Chapter 30
Atherosclerotic Risk Factors
Hypertension
Geoffrey O. Ouma, Emile R. Mohler III,
Based on a chapter in the seventh edition by Stephanie S. DeLoach and Emile Mohler III
Hypertension plays an important role in the pathogenesis of atherosclerosis and is a major risk factor for peripheral artery disease (PAD). However, the available evidence related to PAD and hypertension is mostly extrapolated from subgroup analyses of larger trials of patients with atherosclerotic vascular disease and cardiovascular risk factors. As a result, there are no current concrete within-class comparison studies of the effects of hypertension treatment on PAD-related outcomes. Although no prospective, randomized trial data have demonstrated that antihypertensive therapy alters the course of PAD, nonetheless patients with PAD have high mortality from cardiovascular disease and cerebrovascular disease, and consequently treatment of hypertension is recommended in this population. This chapter addresses the epidemiology, diagnosis, pathogenesis, and management of hypertension as it relates to PAD.
Epidemiology
Scope of the Problem
Hypertension is a prevalent disease in the United States. The National Health and Nutrition Examination Survey (NHANES, 2009-2010) estimates that 64 million or 28.6% of adults older than 18 years in the United States have hypertension.1 In this survey, hypertension was defined as systolic blood pressure (SBP) higher than 140 mm Hg, diastolic blood pressure (DBP) higher than 90 mm Hg, or individuals taking antihypertensive medication. Therefore, the prevalence of hypertension is increasing, with only 24% affected according to the survey conducted in the previous decade (1988-1991; 1999-2000) (Fig. 30-1).2,3 This increase in prevalence of hypertension in the United States is attributed to increasing age of the population as a whole2 and growing rates of obesity.4,5
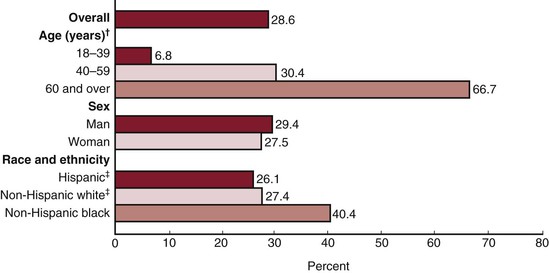
Figure 30-1 Age-specific and age-adjusted prevalence of hypertension among adults aged 18 years and older, United States, 2009-2010. †Significant linear trend. ‡Significantly different from non-Hispanic black persons. (From Centers for Disease Control and Prevention/National Center for Health Statistics, National Health and Nutrition Examination Survey: Hypertension among adults in the United States, 2009-2010. Available at: www.cdc.gov/nchs/data/databriefs/db107.htm.)
The prevalence of hypertension increases with age; 7% of adults between the ages of 18 and 39 years are affected compared with 67% of those 60 years and older.1 The prevalence of hypertension varies by other demographics as well. Hypertension is slightly more prevalent among women compared with men (29% vs 27%).1 Among the different ethnic and racial groups in the United States, blacks have the highest prevalence of hypertension.1,2,5 Similarly, PAD, as manifested by clinical symptoms and ankle-brachial index (ABI), is more common in older blacks compared with whites.6 Data from the NHANES found that PAD is also more common in blacks and Mexican Americans compared with whites.7
Both elevated SBP and DBP are associated with increased cardiovascular risk. The relative predictive value of SBP versus DBP for cardiovascular risk varies by age group. SBP is more predictive of cardiovascular risk in individuals older than 60 years, whereas DBP is more predictive among those younger than 50 years; in individuals between 50 and 60 years of age, both SBP and DBP have equal predictability.8 This phenomenon is due to the high prevalence of isolated systolic hypertension in the elderly. SBP tends to rise more than DBP with aging and arterial stiffness, resulting in a widened pulse pressure.
Hypertension along with tobacco use and diabetes mellitus is a major risk factor for PAD. It is strongly implicated in the pathogenesis of PAD, and accordingly these patients have a high prevalence of hypertension. Quantifying the risk of PAD among hypertensives in part depends on the manner in which investigators define PAD. Data from the Framingham study, in which PAD was defined by intermittent claudication, demonstrated that risk for PAD increases with increasing SBP and DBP in both men and women.9 Subsequently, the Framingham study 38-year follow-up data indicated that in both men and women, hypertension is associated with a more than twofold increased risk for PAD as manifested by intermittent claudication.10 A stronger association exists between PAD and SBP than between PAD and DBP. The NHANES, which also used intermittent claudication to define PAD, found that both untreated hypertension and treated but uncontrolled hypertension are associated with PAD, particularly among the elderly.7 Data from studies that use intermittent claudication as the criterion to define PAD must be weighed with caution as it is now known that many patients with PAD as defined by ABI of less than 0.9 do not have classic symptoms associated with intermittent claudication.11
Other studies define PAD according to ABI measurement. Traditionally, an ABI below 0.9 is considered diagnostic of PAD; however, some studies have more conservative criteria, using ABI of less than 0.80 or less than 0.75. Data from NHANES found that among adults older than 40 years, hypertension was strongly associated with prevalent PAD (ABI < 0.9).12 The Cardiovascular Heart Study demonstrated an inverse relationship between ABI and hypertension.13 In this study, hypertension was defined as a blood pressure higher than 160/90 mm Hg or self-reported use of antihypertensives. After adjustment for confounders, a strong inverse relationship persisted for ABI and SBP but not for DBP. With use of ABI as the criterion for PAD in the Rotterdam Study, the prevalence of hypertension (>160/95 mg Hg or use of antihypertensive medications) was 60% for both men and women.14
Unfortunately, hypertension tends to be undertreated in patients with PAD compared with patients with other forms of cardiovascular disease.15 Many patients with PAD are often hypertensive at the time of diagnosis. In the Peripheral Arterial Disease Awareness, Risk and Treatment: New Resources for Survival (PARTNERS) trial, 35% to 55% of PAD patients were hypertensive at the time of presentation.16 The concurrence of hypertension and PAD is associated with an increased risk for cardiovascular disease events.17 Conversely, hypertension is associated with PAD progression. In a study of patients with PAD observed over time, SBP and smoking were associated with disease progression defined by change in ABI or clinical events during a 4-year period.18
Renal artery stenosis, a secondary form of hypertension, is prevalent among patients with PAD and hypertension. In a series of patients with PAD undergoing digital subtraction angiography, 33% had renal artery stenosis; in 10%, stenosis was greater than 60%.19 This is an important consideration in determining the cause of hypertension in PAD and for subsequent blood pressure management.
In summary, hypertension is prevalent in the population as a whole. It is a major risk for atherosclerotic diseases, such as PAD. Therefore, identification of hypertension is important because, if it is untreated, the associated risk of cardiovascular disease events increases.
Diagnosis
Definition
Epidemiologic studies and therapeutic trials have often used different criteria to define hypertension in populations. As the eighth report (JNC 8) of the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure is currently still under review and yet to be released, current guidelines for hypertension diagnosis and management are based on the JNC 7 report.20 The JNC 7 defines hypertension as blood pressure higher than 140/90 mm Hg based on the average of two or more properly measured, seated blood pressure readings at each of two or more office visits.
The JNC 7 report also states that individuals with SBP of 120 to 139 mm Hg or DBP of 80 to 89 mm Hg should be considered prehypertensive and require health-promoting lifestyle modifications to prevent cardiovascular disease. In persons older than 50 years, SBP higher than 140 mm Hg is a much more important cardiovascular disease risk factor than DBP. The presence of hypertension is classified by JNC 7 as stage 1 or stage 2 (Table 30-1).
Table 30-1
JNC 7 Definition of Hypertension
| Stage | Systolic (mm Hg) | Diastolic (mm Hg) |
| Normal blood pressure | <120 | <80 |
| Prehypertension | 120 to 139 | >80 to 89 |
| Stage 1 hypertension | 140 to 159 | >90 to 99 |
| Stage 2 hypertension | >160 | >100 |
JNC 7, Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Blood Pressure Measurement Technique
Routine blood pressure measurements should be made with an appropriate-sized cuff to ensure accuracy. At least two measurements should be made. The patient should be seated comfortably, with feet on the floor and back supported, for at least 5 minutes in a quiet room before measurements are taken. The arm should be supported at the level of the heart. Ideally, patients should be free of caffeine and smoking 30 minutes before measurements are taken.
Ambulatory blood pressure monitoring is another technique that can be used to verify the diagnosis of hypertension in certain situations. Ambulatory blood pressure monitoring can be used to identify hypertension, masked hypertension, normotension, and white coat hypertension. In addition to suspected cases of white coat hypertension, JNC 7 recommends ambulatory blood pressure monitoring for resistant hypertension (uncontrolled blood pressure despite adequate doses of three drugs including a diuretic), episodic hypertension, autonomic dysfunction, and symptoms of orthostasis in those receiving therapy.
Hypertension, according to ambulatory blood pressure monitoring measurements, is a 24-hour average higher than 130/80 mm Hg or daytime average higher than 140/85 mm Hg.21 White coat hypertension is defined as elevated office blood pressures compared with blood pressures obtained in ambulatory settings. Although initially thought to be a benign condition, white coat hypertension is now believed to carry an increased risk for cardiovascular events compared with normotension.22 Although major guidelines do not address this group, practitioners should evaluate these patients for evidence of target organ damage and counsel about lifestyle modification. Finally, masked hypertension occurs when patients are normotensive in the office setting but with elevated outpatient readings. These individuals, often discovered as a result of participation research studies, may have increased risk for cardiovascular events compared with normotensives.23
Secondary Causes
Patients with resistant hypertension, as defined before, should be evaluated first with a careful history, with particular attention to use of exogenous substances that may lead to elevations in blood pressure (e.g., corticosteroids, weight loss supplements, herbal medication, nonsteroidal anti-inflammatory drugs). Next, the patient’s medications should be reviewed to ensure that adequate doses are being used (regimen should include a diuretic) and that the patient is taking all medications as directed. If these are unrevealing, the patient should be evaluated for secondary causes of hypertension. Patients, such as the elderly, may have pseudohypertension, in which calcified vessels produce falsely elevated blood pressure readings. These individuals may report orthostasis with antihypertensive therapy, have palpable rigid vessels, and lack other evidence of target organ damage.
Once the diagnosis of hypertension has been established, an evaluation for secondary causes that are potentially curable should be done (Table 30-2). The evaluation of secondary causes of hypertension is reviewed elsewhere.24 The physical examination of patients with hypertension should include auscultation for the presence of an abdominal bruit, palpation for an aneurysm, and palpation of the arteries of the limbs for PAD. The initial evaluation of the patient with hypertension should include a complete blood count; chemistry panel, which includes blood urea nitrogen, glucose, calcium, creatinine, and electrolyte determinations; and a fasting lipid profile. A uric acid level is also recommended, especially for patients who may undergo diuretic therapy as this class of medication may result in hyperuricemia. A urinalysis should also be routinely obtained, especially in the diabetic patient who may have microalbuminuria as an early manifestation of nephropathy. Microalbuminuria is also a known risk factor for atherosclerotic disease. Plasma renin activity is not necessary unless the patient is thought to have primary hyperaldosteronism as may be suggested by hypokalemia.
Table 30-2
Secondary Causes of Hypertension
| Cause | Signs and Symptoms |
| Primary aldosteronism | Hypokalemia |
| Cushing’s syndrome | Striae, abdominal obesity |
| Pheochromocytoma | Labile blood pressure, tachycardia, sweats, headaches |
| Renal artery stenosis (atherosclerotic or due to fibromuscular dysplasia) | Smoking history, flash pulmonary edema, abdominal bruits |
| Thyroid disease | Goiter |
| Oral contraceptive pills | Women of childbearing age |
| Obstructive sleep apnea | Snoring |
| Coarctation of the aorta | Children, disparate blood pressures in upper and lower extremities |
| Kidney disease | Elevated serum creatinine, proteinuria |
Pathologic Mechanisms of Hypertension and Atherosclerosis
The pathologic influence of hypertension on the development of atherosclerosis is clear but the molecular mechanisms involved remain uncertain, probably because of the complex nature of atherosclerosis. The genetic makeup of the individual, behavioral tendencies (e.g., smoking), and environmental influences all shape the risk for atherosclerotic plaque development.
Animal Models of Hypertension
Genetically engineered mouse models have given insight into the complex interaction of blood pressure and atherogenesis. Most mouse models of hypertension exhibited increased atherosclerotic lesion size, although there are some exceptions.25 In addition, there are several reports of reduction in blood pressure resulting in reduced atherosclerosis.25 However, there are studies demonstrating that atherosclerosis can be altered in hypertensive mice without significant lowering of blood pressure.25 Therefore, the stimulus for hypertension, for example, activation of the renin-angiotensin system, may be as important as the severity of hypertension for development of atherosclerosis.
Renin-Angiotensin System and Atherosclerosis
One of the strongest correlations between blood pressure and atherosclerosis is perturbation in the renin-angiotensin system. This hormonal system is responsible for homeostatic control of arterial pressure, tissue perfusion, and extracellular volume. The juxtaglomerular cells located in each nephron produce renin, which converts angiotensinogen (produced mainly in the liver) to angiotensin I. Angiotensin-converting enzyme (ACE) converts angiotensin I into angiotensin II, which is a potent vasoconstrictor and mediator of aldosterone secretion. Studies of hyperlipidemic mice in which angiotensin II was chronically infused showed promotion of atherosclerosis independent of changes in arterial blood pressure.26 Furthermore, several studies showed that pharmacologic inhibition of the renin-angiotensin system reduces the development of atherosclerosis independently of blood pressure reduction.25
A pathologic interaction between hypercholesterolemia and hypertension has recently emerged. One study evident of this maladaptive relationship involved the administration of angiotensin II to men with normocholesterolemia and to men with hypercholesterolemia. The blood pressure response to angiotensin II was exaggerated in the hypercholesterolemia group, and this response was blunted by cholesterol reduction.27 Studies in animals indicate that the combination of renin-angiotensin inhibition and statin significantly reduces atherosclerosis compared with renin-angiotensin inhibition alone, probably through ablation of inflammatory signals.28 The results from randomized trials in human subjects confirm the antihypertensive effect seen in animals. A study of 41 patients taking medication for hypertension was conducted whereby patients were randomized to statin versus dietary control. After 3 months, the statin group had a greater reduction in blood pressure compared with the control group.29 Some data suggest that statins may also have a salutary effect on vascular elasticity.28
Endothelial Dysfunction and Hypertension
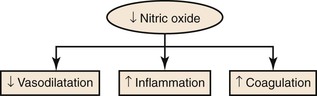
Endothelial dysfunction occurs early in the atherosclerotic process, and hypertension is associated with endothelial dysfunction in the coronary, renal, and peripheral circulation. Studies in animals and humans using an agonist-induced vasodilator response show that this response is blunted in the setting of hypertension.30 One key molecule, partially responsible for the vasodilator response and involved in maintaining normal endothelial function, is nitric oxide. A reduction in endothelium-derived nitric oxide may result in not only a reduced vasodilator response but also a proinflammatory, prothrombotic, and procoagulant phenotype (Fig. 30-2). The genetic deletion of endothelial nitric oxide synthase, the enzyme necessary for generating nitric oxide, resulted in significantly increased SBP (128 ± 3 vs 108 ± 5 mm Hg; P < .001) and decreased heart rate (531 ± 22 vs 629 ± 18 beats/minute; P < .001) compared with wild-type controls.31 Although it seems clear that endothelial dysfunction is a consequence of hypertension, the data regarding endothelial dysfunction as a precursor to hypertension are mixed. One study in the offspring of essential hypertension patients evaluating forearm blood vessel vasodilatation with acetylcholine found a blunted response compared with those without a family history of hypertension.32 Another more recent study evaluating flow-mediated vasodilatation of the brachial artery did not discern a difference between offspring of hypertensive patients and those without family history.33 More research is needed to identify those subjects predisposed to development of hypertension.
Renovascular Hypertension
Renal artery stenosis is most commonly due to atherosclerotic disease and may lead to renovascular hypertension. The consequence of the reduction in blood flow to the kidney is activation of the renin-angiotensin-aldosterone system and possibly ischemic nephropathy. One hypothesis proposed that some of the humoral factors activated by the renal artery stenosis may accelerate the atherosclerotic process.34 Experimental studies of pigs with hypertension secondary to renal artery stenosis showed that increased oxidative stress resulted from this condition and was a stimulus for atherosclerosis independent of cholesterol levels.35 Clinical evidence is also supportive of this hypothesis, which may explain the relatively high prevalence of renal artery stenosis in individuals with cardiovascular disease in other arterial territories.
Management
The goals for treatment of hypertension are to lower blood pressure and to reduce cardiovascular disease risk and atherosclerosis progression.
General Principles
Effective therapy for hypertension usually involves a combination of lifestyle modifications and pharmacotherapy.
Lifestyle Modifications
Lifestyle modifications have been demonstrated to reduce blood pressure and to lower cardiovascular disease risk.36 Depending on the individual, lifestyle modifications can reduce blood pressure by 2 to 20 mm Hg.37 The benefits of various lifestyle modifications can improve health beyond just the effects of blood pressure lowering. The lifestyle modifications that most major medical societies recommend as a part of standard treatment for hypertension include weight loss, limiting dietary sodium, engaging in aerobic physical activity for at least 30 minutes daily most days of the week, and limiting alcohol intake to one or two servings daily. The Dietary Approaches to Stop Hypertension (DASH) eating plan is one example of a low-fat and low-sodium diet rich in fruits and vegetables that has been demonstrated to effectively lower blood pressure.38
Antihypertensive Therapy
Cardiovascular risk increases progressively with increasing blood pressure beginning at 110/75 mm Hg.37 Clinical trials have confirmed the benefit of antihypertensive therapy in reducing cardiovascular complications by lowering blood pressure.39,40 The same benefits of antihypertensive therapy protection against cardiovascular events have been demonstrated in patients with PAD. The subset of patients with PAD, defined by an ABI below 0.9, enrolled in the Heart Outcomes Prevention Evaluation (HOPE) study saw a reduction in cardiovascular events when they were treated with an ACE inhibitor, ramipril.41 In the Appropriate Blood Pressure Control in Diabetes (ABCD) trial, patients with diabetes were randomized to receive either intensive (average SBP, 128 mm Hg) or moderate (average SBP, 137 mm Hg) blood pressure control to determine effects on the rate of ischemic cardiovascular events. The subset of patients enrolled with PAD, determined by ABI, saw a reduction in cardiovascular events when they were subjected to intensive blood pressure control.42
Whereas antihypertensive therapy attenuates cardiovascular disease risk in patients with PAD, there are no data that it alters the course of the disease process. In the United Kingdom Prospective Diabetes Study Group (UKPDS) trial, tight blood pressure control in patients with diabetes and hypertension was associated with reductions in death and stroke but no decrease in risk of incident PAD.43 However, there is some recent evidence that walking times in patients with PAD and intermittent claudication are improved with ACE inhibitors.44,45
The American College of Cardiology and the American Heart Association recommend a blood pressure goal for patients with PAD of less than 140/90 mm Hg.46 Similarly, the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC-II) recommends a goal blood pressure of less than 140/90 mm Hg.47 Patients with diabetes or chronic kidney disease should be treated to a goal blood pressure of less than 130/80 mm Hg.46
Pharmacotherapy
General Considerations
Patients with prehypertension (>120-139/80-89 mm Hg) should be counseled about lifestyle modification, given their high risk for progression to overt hypertension. Guidelines suggest that medications are not indicated for this group; however, a study demonstrated potential benefits of angiotensin receptor blocker (ARB) therapy in patients with prehypertension.48
For patients unable to reach blood pressure goals with lifestyle modifications alone or if target organ damage is evident, medications should be instituted for hypertension management. Thiazide diuretics are considered first-line therapy for most patients with uncomplicated hypertension. If blood pressure is more than 20/10 mm Hg above target at presentation, combination therapy with at least two agents should be initiated. Consideration should be given to fixed-dose combination pills to improve patient adherence. After a thiazide diuretic, the next choice of drug therapy depends on the presence or absence of other comorbid conditions. In cases of uncomplicated hypertension, an ACE inhibitor, ARB, beta blocker, or calcium channel blocker can be used with a thiazide diuretic. For the hypertensive patient with comorbid conditions, a second drug may be chosen for its specific benefits in certain subgroups of patients. For example, patients with chronic kidney disease and diabetes mellitus are known to benefit from ACE inhibitor or ARB therapy. Patients with coronary artery disease or heart failure are known to benefit from beta blockers.
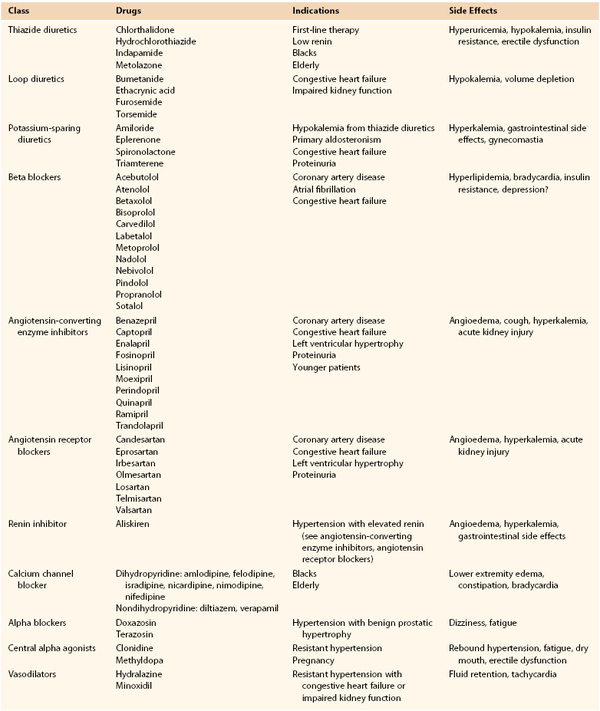
As no antihypertensive therapy has demonstrated specific benefits for PAD,49 medication should be chosen on the basis of the patient’s other cardiovascular disease risk factors (e.g., chronic kidney disease with proteinuria, coronary artery disease, diabetes, or heart failure). Agents in the following classes of antihypertensives have various benefits for particular patient populations (Table 30-3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree