CHAPTER
6
Atrioventricular Reciprocating Tachycardia
ARRHYTHMIAS ASSOCIATED WITH ACCESSORY PATHWAYS (APs)
○AV reciprocating/reentrant tachycardia (85%)
▪ See below.
○Supraventricular tachycardia with pre-excited QRS complexes
▪ Atrial tachycardia, atrial flutter (AFL), or atrioventricular nodal reentrant tachycardia (AVNRT)
• Electrocardiogram (ECG): Regular, wide-complex tachycardia with QRS morphology similar to pre-excitation
▪ Atrial fibrillation (5%–15%)
• ECG: Irregular, wide-complex tachycardia with variable QRS morphology (QRS morphology varies beat-to-beat depending on the degree of fusion between AP and the AV node [AVN] conduction).
ATRIOVENTRICULAR RECIPROCATING TACHYCARDIA (AVRT)
General Information
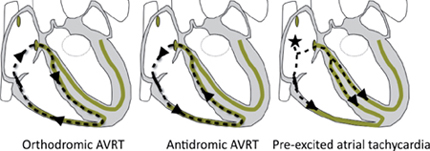
○AVRT is a paroxysmal, regular, narrow-complex tachyarrhythmia due to a macroreentrant circuit involving the atria and ventricles, which are connected via an accessory pathway (AP).
▪ During tachycardia, a long RP interval may be observed.
▪ The baseline ECG may demonstrate evidence of pre-excitation.
Epidemiology and Clinical Features
○30% of symptomatic paroxysmal supraventricular tachycardia (PSVT)
○Males predominate overall
▪ Orthodromic AVRT: Relatively more common in men
▪ Antidromic AVRT (rarer): Relatively more common in women
○Symptom onset typically in 20s (or younger)
○Palpitations, dizziness, syncope (10%)
○Rarely associated with structural heart disease
Table 6.1 Classification of AVRT
| Orthodromic (95%) | Antidromic (5%) | Pathway–Pathway | |
Anterograde conduction | AVN | AP | AP |
Retrograde conduction | AP | AVN | AP |
| |||
12-Lead ECG
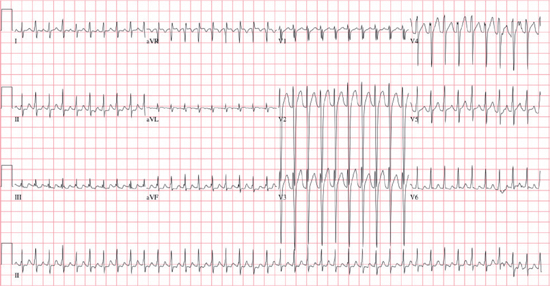
○Rate: Usually 140–250 bpm
○Rhythm: Is regular
○The P wave, PR interval, and QRS are variable.
▪ They depend on the AP location, AVN conduction time, and direction of conduction.
▪ Negative P wave in I and aVL (left-sided reentrant pathway with LA involvement)
Table 6.2 Differentiation of AVRT Mechanisms by QRS Width and RP Interval
| Orthodromic | Antidromic | Pathway-Pathway | |
QRS width | Narrow | Wide | Wide |
RP interval | Long | Short | Long |
○Onset/termination: Paroxysmal
▪ Usually preceded by an ectopic beat (atrial or ventricular)
○Other
▪ The baseline ECG may show pre-excitation (manifest APs).
▪ A sudden decrease in the tachyarrhythmia rate coincident with the development of bundle branch block (BBB) suggests that the involved bundle branch and the AP are on the same side of the heart, and are both involved in the tachyarrhythmia circuit.
Other Investigations
○ 24-hour Holter monitor
▪ Useful for diagnosis with episodes occurring more frequent than weekly
○ Event recorder
▪ Useful for diagnosis with symptomatic episodes occurring weekly to monthly
○ Echocardiogram
▪ Assessment of LV function and to exclude structural or congenital heart disease
○ Electrophysiology study (EPS): See below.
Management
Acute Management
○Narrow-complex tachycardia (orthodromic)
▪ Vagal maneuvers, adenosine, non-dihydropyridine calcium-channel blocker (preferred)
▪ B-blockers, digoxin, amiodarone (alternate)
▪ DC cardioversion (especially if unstable)
○Wide complex
▪ DC cardioversion (especially if unstable)
▪ Ibutilide, flecainide or procainamide (preferred)
• Slows conduction and/or causes block over the AP
▪ AVN targeting agents
• Effective for antidromic or orthodromic AVRT
• Ineffective with pathway-pathway AVRT and pre-excited atrial tachyarrhythmias, as the AVN is not a component of circuit
• Should be avoided in atrial fibrillation (AF) with pre-excited conduction
▪ Adenosine should be avoided.
• May precipitate AF with rapid ventricular response
Chronic Management
Table 6.3 Management of AVRT
| Poorly Tolerated AVRT | Well Tolerated AVRT | WPW with AF | Infrequent AVRT (No Pre-excitation) | Asymptomatic Pre-excitation | |
Surveillance | — | — | — | I | I |
Vagal maneuvers | — | — | — | I | — |
β-blocker | IIb | IIa | — | I (pill-in-the-pocket) | — |
ND-CCB | III | III | — | I (pill-in-the-pocket) | — |
Flecainide, propafenone | IIa | IIa | — | IIb | — |
Sotalol, amiodarone | IIa | IIa | — | IIb | — |
Ablation | I | I | I | IIa | IIa |
I: Should be performed; IIa: May be considered; IIb: Reasonable alternative; III: Not indicated.
ND-CCB: Non-dihydropyridine calcium-channel blocker.
○Non-pharmacologic therapy
▪ Vagal maneuvers
○Pharmacologic therapy
▪ Chronic daily prophylaxis is used for patients with frequent symptoms.
• Class Ic or III antiarrhythmic drugs (AADs) (preferred)
▫ Alter the conduction through the AP and the AVN via class 1c (flecainide, propafenone) and class III (sotalol, amiodarone) AADs.
▫ Alter the conduction through the AP alone (rarely used) via class Ia (quinidine, procainamide, disopyramide) AADs
▫ Note: This may result in increased arrhythmia by increasing the anterograde refractory period, thus increasing the tachycardia zone.
• β-blocker, non-dihydropyridine (ND)-calcium-channel blocker (ND-CCB), digoxin
▫ AVN agents; second-line due to their lack of direct effect on the AP
▪ The “pill-in-the-pocket” strategy is used for patients with infrequent but prolonged episodes (symptomatic but stable episodes that occur less than monthly).
• Propranolol 80 mg and/or diltiazem 120 mg > flecainide 3 mg/kg
○Invasive therapy
▪ Catheter ablation is preferred in most cases.
ATRIOVENTRICULAR REENTRANT TACHYCARDIAS
Electrophysiology Study
Baseline Intervals
○Enhanced AVN conduction (Lown-Ganong-Levine: Atrionodal, atriohisian)
▪ AH interval in sinus rhythm of ≤60 ms (normal: 80–120 ms in most subjects)
▪ Shortened atrioventricular nodal refractory times
• 1:1 conduction between atrium and His bundle are maintained during right atrial pacing at cycle lengths (CLs) below 300 ms.
▪ Abnormal responses to decremental atrial pacing
• AH prolongation ≤100 ms at the shortest 1:1 conduction when compared to the sinus rhythm value
○Manifest pre-excitation
▪ Short HV interval (<35 ms)
▪ Short local AV times: The earliest ventricular (V) EGM will be observed near the AP
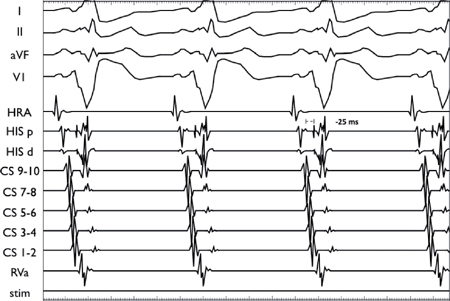
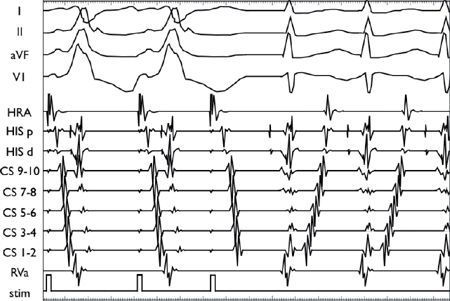
Manifest pre-excitation from a right lateral AP (HV –25 ms).
Anterograde Conduction
○Decremental atrial pacing (DAP)
▪ For manifestat or latent APs, the degree of pre-excitation depends on the anterograde conduction properties of the AP and the relationship between the AP and the AVN conduction velocities.
• Note: For concealed APs, the anterograde conduction will be via the AVN.
▪ Decremental conduction through the AVN with DAP results in AH interval prolongation with a relative shift in ventricular activation to favor the AP, which is associated with:
• Shortening in the HV interval (via AP)
• Widening of the QRS complex (increased pre-excitation)
• Note: If the AP ERP is longer than the AVN ERP, then pre-excitation disappears (long AH, normal HV and narrow QRS), and conduction continues to decrement through the AVN until the AVN ERP is reached.
• Note: If the AP ERP is shorter than AVN ERP, the AV block occurs when AP ERP is reached.
Concealed Left Lateral AP Unmasked with Rapid Atrial Pacing
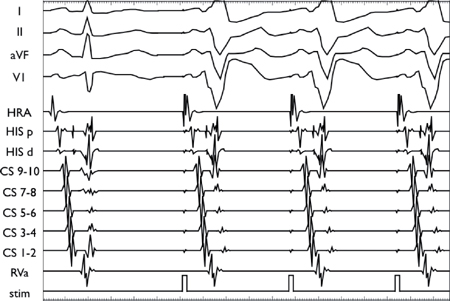
With increased atrial pacing rates, the impulse slows in the AVN (increasing AH interval), allowing increasing degrees of ventricular activation via the AP (HV shortening with manifest pre-excitation). Note the persistence of a short local AV time on the distal CS catheter, which is located near to the AP insertion.
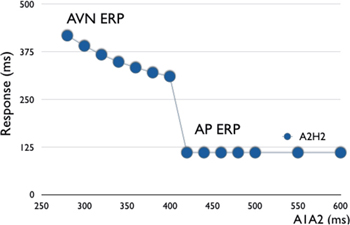
○Anterograde conduction curve
▪ Discontinuous as conduciton shifts from the AVN to AP (or vice versa)
Retrograde Conduction
○Must be present to complete the AVRT circuit
▪ If the pathway only conducts anterograde, the retrograde conduction will be via the AVN.
▪ If the pathway conducts retrograde, then retrograde conduction may be:
• Decremental via the AVN
• Non-decremental via AP
○Atrial activation sequence
▪ Generally eccentric with the earliest atrial activation at a site other than the AVN:
• Left lateral AP (55%): Distal coronary sinus (CS) → proximal CS → His bundle EGM (HBE) → high right atrial (HRA)
• Right free wall AP (10%): HRA → HBE → proximal CS → distal CS
• Posteroseptal AP (35%): Proximal CS → HBE → distal CS → HRA
▪ Can be concentric
• Anteroseptal AP (5%): Atrial insertion site is near the normal AVN exit.
▫ HBE → proximal CS → distal CS and HRA
▫ Note: AP will not display decremental conduction properties.
• Distant AP (e.g., left lateral AP with right ventricular apical pacing)
▫ Normal atrial activation occurs via the AVN before the impulse is able to conduct via the AP.
▫ Activation should shift from concentric to eccentric with decremental conduction in the AVN, ventricular pacing near the AP insertion site, or through the use of drugs that slow or block AVN conduction (e.g., adenosine, verapamil).
• Slowly conducting AP:
▫ The conduction velocity of the AP is slower than that of the AVN.
• Poorly conducting AP:
▫ The ERP of the AP occurs at a longer CL than the AVN ERP.
• Atriofascicular AP:
▫ Normal atrial activation via AVN (no retrograde AP conduction)
Tachycardia Induction
○Tachycardia can be induced with atrial or ventricular overdrive pacing or extrastimuli.
○Orthodromic AVRT
▪ Anterograde induction
• Increasingly rapid atrial pacing or extrastimuli results in AH prolongation (pre-excited QRS).
• An AP block before an AVN block allows conduction exclusively down the AVN (narrow QRS).
• If conduction is slow enough through the AVN (or with ipsilateral BBB) the AP can recover and conduct retrograde; this results in an “atrial echo” (completed loop).
• If the AVN has recovered, then the echo may conduct anterograde; doing so facilitates the induction and perpetuation of tachycardia.
▪ Retrograde induction (orthodromic)
• The same principles apply as above.
• Increasingly rapid ventricular pacing or extrastimuli result in a retrograde AVN block with continued retrograde AP conduction.
• If the AVN has recovered, then it may conduct the impulse anterograde.

○Antidromic AVRT
▪ The same principles apply as above (except reversed).
▪ Anterograde induction
• An AVN block allows conduction exclusively down the AP (wide pre-excited QRS).
• If the conduction is slow enough, the AVN can recover and conduct retrograde.
• If the AP has recovered, then the wave of depolarization may conduct anterograde down the AP.
▪ Retrograde induction
• A retrograde AP block allows conduction exclusively down the AVN.
• If conduction is slow enough, the AP can recover and conduct anterograde.
• If the AVN has recovered, then it may conduct the impulse retrograde to the atria.
▪ The initiation of macroreentry may be more difficult.
▪ Even through there is no manifest pre-excitation, the AP usually has some degree of concealed conduction. (anterograde penetration of an atrial impulse), rendering the AP refractory to retrograde conduction.
▪ To initiate macroreentry, the impulse must occur early enough so that concealed conduction into the bypass tract is blocked.
• It is facilitated by pacing near the bypass tract, which allows more time for the AP to recover.
Observations During Tachycardia
○VA relationship
▪ Obligatory 1:1 relationship (unless nodo-fascicular or nodo-ventricular AP; may have V > A)
○Long VA time (e.g., >70 ms on His bundle catheter or >100 ms on HRA catheter)
▪ Atria and ventricles are activated in series
○Atrial activation
▪ Concentric or eccentric (see above under retrograde conduction)
○Spontaneous variations in TCL
▪ Usually has a constant VA interval
▪ CL wobble is usually due to the variation in AVN conduction.
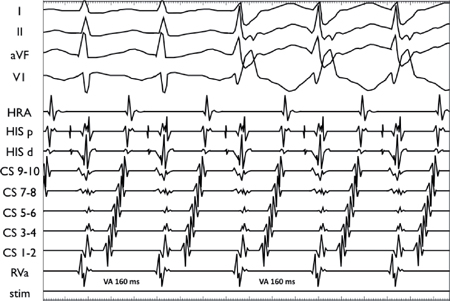
○Spontaneous BBB alters the TCL and VA timing (prolonged by ≥25 ms)
▪ Ipsilateral BBB forces conduction to pass via the contralateral bundle branch and then cross the interventricular septum before returning to the AP. This results in an increase in the TCL and VA time.
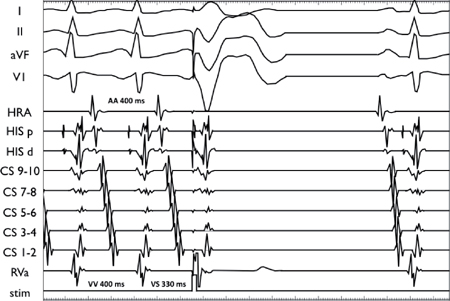
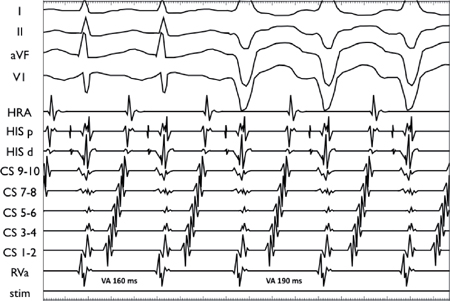
Orthodromic AVRT via a Left Lateral AP
The development of right bundle branch block (RBBB) does not affect the VA timing nor CL, indicating that the right bundle was not part of the circuit.
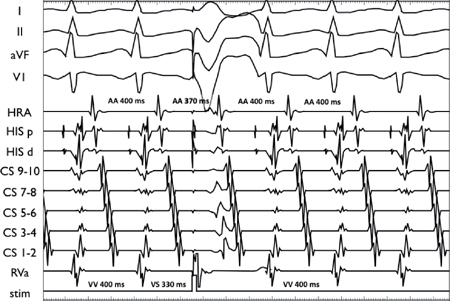
Orthodromic AVRT via a Left Lateral AP
The development of left bundle branch block (LBBB) results in a prolongation of the Tachcyardia CL and VA timing (30 ms) and CL indicating that the left bundle is part of the tachycardia circuit.
Maneuvers During Tachycardia
○Premature ventricular impulses (His-synchronous ventricular premature beat)
▪ Used to differentiate atypical AVNRT from AVRT via a septal AP.
▪ The timing of the atrial activation (A EGM) or TCL after a premature ventricular impulse timed to junctional (His) refractoriness is examined.
• For AVRT, the His synchronous VPB can advance the next atrial activation, delay the next atrial activation, terminate the tachycardia, or exert no effect.
His-synchronous premature ventricular contraction (PVC; delivered 70 ms early) advances the next A and tachycardia cycle by 30 ms (due to decrement in the AP), thus confirming the existence of an AP (but not its involvement in tachycardia).
His-synchronous PVC (delivered 70 ms early) terminates the tachycardia without conducting to the atrium. This confirms both the presence of an AP as well as its involvement in the tachycardia (the ventricle is a critical part of the circuit).
○Entrainment via ventricular overdrive pacing
▪ Used to distinguish AVRT using a paraseptal AP from AVNRT or AT
▪ VA activation should be similar during pacing and tachycardia.
▪ With termination of pacing:
• A VAV (AHV) response is observed.
• The return CL has baseline VA timing intervals (fixed coupling).
• PPI – TCL for AVRT using a septal AP (Stim to V EGM) <115 ms.
• Corrected post-pacing interval (cPPI) = (PPI – TCL) – (AHRVP – AHSVT) <110 ms
• Stim-ARVP – VASVT < 85 ms
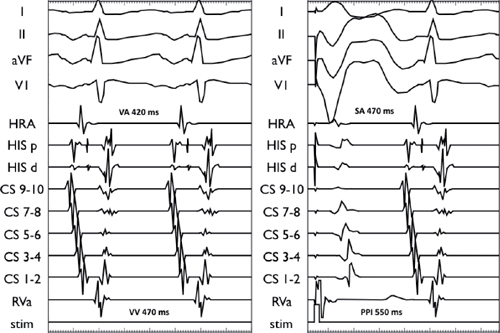
SVT entrainment via RV pacing at 440 ms (TCL 470 ms with a VA time of 420 ms: left panel). The Stim-ARVP – VASVT interval is 50 ms, and the PPI – TCL is 80 ms consistent with an ORT using a right posteroseptal AP.
VAV (AHV) Nodal Response (AVNRT, AVRT)
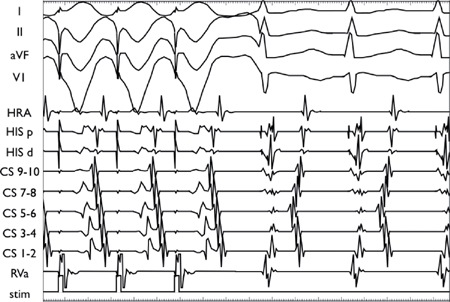
Ventricular entrainment during typical AVNRT results in 1:1 VA conduction. Post cessation of ventricular pacing, the EGM response is atrioventricular (AV).
○Entrainment via atrial overdrive pacing
▪ Used to differentiate AVRT from AT.
▪ With termination of pacing:
• The VA of the first return beat should demonstrate a fixed VA timing (<10 ms of tachycardia VA) in AVNRT and orthodromic AVRT (effectively excludes atrial or junctional tachycardia).
• Post-pacing sequence should be AHA in AVRT.
○Differential RV entrainment
▪ Entrainment at the RVa and RV base is often used to differentiate AVRT using a paraseptal decremental AP from atypical AVNRT.
▪ Interpretation:
• A [PPI – TCL (base) – PPI – TCL (apex)] <30 ms supports AVRT
• A [Stim-ARVP – VASVT (apex) – Stim-ARVP – VASVT (base)] >0 ms supports AVRT
○Parahisian entrainment
▪ Entrainment with and without His capture is often used to differentiate AVRT using a paraseptal decremental AP from atypical AVNRT.
▪
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree