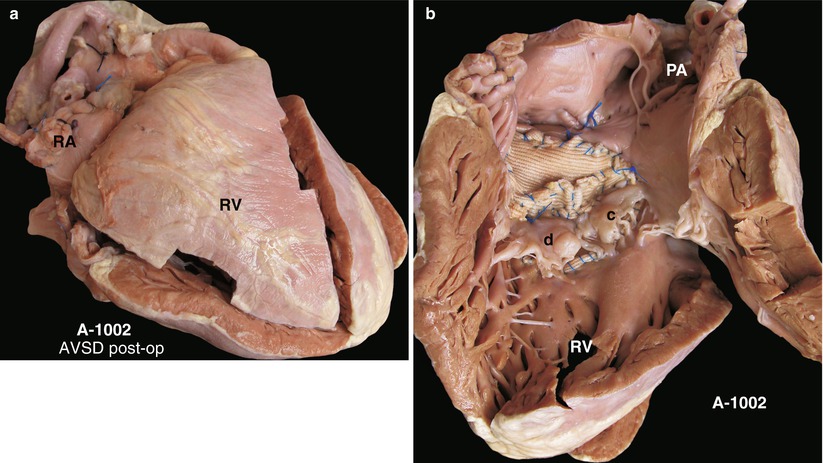
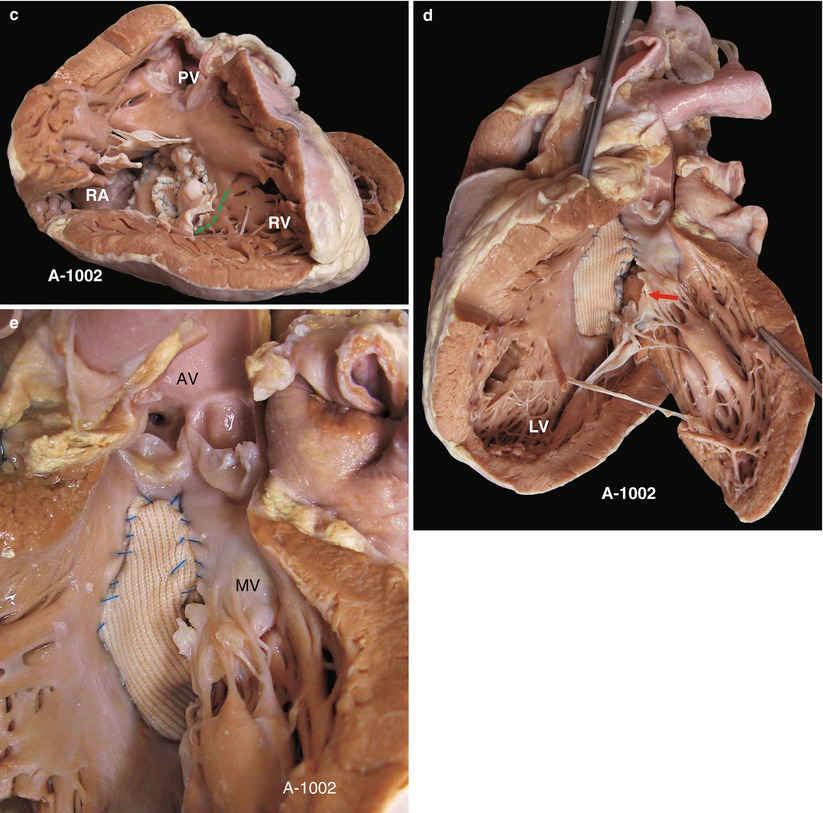
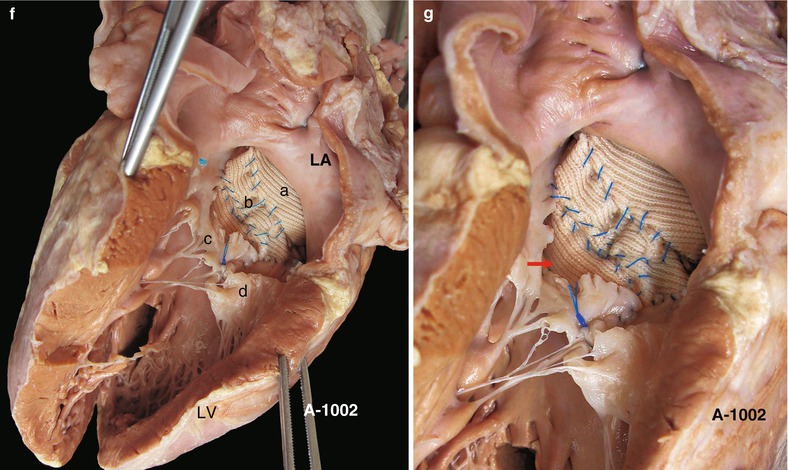
Fig. 12.3
(a) Complete atrioventricular valve septal defect (specimen 1002). External view, postoperation, is shown. RA right atrium, RV right ventricle. (b) Specimen 1002. Viewed from right ventricle outflow tract. The atrial septum and TV are exposed. The defect is repaired with a Dacron patch by using a two-patch technique. C: superior common valve, d: inferior common valve. Those two common valves are sutured together, and coaptation is good. The inferior edge of the ventricular patch can be seen under the TV. It typically is a two-patch technique that uses two Dacron patches separately to repair the ASD and the VSD. ASD atrial septal defect, TV tricuspid valve, VSD ventricular septal defect. PA pulmonary artery, RV right ventricle. (c) Same view as the previous figure. The dash line shows atrioventricular valve node and the bundle of His, which has been displaced to the posterior edge of the AVSD. PV pulmonary valve, RA right atrium, RV right ventricle. (d) Left ventricular view to observe the repair of the atrioventricular septal defect. The interventricular patch is steady and smooth, but the MV is torn apart (arrow), inducing regurgitation. LV left ventricle, MV mitral valve. (e) Close-up view from the left ventricle of the interventricular patch and the slit of the mitral valve leaflet. AV aortic valve, MV mitral valve. (f) View from left atrium and left ventricular inflow tract. The leaflet of the MV is torn apart. The atrial and ventricular portions of the patch can be seen, as can the superior and inferior common valves. a atrial portions of the patch, b ventricular portions of the patch, c superior common valves, d inferior common valves. LA left atrium, LV left ventricle, MV mitral valve. (g) Specimen 1002. Left-side view of complete atrioventricular septal defect after two-patch technique procedure. The interventricular patch and the slit of the MV leaflet of a postoperative complete AVSD treated with two-patch technique can be seen. Red arrow show the rupture of mitral leaflet. MV mitral valve
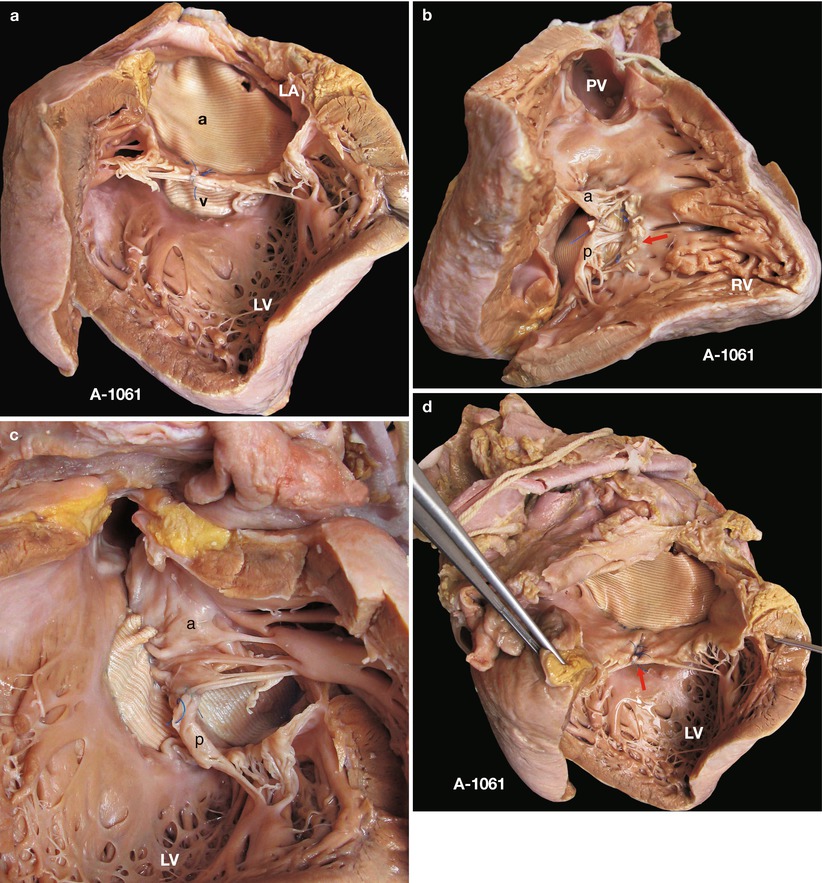
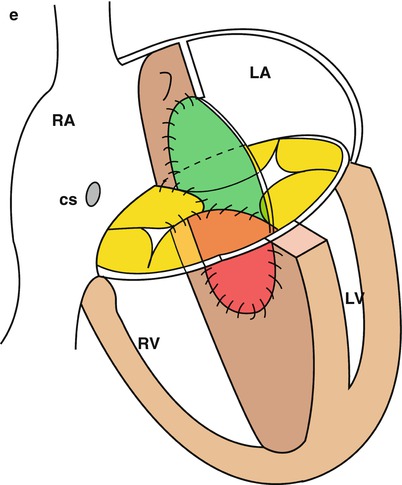
Fig. 12.4
(a) Specimen 1061. Left-side view of complete atrioventricular valve septal defect after two-patch technique procedure. The interatrial patch is superior, and the interventricular patch is inferior. Common atrioventricular valves are on the commissure of those two patches. A interatrial patch, V interventricular patch. LA left atrium, LV left ventricle. (b) Specimen 1061. View from right ventricular outflow tract. The superior common valve and inferior common valve, sutured to the atrial defect patch and the ventricular patch, respectively, are present. The arrow shows the suture line on the inferior edge of the ventricular patch. PV pulmonary valve, RV right ventricle, A Superior common valve, p inferior common valve. (c) Specimen 1061. Exposure of atrioventricular septal defect patch and common valves from left ventricular view. The patch is steady and smooth. a Superior common valve, p inferior common valve. LV left ventricle. (d) Specimen 1061. View from left atrium and left ventricular inflow tract. Only the ASD patch and the suture line of the cleft in the MV can be seen, with the VSD being covered (arrow). ASD atrial septal defect, LV left ventricle, MV mitral valve, VSD ventricular septal defect. (e) Diagram of repair of complete atrioventricular septal defect with two-patch technique. The ASD patch (green) and the VSD patch (red) are sutured together. Common valves are sewn to the attachment line of the two patches. ASD atrial septal defect, LA left atrium, LV left ventricle, RA right atrium, RV right ventricle, VSD ventricular septal defect
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


