CHAPTER
4
Atrioventricular Nodal Reentrant Tachycardia
UNDERSTANDING AND MANAGING ATRIOVENTRICULAR NODAL REENTRANT TACHYCARDIAS (AVNRT)
General Information
AVNRT is a paroxysmal, narrow-complex tachyarrhythmia due to reentry involving 2 functionally and anatomically distinct pathways in the vicinity of the compact atrioventricular node (AVN).
Epidemiology and Clinical Features
○AVNRT accounts for 50%–60% of symptomatic paroxysmal supraventricular tachycardias (SVT)
○Females predominate (2:1 female:male).
○Symptom onset occurs between 30 and 50 years.
○Common symptoms include palpitations (neck pulsation), dizziness, syncope (10%).
○AVNRT is rarely associated with structural heart disease.
Anatomy
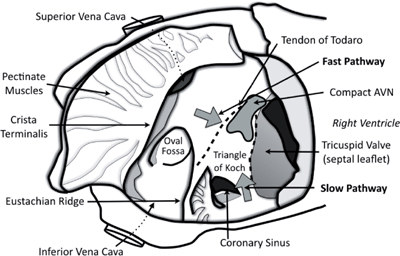
The AVN and its related structures lie along the interatrial septum in the triangle of Koch:
○The apex of the triangle is the atrioventricular (AV) component of the membranous septum containing the compact AVN and bundle of His.
○The base of the triangle is the coronary sinus (CS) ostium and the septal isthmus (tissue anteriorly from the CS os to tricuspid valve (TV) annulus).
○The posterior margin is the tendon of Todaro.
▪ A fibrous continuation of the valve of the inferior caval vein (Eustachian valve)
○The anterior margin is the septal leaflet of the tricuspid valve.
Pathophysiology (Mechanism)
Anatomic limbs of the reentrant circuit contain 2 alternative pathways.
○The fast pathway is located anteroseptal to the compact AVN at the apex of Koch’s triangle (proximal to the usual His bundle recording position, and superior to the tendon of Todaro).
▪ This pathway has the properties of rapid conduction with a long effective refractory period (ERP).
○The slow pathway is located posterior and inferior to the compact AVN (along the tricuspid annulus).
▪ This pathway has the properties of slow conduction with a short ERP.
• A late slow-pathway potential may be observed between the tricuspid valve and the CS ostium (i.e., within the septal isthmus).
▪ Rightward posterior extension of the AVN (participates in most AVNRT)
• Earliest retrograde activation is recorded between the tricuspid annulus and CS ostium.
▪ Leftward inferior extension of the AVN
• Earliest retrograde activation is recorded 2–4 cm inside the CS on the roof. Occasionally it is noted in the left atrium (LA) along the mitral annulus.
Classification
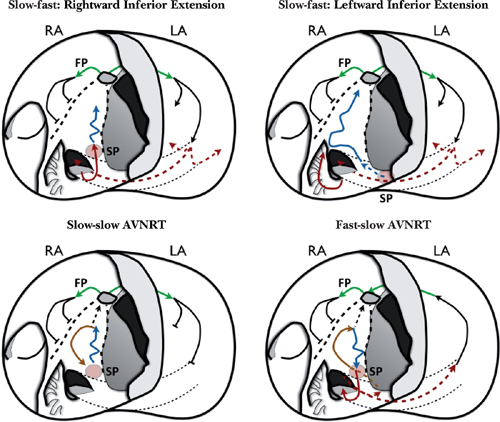
AVNRT can be divided into subtypes based on the anterograde and retrograde conduction.
○Slow-fast (or typical) AVNRT is the most common subtype (90%–95%).
▪ Retrograde conduction: The fast pathway simultaneously activates both sides of the interatrial septum.
• Right atrial activation is blocked along the Eustachian ridge.
• Left atrial activation propagates inferiorly and laterally, CS roof → CS myocardium → CS ostium
• “Rightward inferior extension” (95%)
• “Leftward inferior extension” (5%)
○Slow-slow AVNRT is often referred to as “atypical AVNRT.”
▪ Circuit has a counterclockwise “slow pathway” reentry as viewed in the right anterior oblique (RAO) projection.
▪ Retrograde conduction: Slow pathway via the leftward inferior extension with activation progressing to the CS myocardium and LA
▪ Anterograde conduction: Slow pathway via the rightward inferior extension with activation progressing to the common pathway (thus completing the circuit)
• Passive LA activation → atrial septum → fast pathway (short AH interval)
• Note: The fast pathway does not participate in the reentrant circuit.
○Fast-slow AVNRT is also referred to as “atypical AVNRT.”
▪ Circuit has a clockwise “slow pathway” reentry as viewed in the RAO projection.
▪ Slow pathway via the leftward inferior extension with activation progressing to the CS myocardium and LA.
▪ Slow pathway via the rightward inferior extension with activation progressing to the common pathway (thus completing the circuit)
• Passive LA activation → atrial septum → fast pathway (short AH interval)
• Note: The fast pathway does not participate in the reentrant circuit.
12-Lead Electrocardiogram (ECG)
Common characteristics include the following:
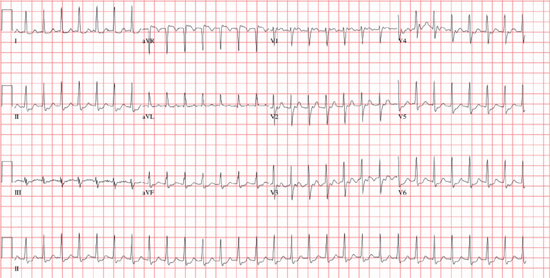
○Rate is typically 140–250 bpm, and rhythm is regular.
○In the P wave, retrograde atrial activation may not be appreciated (see Table 4.1).
Table 4.1 ECG Characteristics of AVNRT
| Typical (90%–95%) | Atypical (5%–10%) | ||
| “Slow-fast” | “Fast-slow” | “Slow-slow” | |
RP Interval* | Short | Long | Long |
P waves | 1. Absent (during QRS) 2. Late but within the QRS • pseudo r′ in V1 • pseudo S in II, III, aVF, V6 | Negative P before the QRS • pseudo q in II, III, aVF, V6 | Negative P after the QRS • pseudo S in II, III, aVF, V6 |
* The RP interval is dictated by the relative conduction velocity of the anterograde and retrograde limbs of the circuit and the HV interval.
○ QRS is narrow unless conduction is aberrant or bundle branch block is present.
○ Onset/termination is paroxysmal and initiated by an ectopic beat (atrial or ventricular).
○ Other: Baseline ECG is often normal.
Other Investigations
○ 24-hour Holter monitor
▪ Useful for diagnosis with episodes occurring more frequent than weekly
▪ Useful for diagnosis with symptomatic episodes occurring weekly to monthly
○Echocardiogram
▪ Assessment of LV function and to exclude structural or congenital heart disease
○Electrophysiology study (EPS): See below.
Management
○The condition is not life threatening but can lead to symptoms.
▪ Tachycardia-mediated cardiomyopathy may rarely occur (more often with atypical AVNRT).
○The goal of pharmacotherapy is to increase the refractory period and slow the conduction of AVN tissue.
Acute Management
○Includes the following options:
▪ Vagal maneuvers: Valsalva, cough, ice water immersion, carotid sinus massage
▪ Adenosine 6–18 mg intravenous push
▪ Non-dihydropyridine calcium-channel blocker (ND-CCB) (preferred to β-blockers [BB], digoxin, amiodarone)
▪ Direct current synchronized cardioversion (especially if unstable or signs of cardiogenic shock, angina, or heart failure)
Chronic Management
Table 4.2 Options for Chronic Management of AVNRT
| Poorly Tolerated AVNRT | Recurrent Symptomatic AVNRT | Infrequent Well-tolerated AVNRT | |
Vagal maneuvers | — | — | I |
BB, ND-CCB | IIa | I | I |
Digoxin | — | IIb | — |
Flecainide, propafenone Sotalol | IIa | IIa (BB/CCB refractory) | I (pill-in-the-pocket) |
Amiodarone | IIa | IIb | — |
Catheter ablation | I | I | I |
I: Should be performed; IIa: May be considered; IIb: Reasonable alternative; III: Not indicated.
○Nonpharmacologic therapy
▪ Vagal maneuvers to terminate an episode as needed (described above)
○Pharmacologic therapy can be dichotomized into:
▪ Chronic daily prophylaxis is used for patients with frequent symptoms.
• BB, ND-CCB, and digoxin offer similar efficacy (30%–50% efficacy).
▫ Wenckebach phenomenon in the slow pathway results in tachycardia termination.
• Class Ic or Class III anti-arrhythmic drugs are second-line options.
▫ Reserved for patients with refractory slow pathways that don’t respond to typical AVN blocking agents.
▪ “Pill-in-the-pocket” strategy is used for patients with infrequent but prolonged episodes (symptomatic but stable episodes that occur less than monthly).
• Propranolol 80 mg and/or Diltiazem 120 mg > Flecainide 3 mg/kg
○Invasive therapy
▪ Catheter ablation (slow-pathway modification) is preferred in most cases.
Electrophysiology Study (EPS)
Anterograde Conduction
○ Dual AVN physiology
▪ The presence of dual AVN physiology serves as evidence of multiple functionally and anatomically distinct conduction pathways.
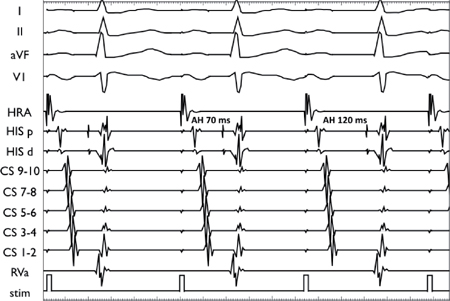
▪ AH jump: With a 10 ms decrease in the extrastimulus (A-A) coupling interval, there is a ≥50 ms increase in the AH interval.
• This occurs when the fast pathway ERP is reached and conduction switches to the slow pathway.
• At times, an AH jump may be observed during incremental atrial pacing.
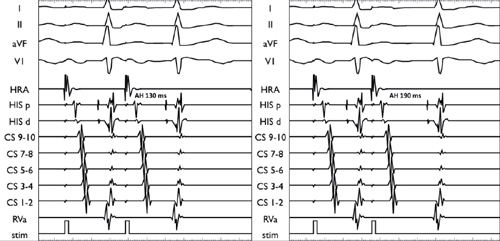
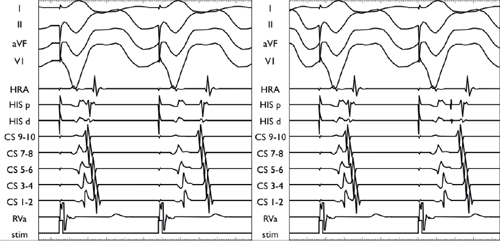
Programmed atrial stimulation. Drive train at 400 ms. In the left panel, an extrastimulus is delivered at a 260 ms coupling interval, resulting in an AH interval of 130 ms. In the right panel, the extrastimulus is delivered at a 250 ms coupling interval, resulting in an AH interval of 190 ms.
Incremental atrial pacing is performed from a high right atrial (HRA) catheter. With a 10 ms decrease in the pacing cycle length (CL), the AH interval increases from 70 ms to 120 ms.
▪ Two-for-one response: A single atrial impulse results in 2 His-ventricular depolarization
• Due to simultaneous anterograde conduction through both the fast and slow pathways
• May lead to non-reentrant dual atrioventricular nodal tachyarrhythmia, whereby a non-tachycardic atrial impulse results in tachycardia due to the presence of 2 ventricular impulses for every atrial impulse
Programmed atrial stimulation. Drive train at 400 ms. An extrastimulus is delivered at a 250 ms coupling interval, resulting in simultaneous conduction to the ventricle via the fast pathway and the slow pathway.
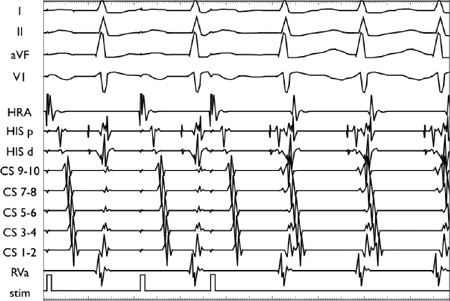
▪ Typical AVN echo is a premature atrial depolarization that conducts anterograde down the slow pathway.
• In the presence of sufficient conduction delay, the fast pathway is able to recover its excitability and conduct the impulse retrograde back to the atria, with near-simultaneous atrial (A) and ventricular (V) depolarization.
• It confirms the presence of dual AVN physiology and retrograde fast pathway conduction.
▪ Tachycardia (or echo) zone defines the range of premature beats that induce reentrant tachycardia.
• The zone is measured from the fast pathway ERP to the slow pathway ERP.
• The wider the tachycardia (or echo) zone, the more likely it is that a premature impulse will fall within that zone and induce reentrant tachycardia.
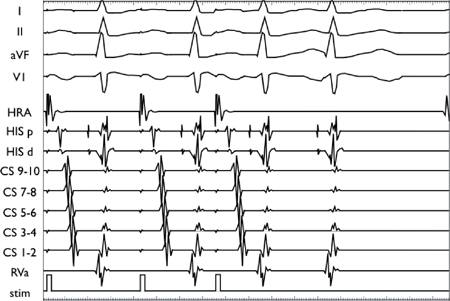
Programmed atrial stimulation. Drive train at 400 ms. An extrastimuli delivered at a 250 ms coupling interval results in an AH jump followed by a typical AVN echo beat.
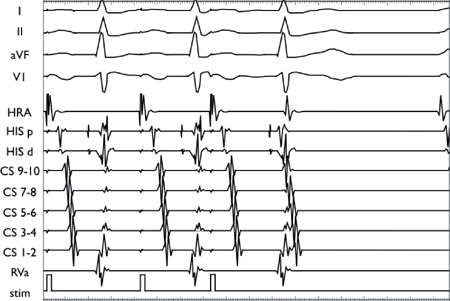
Retrograde Conduction
○VA conduction should be present and midline (concentric).
▪ Caveats:
• Retrograde conduction may not be midline with bystander accessory pathway (AP).
• Ventriculoatrial (VA) conduction will not be present in patients with retrograde block between the ventricle and lower common pathway.
○Dual retrograde AVN pathways are a less common cause of VA jump.
▪ At long coupling intervals, ventricular extrastimuli are conducted up the His-Purkinje system and exit the node via the fast pathway in the atria.
• Short VA time (<70 ms on His bundle electrogram (EGM) or <100 ms on HRA EGM)
• Earliest activation at the His bundle catheter (“concentric activation”)
▪ With progressive ventricular extrastimulus prematurity, decremental VA conduction is observed.
• In the presence of dual retrograde AVN pathways, there is a VA interval jump as retrograde fast pathway ERP is reached and conduction shifts to the slow pathway.
• As the atrial insertions of the fast and slow pathways differ, the earliest retrograde activation may shift from the His catheter (fast pathway) to the proximal CS (slow pathway).
• This shift can be followed by an “atypical” echo.
▪ Note: Infrahisian delay is the more common cause of VA jump.
• With progressive prematurity of ventricular extrastimuli, there may be a sudden increase in the VA interval due to block in the His-Purkinje system below the AVN.
• After retrograde right bundle branch block ([RBBB]; retrograde right bundle branch ERP), the impulse must travel across the interventricular septum in order to enter the conduction system via the left bundle, and subsequently travel to the His and AVN.
• This prolongation in the VH interval may reveal a retrograde His potential, which is normally hidden within the ventricular EGM.
VA jump during decremental ventricular pacing. In the left panel, the retrograde conduction “jumps” from the fast pathway to the slow pathway as the ventricular pacing CL is decreased. In the right panel, the “jump” observed is due to infrahisian delay (as manifested by a prolongation in VH time with the emergence of a retrograde His potential).
Tachycardia Induction
○Performed by rapid atrial overdrive pacing or atrial extrastimuli
▪ This results in block in the fast pathway with the impulse switching to the slow pathway.
• The delay allows retrograde conduction to occur in the fast pathway and induction of tachycardia.
▪ It may require atropine or isoproterenol infusion to facilitate induction.
AVNRT initiation during programmed atrial stimulation. Drive train at 600 ms followed by a single atrial extrastimuli at 440 ms results in AH jump and tachycardia initiation (concentric atrial activation with VA timing <70 ms).
Observations During Tachycardia
○ Short VA time (e.g., ≤70 ms on His bundle catheter or ≤100 ms on HRA catheter)
○ Concentric activation
▪ Anterior exit: Earliest activation is in the anterior septum (His catheter).
▪ Posterior exit: Earliest activation is in the posterior septum (proximal CS).
○ Spontaneous conduction block:
▪ The atria, ventricles, and bundle branches are not necessary components of the tachycardia circuit; therefore, it is possible to see spontaneous AV block (more atrial than ventricular depolarizations), spontaneous VA block (more ventricular than atrial depolarizations), and bundle branch block without any alteration in the tachycardia cycle length (TCL).
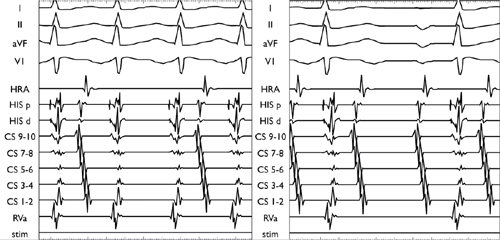
Atypical AVNRT: Anterograde conduction via the fast pathway and retrograde conduction via the slow pathway. Atrial activation is concentric with a long VA time. In the left panel, there is 2:1 upper common pathway block; each His is followed by a ventricular EGM, but only every second His is followed by an atrial EGM. In the right panel, there is 2:1 lower common pathway block; each His EGM is followed by an A EGM, but only every second His is followed by a V EGM.
Maneuvers During Tachycardia
○Late-coupled atrial extrastimuli
▪ Used to differentiate atypical AVNRT from from atrioventricular reciprocating tachycardia (AVRT) (i.e., narrow-complex tachycardia [NCT] with long VA)
▪ Two possible responses to late coupled atrial extrastimuli
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree