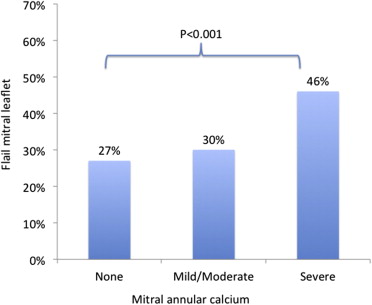
The aim of this study was to assess the association between mitral annular calcium (MAC) and flail mitral leaflets in a cohort of patients with degenerative mitral valve disease. A retrospective study was conducted of consecutive patients with degenerative mitral valve disease who underwent echocardiography at Rabin Medical Center from 2003 to 2012. Special focus was attended to the presence and grade of MAC and characterization of valve pathology (myxomatous vs nonmyxomatous, prolapse vs flail). Patients were excluded if they had undergone previous mitral valve surgery and/or had infective endocarditis. Multivariate logistic regressions were used to control for confounders. The study included 1,912 patients (60.8% men, mean age 63.8 ± 17.4 years) divided into 3 groups: 1,627 (86%) without MAC, 183 (10%) with either mild or moderate MAC, and 94 (5%) with severe MAC. The presence of flail leaflet was 27%, 30%, and 46% in these groups, respectively (p <0.001). After adjustment for age, gender, and co-morbidities, the odd ratio for flail mitral leaflet with severe MAC versus no MAC was 1.76 (95% confidence interval 1.10 to 2.83, p = 0.019). In conclusion, this study demonstrates that degenerative mitral valve disease with severe MAC is significantly associated with flail mitral leaflet.
Mitral annular calcium (MAC) is common in the older population and has been regarded as a cardiac manifestation of atherosclerosis. However, MAC is also relatively frequent in younger patients with myxomatous mitral disease, in whom the assumed pathogenesis is dystrophic calcium deposits at sites of annular trauma, secondary to excess tension exerted by redundant hypermobile leaflets. Calcium deposits may extend beneath the annular plane and cause elevation of the mitral leaflets. Moreover, annular calcium deposits may reduce its flexibility and attenuate its dynamic change in shape throughout the cardiac cycle. These changes may potentially exert excess tension on the chords and predispose to their rupture. Thus, we aimed to assess the association between MAC and flail mitral valve in a population of patients with degenerative mitral valve disease.
Methods
The study group of patients with degenerative mitral valve disease was retrieved from Rabin Medical Center’s cardiac echocardiography database from 2003 to 2012. If patients underwent >1 echocardiographic studies, we obtained the data from the latest study. Demographic and clinical data (hypertension, diabetes, dyslipidemia, current or past smoking, and chronic renal failure, defined as glomerular filtration rate < 60 ml/min/1.73 m 2 for >3 months) were obtained from the electronic records. We excluded patients who underwent mitral valve surgery before the index echocardiographic study and patients with histories of infective endocarditis of the mitral valve or blunt trauma to the chest (to exclude flail leaflets from causes other than degenerative disease). The study protocol was approved by the Ethics Committee of Rabin Medical Center and was in accordance with the Declaration of Helsinki. All patients underwent full echocardiographic studies performed by a certified sonographer and interpreted by cardiologists with specialty in echocardiography (YS, DW, DM, AS, MV). The echocardiographic data were obtained with Philips Sonos 5500, 7500, and iE33 machines (Philips Medical Systems, Andover, Massachusetts). The diagnosis of degenerative mitral valve was made in the presence of either prolapse or flail leaflets. The diagnosis of flail mitral valve was based on the failure of leaflet coaptation with the tip of the involved leaflet protruding into the atrium and the presence of an eccentric regurgitation jet directed away from the flail leaflet. The estimation of mitral regurgitation grade was based on American Society of Echocardiography guidelines. The characterization of the valve as myxomatous was based on leaflet thickness and length in diastole. Mitral valve anatomy was classified as myxomatous when leaflet redundancy was present and nonmyxomatous (i.e., fibroelastic deficiency) when the leaflets appeared normal, except for the ruptured chordae and the flail segment.
MAC was defined as intense echogenic deposits, usually localized at the posterior mitral annulus but sometimes involving the entire annulus. Severe MAC was defined as thickened echogenic annulus ≥5 mm (from the leading anterior to the trailing posterior edge at its greatest width). Less severe MAC was considered mild or moderate MAC.
Continuous variables are expressed as mean ± SD, median (interquartile range), and ranges. Normality of distribution was evaluated using histograms and Q-Q plots. Categorical variables are expressed as frequencies and percentages. Spearman’s rank correlation coefficients were used to describe the relation between mitral regurgitation grade and MAC severity. Continuous variables were compared between groups using Mann-Whitney U tests or Kruskal-Wallis tests. Categorical variables were compared between groups using chi-square tests. Univariate logistic regression was used to evaluate the crude association between flail mitral valve and MAC severity and multivariate logistic regression to evaluate the relation adjusted for age and gender. We used additional block with backward stepwise likelihood ratio method to identify potential confounders (hypertension, diabetes, dyslipidemia, current or past smoking and chronic renal failure). Analyses were performed using SPSS version 20 (SPSS, Inc., Chicago, Illinois). All statistical analyses were 2 tailed. Statistical significance was set at p <0.05.
Results
The study included 1,912 patients; the mean age was 63 ± 13 years, and 61% were men. Data on co-morbidities were available for 1,542 patients. The clinical and echocardiographic characteristics of the study group, divided according to the presence of flail leaflet or the severity of MAC, are listed in Tables 1 and 2 , respectively.
| Variable | Total (N=1912) | Flail mitral valve | P value | |
|---|---|---|---|---|
| No (n=1371) | Yes (n=541) | |||
| Age, ±SD (years) | 63±16 | 61.6±18.3 | 69.5±13.4 | <0.001 |
| Female | 40% | 43% | 28% | <0.001 |
| Hypertension | 42% | 39% | 51% | <0.001 |
| Dyslipidemia | 35% | 32% | 42% | <0.001 |
| Diabetes Mellitus | 13% | 12% | 14% | 0.49 |
| Smoker | 16% | 15% | 19% | 0.07 |
| Chronic renal failure | 8% | 7% | 11% | 0.03 |
| Mitral Regurgitation: | <0.001 | |||
| None | 15% | 21% | 0% | |
| Mild | 32% | 44% | 1% | |
| Moderate | 27% | 26% | 31% | |
| Severe | 25% | 10% | 67% | |
| MAC: | <0.001 | |||
| None | 86% | 87% | 82% | |
| Mild- moderate | 10% | 9% | 10% | |
| Severe | 5% | 4% | 8% | |
| Myxomatous degeneration | 33% | 32% | 34% | 0.53 |
| Variable | Total (N=1912) | MAC severity | P value | ||
|---|---|---|---|---|---|
| None (n=1627) | Mild- mod (n=183) | Severe (n=94) | |||
| Age, ±SD (years) | 63±16 | 61.6±17.5 | 75.2±10.6 | 80.5±7.4 | <0.001 |
| Female | 39% | 38% | 38% | 71% | <0.001 |
| Hypertension | 42% | 39% | 55% | 64% | <0.001 |
| Dyslipidemia | 35% | 32% | 50% | 45% | <0.001 |
| Diabetes Mellitus | 13% | 11% | 18% | 24% | 0.49 |
| Smoker | 16% | 16% | 17% | 12% | 0.07 |
| Chronic Renal Failure | 8% | 8% | 10% | 13% | 0.03 |
| Mitral Regurgitation: | <0.001 | ||||
| None | 15% | 17% | 6% | 2% | |
| Mild | 32% | 33% | 32% | 14% | |
| Moderate | 27% | 26% | 31% | 48% | |
| Severe | 25% | 24% | 31% | 35% | |
| Flail leaflet | 28% | 27% | 30% | 46% | <0.001 |
| Myxomatous degeneration | 33% | 34% | 32% | 19% | 0.53 |
The prevalence of flail mitral leaflet was 27% in patients without MAC, 30% in patients with mild or moderate MAC, and 46% in patients with severe MAC (p <0.001) ( Figure 1 ). After adjusting for age, gender, and co-morbidities, the odds ratio for flail mitral leaflet in patients with severe MAC compared with patients with no MAC was 1.76 (95% confidence interval 1.10 to 2.83); see Table 3 .
| MAC severity | OR (95% CI) to flail mitral valve | P value | |
|---|---|---|---|
| Crude data | None | 1 | 0.001 |
| Mild – moderate | 1.13 (0.81-1.58) | 0.49 | |
| Severe | 2.27 (1.49-3.45) | <0.001 | |
| Age and sex adjusted | None | 1 | 0.008 |
| Mild- moderate | 0.80 (0.56-1.13) | 0.2 | |
| Severe | 1.8 (1.17-2.87) | 0.008 | |
| Co-morbidities adjusted | None | 1 | 0.03 |
| Mild- moderate | 0.85 (0.59-1.22) | 0.38 | |
| Severe | 1.76 (1.10-2.83) | 0.019 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


