As the number of Hodgkin’s lymphoma (HL) survivors grows, understanding long-term complications becomes more important. Mediastinal radiotherapy (MRT) seems to cause valvular disease, and the prevalence might increase during follow-up. In this cross-sectional study 82 HL survivors participated (52% men, mean age 47.8 years, 50 treated with MRT). Valvular disease was diagnosed by transthoracic echocardiography and compared between HL survivors treated with and without MRT. Univariate and multivariate logistic regression analysis was used to identify predictors for valvular disease. During a median follow-up of 13.4 years (range 2 to 39 years), ≥ mild valvular disease was present in 61.2% of HL survivors with MRT (n = 30), compared with 31.0% of HL survivors without MRT (n = 9; odds ratio [OR] 3.51, 95% CI 1.32 to 9.30, p = 0.01). In multivariate analysis, only current age remained predictive for ≥ mild valvular disease (OR 1.08 per year, 95% CI 1.01 to 1.14, p = 0.023). Aortic regurgitation (AR) was most prevalent and irradiated patients had significantly more ≥ mild AR (38.2% vs 6.8%, p = 0.007). Within the MRT subgroup, time after radiation of >15 years was associated with AR (OR 4.70, 95% CI 1.05 to 21.03, p = 0.043), after adjusting for current age and hypertension. Severe valvular disease was present in 24.5% of HL survivors with MRT compared with 3.4% without MRT (p = 0.016). Valvular surgery was performed in 9 HL survivors (18.0%) with MRT and in none without MRT. In conclusion, the prevalence of valvular disease in HL survivors treated with MRT is high and increases with time after irradiation. Long-time screening for valvular disease by transthoracic echocardiography might be worthwhile.
Of all cancers diagnosed in the developed world, Hodgkin’s lymphoma (HL) accounts for approximately 0.6%, with about 8,220 new cases in the United States annually and with an incidence peak in young adulthood. Improved treatment modalities with radiotherapy (RT) and chemotherapy (alone or combined) has led to improved disease-specific survival with cure rates of circa 80%. For these reasons, the number of HL survivors grows and understanding long-term complications becomes more important. Potential long-term cardiac adverse effects of mediastinal RT (MRT) include valvular disease, pericarditis, coronary artery disease, and cardiomyopathy, which might eventually lead to increased mortality. There appears to be a strong association between time after MRT and prevalence of cardiac disease, implicating that radiation-associated cardiovascular toxicity may be progressive. HL survivors, who are relatively young and survive for long periods, are therefore at increased risk. However, the course is often asymptomatic and symptoms can be misinterpreted. Most prevalent radiation-associated noncoronary cardiac disease is valvular disease. Previous studies report differently on the prevalence, whereas it also remains challenging to identify which HL survivors are susceptible. This study aims to assess the prevalence and clinical determinants of (asymptomatic) valvular disease in HL survivors who underwent MRT. Knowledge of these determinants is a prerequisite for developing appropriate follow-up and screening programs.
Methods
All HL survivors remaining in hematological remission registered at our institution with a follow-up of at least 2 years after the initial diagnosis were invited to participate (n = 113). From November 2007 to August 2008, 82 HL survivors could be included. Nineteen HL survivors died, with a known cause of death in 11 patients (7 secondary malignancies, 3 cardiovascular complications, and 1 infectious complication). Six patients could not be traced because they did not attend regular checkups and another 6 reduced participation (3 because of old age, 1 because of long traveling distance, and 2 without specific reason). The institutional review committee approved this study. All participating subjects gave informed consent.
Patients were treated from 1969 to 2005 with different regimens. Until the late 1990s, typically extended field RT (mostly mantle field RT to neck, mediastinum, axillary lymph nodes, and paraaortic lymph nodes) was performed in patients with limited stage HL, being replaced by involved field radiation in the more recently treated patients. Patients with more advanced stages of disease were primarily treated with chemotherapy, to which RT was added in case of bulky disease, mostly located in the mediastinum. Until the 1980s, chemotherapy consisted mainly of MOPP (mechlorethamine, vincristine, procarbazine, and prednisone). Afterward, anthracycline-containing regimens such as ABVD (doxorubin, bleomycin, vinblastine, and dacarbazine) became part of the primary treatment.
Major risk factors for development of cardiac disease were recorded for each patient. Hypertension was defined as systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg at 3 different measuring points or the current use of antihypertensive medication. Dyslipidemia was defined as total cholesterol >5.0 mmol/L/or high-density lipoprotein cholesterol <1.0 mmol/L or low-density lipoprotein cholesterol >3.0 mmol/L/or triglycerides >1.7 mmol/L.
Two-dimensional transthoracic echocardiography, Doppler (color, pulsed wave, and continuous wave) studies were obtained using the Philips IE33 ultrasound scanner. Two independent experienced echocardiographers, who were blinded to patient and treatment details, interpreted the echocardiographic studies. Valve regurgitation and stenosis were assessed using guidelines of the European Association of Echocardiography.
To evaluate valvular heart disease of MRT, the group was divided in patients who received mediastinal RT and in patients who did not. Because of the assumed association between time after irradiation and valvular heart disease, prevalence was also assessed in irradiated patients grouped by number of years between irradiation and cardiac examination (2 to 10 years, 11 to 20 years, and >20 years).
For analysis of valvular disease patients were categorized into 2 groups on the basis of severity: none or trace versus more than or equal to mild (≥ mild) valvular disease. HL survivors who underwent valvular surgery were scored according to the degree of severity of valvular disease before surgery.
Data were expressed as mean/median with SDs/range or as percentages. Comparisons of means and medians were performed using the Student t test and the Mann–Whitney test respectively, whereas differences in proportions were evaluated by the chi-square test. In the irradiated group, clinical variables possibly associated with valvular heart disease were assessed using regression models. If outcome variables were categorical, logistic regression was performed and results were expressed as odds ratio (OR) and 95% CIs. If outcome variables were continuous, linear regression models were used and results were expressed as regression coefficients and 95% CI. For all outcomes, univariate analysis was performed first, after which significant findings were assessed in a multivariate model. Variables used in univariate analysis were current age, gender, body mass index, smoking, diabetes, dyslipidemia, hypertension, age at diagnosis, time after treatment, irradiation dose (<40/≥40 Gy), treatment containing chemotherapy, and anthracycline-containing chemotherapy. In univariate analysis, time after treatment was used as a continuous variable. If this parameter showed a significant univariate association and remained predictive in multivariate analysis, we searched for the optimal cut-off value for this variable. All analyses were performed using IBM SPSS Statistics, version 21. A 2-tailed p value < 0.05 was considered statistically significant.
Results
Fifty of 82 HL survivors were treated with MRT. Patient characteristics are listed in Table 1 . Participants ranged in age from 24 to 79 years and time because MRT varied from 4 to 39 years. Subjects in the irradiated group were about 9 years younger at diagnosis and received treatment approximately 8 years earlier. Most of irradiated HL survivors (70%) were treated with a radiation dose of 40 Gy or higher.
| Variable | MRT (n=50) | No MRT (n=32) | P-value |
|---|---|---|---|
| Current age (years) | 48 ± 14 | 48 ± 12 | 0.870 |
| Men | 52% | 59% | 0.513 |
| Body mass index (kg/m 2 ) | 24.7 ± 4.3 | 27.7 ± 4.2 | 0.002 |
| Positive family history of CVD | 30% | 16% | 0.139 |
| Smoker (pack years) | 4.6 ± 10.1 | 11.9 ± 17.7 | 0.021 |
| Diabetes mellitus | 4.2% | 0% | 0.250 |
| Dyslipidemia | 72% | 72% | 0.990 |
| NT-proBNP (pg/ml) | 155 (27-3633) | 45 (9-3270) | 0.001 |
| Hypertension | 28% | 28% | 0.990 |
| Age at diagnosis (years) | 30 ± 13 | 39 ± 14 | 0.003 |
| Time after treatment (years) | 16.5 ± 8.5 | 8.1 ± 6.5 | 0.000 |
| Mediastinal irradiation dose (Gy) | 40 (28-44) | – | – |
| Chemotherapy | 70% | 97% | 0.003 |
| Anthracycline chemotherapy | 52% | 84% | 0.192 |
In the total group of HL survivors, ≥ mild valvular disease was present in 39 of all patients (47.6%) with a total of 65 valves involved (24 aortic, 24 mitral, 11 tricuspid, and 6 pulmonary).
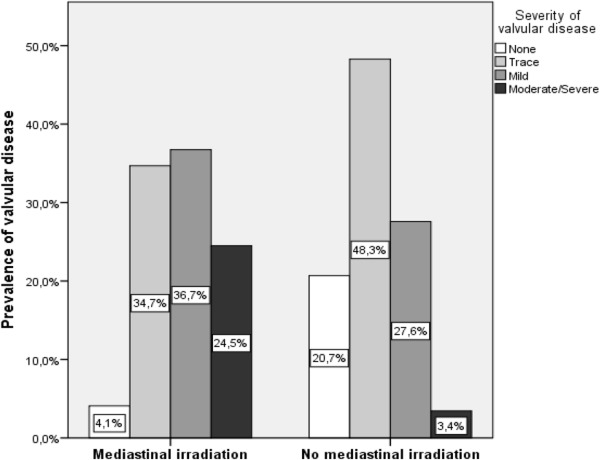
Valvular disease was more prevalent in irradiated patients ( Figure 1 ). In total, ≥ mild valvular disease was present in 61.2% of HL survivors with MRT (n = 30), compared to 31.0% of HL survivors without MRT (n = 9) with an OR 3.51 (95% CI 1.32 to 9.30, p = 0.01). The degree of severity of valvular dysfunction for separate valves is listed in Table 2 . Left-sided valvular regurgitation was most prevalent in HL survivors with MRT compared to nonirradiated HL survivors, ≥ mild aortic regurgitation (AR) in 38.2% versus 6.8% (OR 8.55, 95% CI 1.82 to 40.16, p = 0.007) and ≥ mild mitral regurgitation (MR) in 36.7% versus 17.2% (OR 2.8, 95% CI 0.91 to 8.59, p = 0.074), respectively. Mild or greater tricuspid regurgitation (TR) was found in 20.4% (n = 10) of HL survivors treated with MRT, compared to 3.4% (n = 1) HL survivors treated without MRT (OR 7.37, 95% CI 0.89 to 60.95, p = 0.064). Mild or greater aortic stenosis (AS) was found in 16.3% (n = 8) of HL survivors treated with MRT, compared to 6.9% (n = 2) HL survivors treated without MRT (OR 2.63, 95% CI 0.52 to 13.4, p = 0.242). For mitral stenosis (MS), a comparison between the 2 subgroups could not be made because ≥ mild MS did not occur in nonirradiated HL survivors. For all types of valvular disease, prevalence and degree of severity are highest in the group treated more than 20 years before evaluation.
| Echocardiographic finding | HL survivors with MRT | No MRT | p-value ∗ | |||
|---|---|---|---|---|---|---|
| All patients n=49 | Years following irradiation | All patients n=29 | ||||
| 2-10 years n=13 | 11-20 years n=21 | >20 years n=15 | ||||
| Aortic regurgitation | 0.007 | |||||
| None | 24 (48%) | 10 (77%) | 11 (52%) | 3 (20%) | 26 (90%) | |
| Trace | 6 (12%) | 1 (8%) | 4 (19%) | 1 (7%) | 1 (3%) | |
| Mild | 13 (26%) | 2 (15%) | 4 (19%) | 7 (47%) | 1 (3%) | |
| Moderate/severe | 6 (12%) | 0 (0%) | 2 (10%) | 4 (27%) | 1 (3%) | |
| Mitral regurgitation | 0.074 | |||||
| None | 9 (18%) | 3 (23%) | 3 (14%) | 3 (20%) | 12 (41%) | |
| Trace | 22 (45%) | 5 (39%) | 11 (52%) | 6 (40%) | 12 (41%) | |
| Mild | 12 (25%) | 5 (39%) | 6 (29%) | 1 (7%) | 5 (17%) | |
| Moderate/severe | 6 (12%) | 0 (0%) | 1 (5%) | 5 (33%) | 0 (0%) | |
| Tricuspid regurgitation † | 0.068 | |||||
| None | 8 (16%) | 5 (39%) | 2 (10%) | 1 (7%) | 13 (45%) | |
| Trace | 30 (63%) | 8 (62%) | 14 (67%) | 8 (57%) | 15 (52%) | |
| Mild | 7 (15%) | 0 (0%) | 4 (19%) | 3 (21%) | 1 (3%) | |
| Moderate/severe | 3 (6%) | 0 (0%) | 1 (5%) | 2 (14%) | 0 (0%) | |
| Pulmonary regurgitation ‡ | 0.847 | |||||
| None | 23 (50%) | 6 (55%) | 8 (38%) | 9 (64%) | 18 (67%) | |
| Trace | 19 (41%) | 4 (36%) | 12 (57%) | 3 (21%) | 7 (26%) | |
| Mild | 4 (9%) | 1 (9%) | 1 (5%) | 2 (14%) | 2 (7%) | |
| Moderate/severe | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Aortic stenosis | 0.242 | |||||
| None | 41 (84%) | 12 (92%) | 20 (95%) | 9 (60%) | 27 (93%) | |
| Mild | 2 (4%) | 0 (0%) | 1 (5%) | 1 (7%) | 1 (3%) | |
| Moderate/severe | 6 (12%) | 1 (8%) | 0 (0%) | 5 (33%) | 1 (3%) | |
| Mitral stenosis | – | |||||
| None | 47 (96%) | 13 (100%) | 21 (100%) | 13 (87%) | 29 (100%) | |
| Mild | 1 (2%) | 0 (0%) | 0 (0%) | 1 (7%) | 0 (0%) | |
| Moderate/severe | 1 (2%) | 0 (0%) | 0 (0%) | 1 (7%) | 0 (0%) | |
∗ p Value for differences in ≥ mild valvular disorders between MRT and non-MRT group.
† Data for tricuspid regurgitation available for 48 subjects in MRT group (follow-up >20 years: 14 subjects).
‡ Data for pulmonary regurgitation available for 46 subjects in MRT group (follow-up 2 to 10 years: 11 subjects, >20 years: 14 subjects) and 27 subjects in non-MRT group. Percentages may not add up to 100% because of rounding.
Within the MRT group, clinical determinants of overall ≥ mild valvular disease were current age (OR 1.09 per year, 95% CI 1.03 to 1.17, p = 0.004) and time after treatment (OR 1.10 per year, 95% CI 1.01 to 1.21, p = 0.026). In multivariate analysis, only current age remained predictive for ≥ mild valvular disease (OR 1.08 per year, 95% CI 1.01 to 1.14, p = 0.023). Within the MRT group, AR could be predicted by current age, hypertension, and time after treatment using univariate analysis. In a multivariate model, only time after treatment remained associated with AR (OR 1.13 per year, 95% CI 1.01 to 1.26, p = 0.035). A significant cut-off point was found at 15 years after treatment: patients irradiated >15 years before evaluation showed a 4.70-fold increased odds for AR (95% CI 1.05 to 21.03, p = 0.043), adjusted for age and hypertension. For TR and AS: hypertension, time after treatment, and treatment containing chemotherapy proved to be predictive. Hypertension was also associated with pulmonary regurgitation. No clinical variables remained associated in multivariate analysis in these valvular lesions. For MR and MS, no significant predictors could be identified in univariate analysis in the MRT group ( Table 3 ).



