CHAPTER
8
Atrial Flutter and Macroreentrant Atrial Tachycardia
ATRIAL FLUTTER (AFL)
General Information
○Regular, narrow-complex tachyarrhythmia due to a macroreentrant loop in the atria
▪ Due to activation encircling a large central anatomic (valves, veins, scar) or functional obstacle
• No single point of origin
• Activation can be recorded throughout the entire cycle length (CL).
Epidemiology and Clinical Features
○Paroxysmal or persistent tachycardia with palpitations, chest pain, fatigue, dyspnea, or effort intolerance
▪ Note: If persistent rapid rates are present, then heart failure may result (tachycardia induced cardiomyopathy).
○Syncope is rare but can occur with rapid 1:1 conduction.
○“Silent” atrial tachycardia: Detected in asymptomatic patients on electrocardiogram (ECG), Holter, or implantable devices
Classification of Macroreentrant Atrial Tachycardia (MRAT)
Cavotricuspid Isthmus-Dependent MRAT
○Macroreentrant circuit confined to the right atrium (passive LA activation)
▪ Encircles the tricuspid valve (TV) with a posterior boundary (superior vena cava [SVC], inferior vena cava [IVC], and crista terminalis)
▪ Typical AFL: Counterclockwise activation
▪ Reverse-typical AFL: Clockwise activation
▪ Double-wave reentry: Two waves in the typical pathway
• Usually unstable; self-terminates or degrades into atrial fibrillation (AF)
▪ Lower loop reentry: MRAT encircling inferior vena cava with an upper turn around point is located in the posterior RA via a conduction gap in the crista terminalis.
Non-cavotricuspid Isthmus-Dependent MRAT
○Right atrial MRAT
▪ Upper loop reentry: MRAT encircling the SVC with a lower turn-around point is located at a conduction gap in the crista terminalis.
• Counterclockwise: Descending activation sequence in the free wall anterior to the crista
• Clockwise: Ascending activation sequence in the free wall anterior to the crista
▪ RA free wall flutter: MRAT encircling a low-voltage zone in the anterior free wall
▪ RA “figure-of-eight” reentry
• Type 1: Simultaneous upper and lower loop reentry share a common pathway through conduction gap in the crista terminalis. The two separate obstacles are the SVC combined with upper crista and the IVC combined with lower crista.
• Type 2: Simultaneous upper loop reentry and free wall reentry share a common pathway between the crista terminalis and the low-voltage zone. The two separate central obstacles are the SVC with upper crista and a part of the low-voltage zone.
○Left atrial MRAT
▪ Peri-mitral flutter: MRAT encircling the mitral annulus; isthmus between the mitral annulus and left inferior pulmonary vein (LIPV)
▪ Peri-venous flutter: MRAT encircling the ipsilateral pulmonary veins (PVs) via a gap between the superior PVs
▪ “Small loop” reentry: MRAT confined to a region of <3 cm; usually across two gaps in an ablation line (i.e., circumferential PV isolation)
▪ Coronary sinus (CS) macroreentry: MRAT involving the coronary sinus (CS) musculature and atrial septum
○“Lesion-related MRAT” (scar-related flutter)
▪ Post cardiac surgery: Right atriotomy, suture line, or prosthetic patch;
▪ Post surgical MAZE or percutaneous catheter ablation
12-Lead ECG
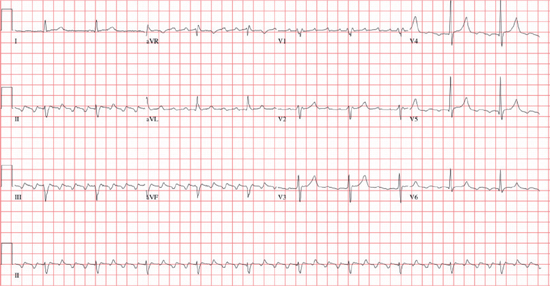
○Rate: The atrial rate is between 250 and 350 bpm.
▪ It can be slower in the presence of class 1a, 1c, III antiarrhythmics.
○ Rhythm: Ventricular conduction is variable:
▪ Regular: Usually 1:1, 2:1, or 4:1 AV association
• Odd conduction ratios (e.g., 3:1) are rare.
▪ Regularly irregular: Dual-level AV block; e.g., 6:2
▪ Irregularly irregular: Variable AV conduction may be confused with AF.
○Flutter waves
▪ Morphology depends on the location of the reentrant loop.
• Typical: Counterclockwise activation along the TV results in:
▫ Negative F waves in the inferior leads and V6; positive F wave in V1–V5
• Reverse-typical: Clockwise activation along the TV results in:
▫ Positive F waves in inferior, V6; negative F waves in V1–V5
○PR: No isoelectric PR interval
○QRS: Narrow complex unless aberrancy or bundle branch block (BBB)
○Onset/termination can be paroxysmal or non-paroxysmal
○Maneuvers: Carotid sinus massage or adenosine usually increases the degree of AV block and facilitates identification of flutter waves.
Other Investigations
○ Laboratory investigations
▪ Investigations into underlying cause (see Etiology)
○ 24-hour Holter monitor
▪ Useful for diagnosis with episodes occurring more frequent than weekly
○ Event recorder
▪ Useful for diagnosis with symptomatic episodes occurring weekly to monthly
○ Echocardiogram
▪ Assessment of LV function and to exclude structural or congenital heart disease
▪ Electrophysiology study (EPS): See below.
Management
Acute Management
Table 8.1 Management of AFL or MRAT
| Not Tolerated | Stable – Conversion | Stable – Rate Control | |
BB/ND-CCB | IIa | — | I |
Digoxin | IIb | — | IIb |
Ibutilide | — | IIa (38%–76% success) | — |
Amiodarone | IIb | IIb | IIb |
Class Ic: Flecainide, procainamide Class Ia: Propafenone Class III: Sotalol | — | IIb (<40% success) | — |
DC cardioversion | I | I (>95% success) | — |
Pacing (atrial/esophageal) | — | I (80% success) | — |
I: Should be performed; IIa: May be considered; IIb: Reasonable alternative; III: Not indicated.
BB, β-blockers; ND-CCB, non-dihydropyridine calcium-channel blockers.
○Rate control
▪ Difficult to achieve
▪ β-blockers or non-dihydropyridine calcium-channel blockers (ND-CCB) are preferred
▪ Digoxin or amiodarone are second line
○Cardioversion
▪ Medical: Ibutilide, procainamide, sotalol, amiodarone, quinidine
• A β-blocker or ND-CCB (diltiazem or verapamil) should be given before administering a class I AAD (i.e., procainamide, propafenone, flecainide), because these agents have can potentially slow the atrial rate, resulting in rapid conduction across the AV node (AVN) (e.g., paradoxical increase in the ventricular rate).
▪ Electrical: DC shock at low synchronized energy levels (30–50 J) terminates the reentrant circuit, inducing uniform refractoriness.
▪ Overdrive pacing: Pace the atrium from atrial or esophageal leads at a rate > than flutter can terminate the circuit.
Chronic Management
○Anticoagulation
▪ See AF section.
○Pharmacologic therapy
▪ Rate control: β-blocker, verapamil/diltiazem, digoxin
▪ Rhythm control: Dofetilide preferred to other antiarrhythmic drugs (AADs).
Table 8.2 Chronic Management of AFL or MRAT
| First Episode Tolerated | Recurrent Tolerated | Poorly Tolerated | After AAD for AF | Non-CTI Failed AAD | |
Cardioversion alone | I | — | — | — | — |
Dofetilide | — | IIa (>70% 1y success) | — | — | — |
Antiarrhythmic drugs – Class III, class Ic, class Ia | — | IIb (~50% 1y success) | — | — | — |
Catheter ablation | IIa | I | I | I | IIa |
I: Should be performed; IIa: May be considered; IIb: Reasonable alternative; III: Not indicated.
○Invasive therapy
▪ Catheter ablation: Preferred over AADs
CATHETER ABLATION OF MACROREENTRANT ATRIAL TACHYCARDIA (MRAT)
Indication
○AFL or MRAT that is symptomatic, recurrent, or refractory to medical therapy (class I indication).
Anticipated Success
○ Cavotricuspid isthmus (CTI)-dependent flutter: >95% acute success; 5%–10% redo rate
▪ 30% will go on to develop AF after AFL ablation (compared to >50% with AFL not undergoing CTI ablation)
○ Non-CTI-dependent flutter: 50%–88% chronic success rate
○ Co-existing AF and AFL: Arrhythmia-free survival depends on the dominant rhythm.
▪ Predominantly AFL: 60% free of both AF and AFL
▪ Predominantly AF: 25–30% free of both AF and AFL
Anticipated Complications
○Similar to all invasive ablation procedures
○<0.5% risk of AV block (particularly with ablation near the septum, due to damage to the AV nodal artery.
Patient Preparation
○
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


