CHAPTER 6
Assessment of Stage C Patients with HF-rEF
“It is a capital mistake to theorize before one has data.”
—Sherlock Holmes (Sir Arthur Conan Doyle)1
The “3 Fs” of Ongoing Heart Failure Assessment
Care of a patient with Stage C heart failure requires repetition of a clinical cycle that includes assessment, initiation of a plan, and reassessment. New symptoms may fit the previous diagnosis of heart failure or herald new causes of heart failure or other disorders.
Fit: Do Findings Fit the Diagnosis of Heart Failure?
Even an experienced clinician can miss the diagnosis of heart failure. Preexisting chronic obstructive lung disease or renal insufficiency can obscure the cardiac etiology of shortness of breath or fatigue. In a young person, shortness of breath due to either cardiomyopathy or myocarditis is often attributed to asthma or pneumonitis. Conversely, recurrent symptoms may be attributed entirely to a previous heart failure diagnosis rather than an alternative new diagnosis.
Few patients have symptoms due to heart failure with a normal BNP, ECG, and chest x-ray. A chest x-ray may show cardiomegaly or bilateral pulmonary infiltrates consistent with edema (see Chapter 2).
ASSESSING THE HISTORY AND SYMPTOMS
The assessment of heart failure includes information from the standard components of medical diagnosis such as: cardinal symptoms, history, physical findings, and past medical history.
Cardinal Symptoms
The cardinal symptoms of heart failure are shortness of breath, fatigue, edema, or chest pain; although any of these may also be due to alternative etiologies. For each of these symptoms some common alternative etiologies also need to be considered (List 6.1).
LIST 6.1 Alternate Etiologies of Cardinal Heart Failure Symptoms 2
Shortness of Breath • Pulmonary • Anemia • Musculoskeletal • Functional | Fatigue • Anemia • Musculoskeletal • Metabolic • Functional |
Edema • Renal • Hepatic • Nutritional • Venous insufficiency • Obstruction of venous return | Chest Pain • Gastrointestinal • Pulmonary • Musculoskeletal • Functional |
In addition to the cardinal symptoms of heart failure, the clinician should be alert to less specific symptoms, especially in the elderly (List 6.2).
LIST 6.2 Less Specific Symptoms of Heart Failure
PAST MEDICAL HISTORY
Details of the past medical, family, and social history can be important in assessing heart failure. Key questions regarding the patient’s own medical history include:
1. Does the patient have previously known medical problems that could contribute to heart failure (List 6.3)?
2. Does the patient have risk factors for coronary artery disease, including hypertension, hyperlipidemia, smoking, and diabetes mellitus?
LIST 6.3 Pertinent Past Medical History for Heart Failure
FAMILY HISTORY
Key questions regarding the patient’s family history include:
1. Is there a family history of heart failure or coronary artery disease?
2. Is there a family history of early unexplained or sudden death?
SOCIAL HISTORY
Key questions regarding the patient’s family history include:
1. Is there a history of noncompliance with medications or diet?
2. Is alcohol use excessive?
3. Is there a history of illicit drug use?
4. Is there an adequate family or social support structure?
5. Has there been any unusual travel and/or exposure (e.g., toxins)?
PHYSICAL EXAM
Most individuals with ventricular dysfunction will appear completely comfortable at rest and with simple ambulation. Only with physical exertion or decompensated heart failure do patients appear overtly short of breath or fatigued.
Proper evaluation of vital signs is fundamental for assessment of heart failure syndromes. Each of the basic vital signs can have more than one etiology and the proper interpretation may guide a specific approach to heart failure. Tachycardia can represent compromised cardiac reserve at rest or arrhythmia mediating a cardiomyopathy; bradycardia can indicate medication effect, sinoatrial dysfunction, or AV node block. Hypertension may be the etiology of heart failure or identify a target for therapy; hypotension can imply intravascular depletion, pharmacologic effects, or profoundly low cardiac reserve. Tachypnea is consistent with pulmonary congestion, concomitant pulmonary disorders, or anemia. Fever may signal associated infection or active inflammatory myocarditis.
Beyond basic vital signs, the physical exam helps determine if a heart failure patient is “wet” (volume overloaded) or “dry” (intravascularly depleted). Criteria for “wet” include jugular venous neck distention, pulmonary rales, S3 gallop, abdominojugular reflux (AJR), hepatomegaly, and peripheral edema (Figure 6.1). Any of these findings can indicate elevated ventricular filling pressures, suggesting that the patient is “wet.” Physical exam findings that indicate intravascular depletion, suggesting that a patient is “dry,” include hypotension, an orthostatic decrease in blood pressure, or decreased skin turgor. More commonly, decreased intravascular volume is suggested by the findings of weight loss, a history of a gastrointestinal syndrome, or laboratory evidence of an increased ratio of blood urea nitrogen (BUN) to creatinine (Cr). Some clinicians supplement the cardiovascular physical exam with a bedside focused cardiac ultrasound.3
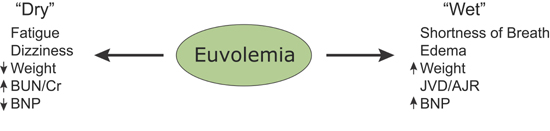
FIGURE 6.1 Assessing whether patients are “wet” or “dry”.
The volume status of a patient contributes to important cardiac abnormalities and specific physical exam findings are associated with each abnormality (List 6.4).
LIST 6.4 Cardiac Abnormalities and Associated Physical Exam Findings
Cardiac Abnormality | Physical Exam Sign |
Elevated cardiac filling pressures and fluid overload | • Elevated jugular venous pressure • S3 gallop • Rales • Abdominojugular reflux • Ascites • Edema |
Cardiac enlargement | • Laterally displaced or prominent apical impulse • Murmurs suggesting valvular dysfunction |
Reduced cardiac output | • Hypotension • Narrow pulse pressure • Cool extremities • Tachycardia with pulsus alternans |
Arrhythmia | • Irregular or rapid pulse suggestive of atrial fibrillation or frequent ectopy |
CLINICAL ESTIMATION OF HEMODYNAMICS IN HEART FAILURE
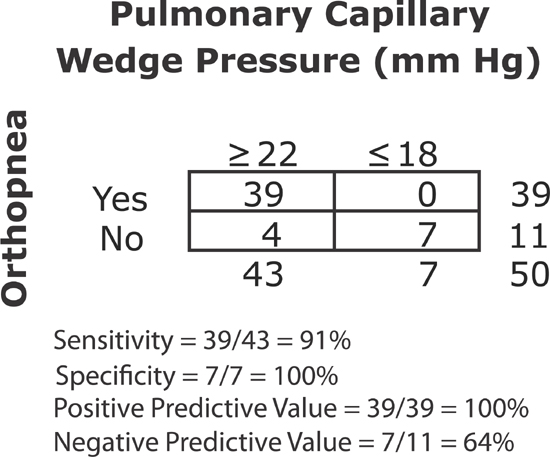
Stevenson and Perloff evaluated clinical factors to determine which might be useful to predict pulmonary capillary wedge pressure (PCWP) and cardiac output measured by right heart catheterization.4 Subjects were 50 patients with known HF-rEF who were being evaluated for heart transplant or adequacy of medical regimens. Orthopnea (a recent history of shortness of breath while patients were supine, requiring extra pillows) had a 91% sensitivity for being PCWP being ≥ 22 mm Hg (Figure 6.2). Physical exam findings of congestion were relatively insensitive to detect an elevated PCWP. Peripheral edema, neck vein distention, or rales were present in only 50% of patients with high wedge pressure. However, when any of these findings were present on physical exam, it was highly specific for a PCWP of ≥ 22 mm Hg.
FIGURE 6.2 Orthopnea as a clinical indicator of PCWP. Orthopnea was a sensitive specific predictor of a high PCWP in patients with known advanced heart failure.4
Stevenson and Perloff also found that the best discriminator for predicting a low cardiac index (≤ 2.2 L/min/m2) was a proportional pulse pressure (pulse pressure divided by the systolic pressure) less than or equal to 25% (Figure 6.3). Proportional pulse pressure and cardiac index also correlated in a linear relationship over a range of values.
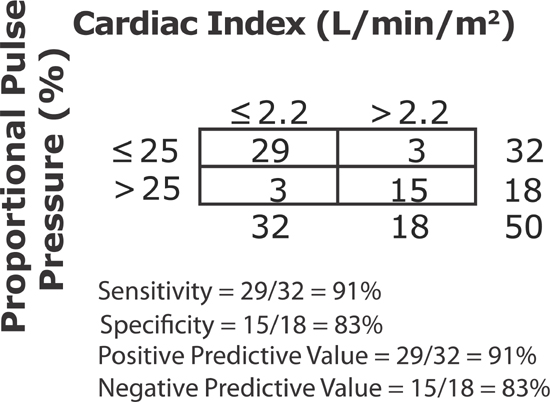
FIGURE 6.3 Proportional pulse pressure as a clinical indicator of low cardiac index. Proportional pulse pressure ([Systolic–Diastolic] / Systolic) less than or equal to 25% has an overall predictive accuracy of 88%.4
LABORATORY TESTS
Laboratory tests are part of the standard evaluation for heart failure and often have a particular relationship of abnormal findings to cardiac pathology (List 6.5).
LIST 6.5 Laboratory Tests in Heart Failure
ECG
Abnormalities are often present on resting ECG in patients with heart failure (Table 6.1).
TABLE 6.1 Corresponding ECG findings and suspected diagnoses.2
FINDINGS | SUSPECTED DIAGNOSIS |
Acute ST-T changes | Myocardial ischemia |
Atrial fibrillation, other tachyarrhythmia | Thyroid disease or heart failure due to rapid ventricular rate |
Bradyarrhythmias | Heart failure due to low heart rate/heart block |
Previous MI (e.g., Q waves) | Heart failure due to reduced left ventricular performance |
Low voltage | Pericardial effusion, amyloidosis |
Left ventricular hypertrophy | Diastolic dysfunction, hypertrophic cardiomyopathy |
CHEST X-RAY (CXR)
A chest x-ray provides information on 2 important questions that may support a diagnosis of heart failure depending on results of further investigation:
1. Are pulmonary infiltrates present?
• Edema?
• Other causes of dyspnea (i.e., fibrosis, pneumonia, inflammation)?
2. Is the cardiac silhouette enlarged? (Figure 6.4)
• Left ventricular dilation?
• Left ventricular hypertrophy?
• Right ventricular enlargement (may be present on lateral film only)?
• Pericardial effusion?
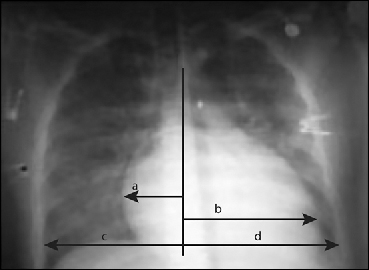
FIGURE 6.4 Chest x-ray demonstrating enlarged cardiac silhouette. Cardiac enlargement defined as (a + b/c + d > 0.5).5 Source: Adapted with permission from Jaski BE, Basics of Heart Failure. Springer Science + Business Media B.V.; 2000: 108.
An important caveat is that in the patient with chronic heart failure, a physical exam and chest x-ray can be free of findings of lung congestion despite a markedly elevated pulmonary capillary wedge pressure, as in Figure 6.4. This may relate to chronic enlargement of lung lymph vessels compensating for increased left heart filling pressures with increased return of interstitial edema to the venous system. Clear lung fields are also seen in isolated right heart failure.
Additional Testing Requirements
Because chest x-ray findings can be nonspecific, additional testing is often needed such as BNP, echocardiography, or (less often) right heart catheterization. BNP is usually elevated with ventricular dysfunction even in the absence of exam or chest x-ray abnormalities. If an empiric trial of diuretics leads to improvement, pulmonary congestion due to heart failure is the likely diagnosis, especially if abnormalities are present on the echocardiogram (see discussion of the second “F” for Function). Alternatively, when nonspecific interstitial infiltrates are present on chest x-ray, symptomatic patients may require either Doppler echocardiogram estimation or catheter measurement of pulmonary capillary wedge pressure to distinguish heart failure from pulmonary infection, inflammation, or fibrosis.
Function: Is Left Ventricular Systolic Function Abnormal by Echocardiography?
For some patients, when standard echocardiogram imaging is inadequate, alternative tests for measurement of left ventricular ejection fraction (EF) are available, such as contrast echocardiography, radio-nuclide ventriculography, cardiac magnetic resonance imaging (MRI), catheterization ventriculography, or cardiac computed tomography (CT). Echocardiography is the primary diagnostic test for determining systolic function (Figure 6.5).
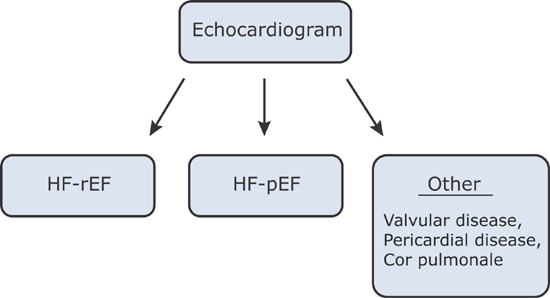
FIGURE 6.5 Echocardiography triage for cardiac function when heart failure is clinically suggested.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree